When do I apply for Medicare Part?
You can:
- Enroll in Medicare when you turn 65
- Enroll in only Medicare Part A when you turn 65
- Delay Medicare until you lose your coverage
How to enroll in Medicare Part?
They must:
- File an application to enroll by contacting the Social Security Administration;
- Enroll during a valid enrollment period; and
- Also enroll in or already have Part B.
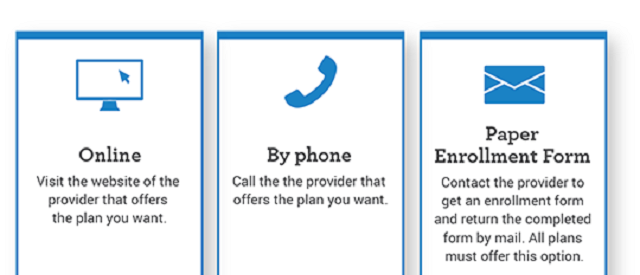
How do I apply for Medicare Part?
medicare/apply.html and select “Apply for Medicare Only.” 3. Use the “Related Information” links if you need more information. 4. Apply and complete the application, which normally takes 10 to 30 minutes. 5. Select “Submit Now” to send your application electronically to Social Security. What happens next?
What information is required to apply for Medicare Part?
You’ll need to prove that you’re eligible to enroll in Medicare. You might need to submit documents that verify your age, citizenship, military service, and work history. Social Security can help...

What is part Medicare Part A?
Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. coverage if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A." Most people get premium-free Part A.
What is Medicare Part A or B mean?
Part A provides inpatient/hospital coverage. Part B provides outpatient/medical coverage. Part C offers an alternate way to receive your Medicare benefits (see below for more information). Part D provides prescription drug coverage.
Why do you need Medicare Part A?
Medicare Part A (Hospital Insurance) Part A helps cover your inpatient care in hospitals. Part A also includes coverage in critical access hospitals and skilled nursing facilities (not custodial or long-term care). It also covers hospice care and home health care. You must meet certain conditions to get these benefits.
What is the meaning of Part A and Part B?
Part A is hospital coverage, while Part B is more for doctor's visits and other aspects of outpatient medical care. These plans aren't competitors, but instead are intended to complement each other to provide health coverage at a doctor's office and hospital.
Why do I need Medicare Part C?
Medicare Part C provides more coverage for everyday healthcare including prescription drug coverage with some plans when combined with Part D. A Medicare Advantage prescription drug (MAPD) plan is when a Part C and Part D plan are combined. Medicare Part D only covers prescription drugs.
What is the difference between Medicare A & B?
Part A (Hospital Insurance): Helps cover inpatient care in hospitals, skilled nursing facility care, hospice care, and home health care. Part B (Medical Insurance): Helps cover: Services from doctors and other health care providers.
Is Medicare Part A free?
Most people don't pay a monthly premium for Part A (sometimes called "premium-free Part A"). If you buy Part A, you'll pay up to $499 each month in 2022. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $499.
Who is eligible for Medicare Part A?
You are eligible for premium-free Part A if you are age 65 or older and you or your spouse worked and paid Medicare taxes for at least 10 years. You can get Part A at age 65 without having to pay premiums if: You are receiving retirement benefits from Social Security or the Railroad Retirement Board.
What happens if you don't enroll in Medicare Part A at 65?
If you don't have to pay a Part A premium, you generally don't have to pay a Part A late enrollment penalty. The Part A penalty is 10% added to your monthly premium. You generally pay this extra amount for twice the number of years that you were eligible for Part A but not enrolled.
How do you get Medicare Part C?
To be eligible for a Medicare Part C (Medicare Advantage) plan:You must be enrolled in original Medicare (Medicare parts A and B).You must live in the service area of a Medicare Advantage insurance provider that's offering the coverage/price you want and that's accepting new users during your enrollment period.
What is Medicare type B?
Medicare Part B helps cover medically-necessary services like doctors' services and tests, outpatient care, home health services, durable medical equipment, and other medical services. Part B also covers some preventive services. Look at your Medicare card to find out if you have Part B.
Why do I need Medicare Part B?
Medicare Part B helps cover medical services like doctors' services, outpatient care, and other medical services that Part A doesn't cover. Part B is optional. Part B helps pay for covered medical services and items when they are medically necessary.
What is national coverage?
National coverage decisions made by Medicare about whether something is covered. Local coverage decisions made by companies in each state that process claims for Medicare. These companies decide whether something is medically necessary and should be covered in their area.
Is Medicare Advantage the same as Original Medicare?
What's covered? Note. If you're in a Medicare Advantage Plan or other Medicare plan, your plan may have different rules. But, your plan must give you at least the same coverage as Original Medicare. Some services may only be covered in certain settings or for patients with certain conditions.
When do you have to be on Medicare before you can get Medicare?
Individuals already receiving Social Security or RRB benefits at least 4 months before being eligible for Medicare and residing in the United States (except residents of Puerto Rico) are automatically enrolled in both premium-free Part A and Part B.
How long does Medicare take to pay for disability?
A person who is entitled to monthly Social Security or Railroad Retirement Board (RRB) benefits on the basis of disability is automatically entitled to Part A after receiving disability benefits for 24 months.
How long do you have to be on Medicare if you are disabled?
Disabled individuals are automatically enrolled in Medicare Part A and Part B after they have received disability benefits from Social Security for 24 months. NOTE: In most cases, if someone does not enroll in Part B or premium Part A when first eligible, they will have to pay a late enrollment penalty.
How long does it take to get Medicare if you are 65?
For someone under age 65 who becomes entitled to Medicare based on disability, entitlement begins with the 25 th month of disability benefit entitlement.
What is the income related monthly adjustment amount for Medicare?
Individuals with income greater than $85,000 and married couples with income greater than $170,000 must pay a higher premium for Part B and an extra amount for Part D coverage in addition to their Part D plan premium. This additional amount is called income-related monthly adjustment amount. Less than 5 percent of people with Medicare are affected, so most people will not pay a higher premium.
What happens if you don't enroll in Part A?
If an individual did not enroll in premium Part A when first eligible, they may have to pay a higher monthly premium if they decide to enroll later. The monthly premium for Part A may increase up to 10%. The individual will have to pay the higher premium for twice the number of years the individual could have had Part A, but did not sign up.
Why does Part A end?
There are special rules for when premium-free Part A ends for people with ESRD. Premium Part A and Part B coverage can be voluntarily terminated because premium payments are required. Premium Part A and Part B coverage ends due to: Voluntary disenrollment request (coverage ends prospectively); Failure to pay premiums;
What is Part A insurance?
Part A helps cover your inpatient care in hospitals. Part A also includes coverage in critical access hospitals and skilled nursing facilities (not custodial or long-term care). It also covers hospice care and home health care. You must meet certain conditions to get these benefits.
What does Part B cover?
Part B helps cover medically necessary services like doctors’ services, outpatient care, and other medical services that Part A doesn’t cover. Part B also covers many preventive services. Part B coverage is your choice. However, you need to have Part B if you want to buy Part A.
Can I get medicare if I have SSI?
Getting SSI doesn’t make you eligible for Medicare. SSI provides a monthly cash benefit and health coverage under Medicaid. Your spouse may qualify for Medicare when he/she turns 65 or has received disability benefits for 24 months.
Does Medicare cover prescription drugs?
Medicare prescription drug coverage is available to everyone with Medicare. Private companies provide this coverage. You choose the Medicare drug plan and pay a monthly premium. Each plan can vary in cost and specific drugs covered. If you decide not to join a Medicare drug plan when you’re first eligible, and you don’t have other creditable prescription drug coverage, or you don’t get Extra Help, you’ll likely pay a late enrollment penalty. You may have to pay this penalty for as long as you have Medicare drug coverage.
Is SSI the same as disability?
monthly benefit paid by Social Security to people with limited income and resources who are disabled, blind, or age 65 or older. SSI benefits aren’t the same as Social Security retirement or disability benefits.
Who is responsible for Medicare payments?
If a federal, state, county, city or other level of government, the Indian Health Service (IHS), or an Indian tribe will be legally and financially responsible for Medicare payments received (including any potential overpayments), the name of that government, the IHS or Indian tribe must be reported as an owner or controlling entity. The DMEPOS supplier must submit a letter on the letterhead of the responsible government agency or tribal organization that attests that the government or tribal organization will be legally and financially responsible in the event that there is any outstanding debt owed to CMS. This letter must be signed by an appointed or elected official of the government or tribal organization who has the authority to legally and financially bind the government or tribal organization to the laws, regulations, and program instructions of Medicare. The appointed/elected official who signed the letter must be reported in Section 9.
What is Medicare billing number?
The Medicare Identification Number, often referred to as a Medicare supplier number or Medicare billing number is a generic term for any number other than the National Provider Identifier (NPI) that is used by a DMEPOS supplier to bill the Medicare program.
What is billing agency?
billing agency/agent is a company or individual that you contract with to prepare and submit your claims. If you use a billing agency/agent you must complete this section; you remain responsible for the accuracy of the claims submitted on your behalf.
What section of the CSA must a supplier be reported in?
the supplier MUST have at least one owner or controlling entity and one managing employee reported in Section 8 and/or Section 9.
What happens if my Medicare DMEPOS is deactivated?
If your Medicare DMEPOS supplier billing number was deactivated, you will be required to submit an updated CMS-855S. You must also meet all current requirements for your supplier type to reactivate your supplier billing number.
Where are Medicare records stored?
If the Medicare beneficiaries’ medical records are stored at a location other than the Business Location Address in Section 2A in accordance with 42 C.F.R. section 424.57 (c)(7)(E), complete this section with the name and address of the storage location. This includes the records for both current and former Medicare beneficiaries. Post office boxes and drop boxes are not acceptable as a physical address where Medicare beneficiaries’ records are maintained. The records must be the supplier’s records, not the records of another supplier. If all records are stored at the Business Location Address reported in Section 2A, check the box below and skip this section.
Do I have to submit an updated enrollment application for Medicare revalidation?
If you have been contacted by the NSC MAC to revalidate your Medicare enrollment, you will be required to submit an updated enrollment application. Do not submit an application for revalidation until you have been contacted by the NSC MAC.