
In general, if you have Original Medicare and retiree insurance, Medicare will pay your health care bills first. In this case, your group coverage is your secondary insurance. Thus, it acts similar to a Medicare Supplement policy.
Full Answer
How does Medicare work after retirement?
How Does Medicare Work After Retirement? Is it mandatory? Medicare is a federal program that helps you pay for healthcare once you reach age 65 or if you have certain health conditions. You don’t have to sign up when you turn 65 years old if you continue working or have other coverage.
How does retiree insurance work?
Generally, when you have retiree coverage from an employer or union, they control this coverage. Employers aren't required to provide retiree coverage, and they can change benefits, premiums, or even cancel coverage. What's the cost and coverage?
What is the Medicare Retirement Age?
Medicare is a public health insurance program that you qualify for when you turn 65 years old. This might be retirement age for some people, but others choose to continue working for many reasons, both financial and personal.
Do retirees need all four parts of Medicare?
Many retirees wonder how to determine whether they need all four parts of Medicare. Questions about Medicare costs, supplemental insurances, and enrollment periods often arise as well. For Americans 65 and older, conversations about health insurance should include Medicare.
Do you automatically get Medicare when you retire?
If you retire and sign up for Social Security benefits before age 65, you'll automatically be enrolled in Parts A and B of Medicare when you turn 65.
When you retire do you keep your insurance?
"The most obvious insurance retirees need to maintain is health insurance," says Clark. The increasing cost of health care that comes with advanced age is a major reason to buy medical insurance. And since the implementation of the Affordable Care Act in 2014, the law requires virtually everyone to maintain coverage.
Can I keep my insurance if I have Medicare?
It is possible to have both private insurance and Medicare at the same time. When you have both, a process called “coordination of benefits” determines which insurance provider pays first. This provider is called the primary payer.
How much does Medicare cost if you are retired?
Medicare Part B is medical insurance. The monthly premium for Medicare Part B in 2022 is $170.10. That means that for the year 2022 you may pay $1,782 for Medicare's medical insurance for retirees....Health insurance for retirees: premiums.CoverageMonthly PremiumTotal Yearly Premium CostsMedicare Part B$170.10$1,7821 more row•Dec 30, 2021
What benefits do retirees get?
Benefits Eligibility.Medical Plans.Pharmacy Program.Dental Plans.Mental Health Resources.Retirement Savings.Life Events.Family Resources.More items...
What should you not do in retirement?
10 Things Not to Do When You RetireEnjoy, but Don't Be Undisciplined. ... Don't Immediately Downsize Your Home. ... Don't Blow Your Savings. ... Don't Neglect Your Estate Planning. ... Don't Expect Relationships to Remain Unchanged. ... Don't Be Afraid to Try New Things. ... Don't Let Loneliness Creep Into Your Life. ... Don't Neglect Your Appearance.More items...
Can you have Medicare and employer insurance at the same time?
Yes, you can have both Medicare and employer-provided health insurance. In most cases, you will become eligible for Medicare coverage when you turn 65, even if you are still working and enrolled in your employer's health plan.
Is Medicare Part A free at age 65?
You are eligible for premium-free Part A if you are age 65 or older and you or your spouse worked and paid Medicare taxes for at least 10 years. You can get Part A at age 65 without having to pay premiums if: You are receiving retirement benefits from Social Security or the Railroad Retirement Board.
What happens if you don't enroll in Medicare Part A at 65?
If you don't have to pay a Part A premium, you generally don't have to pay a Part A late enrollment penalty. The Part A penalty is 10% added to your monthly premium. You generally pay this extra amount for twice the number of years that you were eligible for Part A but not enrolled.
Is Medicare Part A and B free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
Why is Medicare Part B so expensive?
Why? According to CMS.gov, “The increase in the Part B premiums and deductible is largely due to rising spending on physician-administered drugs. These higher costs have a ripple effect and result in higher Part B premiums and deductible.”
How much do most seniors pay for Medicare?
Most people don't pay a monthly premium for Part A (sometimes called "premium-free Part A"). If you buy Part A, you'll pay up to $499 each month in 2022. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $499.
What is Medicare for people 65 and older?
Medicare. Medicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD) and. group health plan.
What is a group health plan?
group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families. (retiree) coverage from a former employer, generally Medicare pays first for your health care bills, and your. group health plan. In general, a health plan offered by an employer ...
Does stop loss cover out of pocket costs?
It might only provide "stop loss" coverage, which starts paying your. out-of-pocket costs. Health or prescription drug costs that you must pay on your own because they aren’t covered by Medicare or other insurance. only when they reach a maximum amount.
When do you get Medicare?
Medicare is a public health insurance program that you qualify for when you turn 65 years old. This might be retirement age for some people, but others choose to continue working for many reasons, both financial and personal. In general, you pay for Medicare in taxes during your working years and the federal government picks up a share of the costs.
How long do you have to sign up for Medicare if you have an employer?
Once your (or your spouse’s) employment or insurance coverage ends, you have 8 months to sign up for Medicare if you’ve chosen to delay enrollment.
What is Medicare Supplement?
Medicare Supplement, or Medigap, plans are optional private insurance products that help pay for Medicare costs you would usually pay out of pocket . These plans are optional and there are no penalties for not signing up; however, you will get the best price on these plans if you sign up during the initial enrollment period that runs for 6 months after you turn 65 years old.
Does Medicare cover late enrollment?
Medicare programs can help cover your healthcare needs during your retirement years. None of these programs are mandatory, but opting out can have significant consequences. And even though they’re option, late enrollment can cost you.
Do you have to sign up for Medicare if you are 65?
Medicare is a federal program that helps you pay for healthcare once you reach age 65 or if you have certain health conditions. You don ’t have to sign up when you turn 65 years old if you continue working or have other coverage. Signing up late or not at all might save you money on monthly premiums but could cost more in penalties later.
Do you pay Medicare premiums when you turn 65?
Because you pay for Medicare Part A through taxes during your working years, most people don’t pay a monthly premium. You’re usually automatically enrolled in Part A when you turn 65 years old. If you’re not, it costs nothing to sign up.
Is Medicare mandatory?
While Medicare isn’t necessarily mandatory, it may take some effort to opt out of. You may be able to defer Medicare coverage, but it’s important to if you have a reason that makes you eligible for deferment or if you’ll face a penalty once you do enroll.
How long does Medicare coverage last?
Your initial enrollment period for Medicare (all four parts) begins three months prior to the month you turn 65 and lasts until the end of the third month after your birthday month—a total of seven months. If you don’t sign up during the initial window, you can sign up between January 1st and March 31st each year for coverage that begins July 1st. Failure to sign up during the initial enrollment period, however, could result in permanently higher premiums—unless you qualify for a special enrollment period. 9
What does Medicare Part A cover?
Medicare Part A, hospital coverage, pays for your care in a hospital, skilled nursing facility, nursing home (as long as it’s not just for custodial care), hospice, and certain types of home health services. 1
What is Medicare Part D prescription drug coverage?
Prescription drug coverage is based on a medication list (called a formulary) that is included with Medicare Part D. Each Medicare prescription drug plan has its own list. Most plans place drugs into different “tiers,” with each tier having a different cost. 5
How much is Medicare Part B in 2021?
The 2021 standard monthly premium for Medicare Part B coverage is $148.50, up from $144.60 in 2020.
How long does a Medigap open enrollment period last?
So if you have a Medigap policy, you may also need Part D. 6 . A one-time Medigap open-enrollment period lasts six months and begins the month you turn 65 (and are enrolled in Part B). During this period, you can buy any Medigap policy sold in your state regardless of your health.
How long does it take for Medicare to open?
When you're first eligible for Medicare, the open enrollment period lasts roughly seven months and begins three months prior to the month of your 65th birthday.
How long do you have to enroll in Medicare after 65?
In general, the SEP requires that you enroll in Medicare no later than eight months after your group health plan or the employment on which it is based ends (whichever comes first). One important exception to SEP rules: If your group health plan or employment on which it is based ends during your initial enrollment period, you do not qualify for a SEP. 10
How Does Medicare Work with Retiree Insurance?
In general, if you have Medicare and retiree insurance, Medicare will pay your health care bills first. In this case, your group coverage is your secondary insurance. Thus, it acts similar to a Medicare Supplement policy. To get full benefits from your retiree insurance, you’ll want to enroll in Part A and Part B when you become eligible.
How to Get Answers to Retirement Insurance and Medicare Questions
We know that navigating coverage options can be confusing. That’s where we come in. We’re here to help you understand your options from the inside out. As a result, you’ll feel better prepared when it’s time for you to choose the best combination of coverage.
What to do if you retire before you qualify for Medicare?
If you're retiring before you're eligible for Medicare, compare the cost of retiree health insurance or COBRA to Marketplace insurance plans. You should also ask how the coverage changes when you're eligible for Medicare.
What age do you have to retire to get health insurance?
If you retire before age 65, you may need to find a health insurance plan to cover you until you're eligible for Medicare. Regardless of your age, you have retirement health insurance options. President Biden has signed an executive order for a special enrollment period for HealthCare.gov to assist those who have lost health insurance due ...
What are the options for Medicare if you don't have employer health coverage?
The two primary options if you don't have access to employer health coverage are: Medicare supplements: Also known as Medigap plans, these plans help cover the gaps in Medicare.
What are the different types of Medicare?
Medicare has the following parts: 1 Part A covers inpatient hospital care, limited care in a skilled nursing facility, hospice care, and some home health care. 2 Part B covers other aspects of health care, including outpatient care, doctor care, and durable medical equipment. You pay a monthly premium for Part B. 3 Part D covers prescriptions, and its benefits are accessed by purchasing Part D plans through private insurance companies.
What is the Medicare handbook?
Each year you're eligible for Medicare, you'll receive a handbook called "Medicare & You.". This handbook reviews how Medicare works and provides in-depth information on any changes. You can also download the handbook or opt to be sent an electronic copy each year.
What can an experienced health insurance agent do?
An experienced health insurance agent can help you navigate your retirement health insurance options. They can conduct a complete analysis of your options by asking you about your existing doctors and medications and then tell you which plans will provide the most cost-effective benefits based on your personal medical situation.
How old do you have to be to qualify for Medicare?
In most cases, as long as you've worked at least 10 years and paid Medicare taxes during those years, you're eligible for Medicare starting at age 65. If you're permanently disabled or have end-stage renal disease, you can qualify for Medicare before age 65. 7
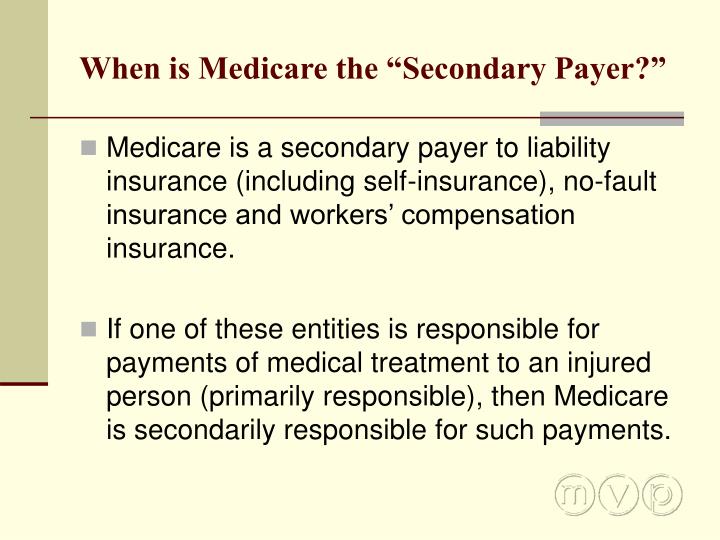
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What happens if you don't get Social Security at 65?
If you’re still working at age 65 and you’re not claiming Social Security benefits, the government will not automatically enroll you in Medicare Part A, which covers hospital stays. 1
Who is eHealth Medicare?
If you qualify for Medicare and are ready to look at plans, eHealth Medicare, an independent insurance broker and partner of Investopedia, has licensed insurance agents at <833-970-1257 TTY 711>; who can help connect you with Medicare Advantage, Medicare Supplement Insurance, and Prescription Drug Part D plans.
How long do you have to enroll in Part B?
If it doesn’t, you should enroll in Part B to avoid paying the premium penalty that’s imposed if you don’t enroll in Part B within eight months of becoming eligible for it. 1 .
