- File your appeal within 120 days of receiving the Medicare Summary Notice (MSN) that lists the denied claim.
- Circle the item on your MSN that you are appealing and clearly explain why you think Medicare’s decision is wrong. ...
- Include additional information that supports your appeal. You may want to ask your doctor, health care provider or health equipment supplier for help in providing information that could assist in ...
- Carefully read the specific instructions that appear on your MSN about how to file your appeal. (Don’t forget to sign your name and include your telephone number.)
What happens if my Medicare appeal is denied?
If the appeal is denied at the third level, it can still be presented to the Medicare Appeals Council, a department within the U.S. Department of Health and Human Services. The final level of appeal is to the federal courts. You generally have 60 days to file appeals before an ALJ, the Medicare Appeals Council and to federal court.
How do I appeal a Medicare claim?
• Your representative’s signature and the date they signed the request. If you’re appointing someone to help with your appeal, send the representative a form or written request with your appeal request to the Medicare Administrative Contractor (MAC) (the company that handles claims for Medicare), or your Medicare health plan.
How do I appeal a Medicare Part D prescription drug decision?
Filing an initial appeal if you have a Medicare Part D prescription drug plan. If you disagree with your Part D plan’s decision, you can file a formal appeal. The first level of appeal is to your plan, which is required to notify you of its decision within seven days for a regular appeal and 72 hours for an expedited appeal.
Is there legal guidance on the Medicare appeals process?
“Medicare Appeals” isn’t a legal document. Official Medicare Program legal guidance is contained in the relevant statutes, regulations, and rulings. 3 Table of contents Section 1: What can I appeal, and how can I appoint a representative?

How long does it take to appeal Medicare?
The final level of appeal is to the federal courts. You generally have 60 days to file appeals before an ALJ, the Medicare Appeals Council and to federal court.
Why does Medicare reject my doctor's recommendation?
For example: Your Medicare Part D drug plan rejects your doctor’s recommendation that you receive a discount on an expensive medication because the available lower-cost drugs are not effective for your condition.
What happens if you disagree with a Medicare decision?
If you disagree with a decision about one of your Medicare claims, you have the right to challenge that decision and file an appeal. Situations in which you can appeal include: Denials for health care services, supplies or prescriptions that you have already received. For example: During a medical visit your doctor conducts a test.
How to report Medicare not paying?
If you still have questions about a claim you think Medicare should not have paid, report your concerns to the Medicare at 1-800-MEDICARE. Make copies for your records of everything you are submitting. Send the MSN and any additional information to the address listed at the bottom on the last page of your MSN.
What to do if Medicare Advantage decision is not in your favor?
In addition, Medicare Advantage companies must give patients a way to report grievances about the plan and the quality of care they receive from providers in the plan.
When a doctor submits a claim to be reimbursed for that test, what does Medicare determine?
When the doctor submits a claim to be reimbursed for that test, Medicare determines it was not medically necessary and denies payment of the claim. Denials of a request you or your doctor made for a health care service, supply or prescription. For example: Medicare determines that a wheelchair is not medically necessary for your condition.
How to request a plan exception?
Requests for plan exceptions can be made by phone or in writing if you are asking for a prescription drug you haven’t yet received. If you are asking to be reimbursed for the price of drugs you have already bought, you must make your request in writing.
What to do if you are not satisfied with the IRE decision?
If you’re not satisfied with the IRE’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or, in certain circumstances, a review of the appeal record by an ALJ or an attorney adjudicator.
How long does it take for an IRE to review a case?
They must get this information within 10 days after the date you get the notice telling you your case file has been sent to the IRE. The IRE’s address is on the notice.
What to do if you are not satisfied with QIC?
If you’re not satisfied with the QIC’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or , in certain circumstances, a review of the appeal record by an ALJ or attorney adjudicator.
What is the ABN for Medicare?
If you have Original Medicare and your doctor, other health care provider, or supplier thinks that Medicare probably (or certainly) won’t pay for items or services, he or she may give you a written notice called an ABN (Form CMS-R-131).
What happens if you disagree with a decision?
If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you’ll get instructions on how to move to the next level of appeal.
Do doctors have to give advance notice of non-coverage?
Doctors, other health care providers, and suppliers don’t have to (but still may) give you an “Advance Beneficiary Notice of Noncoverage” for services that Medicare generally doesn’t cover, like:
Does CMS exclude or deny benefits?
The Centers for Medicare & Medicaid Services (CMS) doesn’t exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, disability, sex, or age in admission to, participation in, or receipt of the services and benefits under any of its programs and activities, whether carried out by CMS directly or through a contractor or any other entity with which CMS arranges to carry out its programs and activities.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
What is Medicare appeal?
a particular health care service, certain supplies, a particular item, or a prescription drug that you believe should be covered that you think you should be able to get; or. payment for a health care service, certain supplies, a particular item, or a prescription drug you already received. It’s also possible to make an appeal if Medicare ...
How many levels of appeals are there for Medicare?
For each part of the Medicare program (Part A, Part B, Part C, and Part D), the appeals process has five different levels. If you want to further appeal a decision made at any level of the process, you can usually go to the next level.
What are the levels of appeals?
The appeals process consists of five different levels: Level 1: Redetermination by the Medicare administrative contractor. Level 2: Reconsideration by a qualified independent contractor. Level 3: A hearing before an administrative law judge. Level 4: Review by the Medicare Appeals Council. Level 5: Judicial review by a federal district court.
What is the level of Medicare?
Level 1: Reconsideration from your plan. Level 2: Review by an independent review entity. Level 3: Decision by the Office of Medicare Hearings and Appeals. Level 4: Review by the Medicare Appeals Council. Level 5: Judicial review by a federal district court.
How often do you get Medicare Summary Notice?
Those who have Original Medicare (Medicare Part A and Part B) will receive what’s called a “Medicare Summary Notice” every three months in the mail, if you get Part A and Part B-covered items and services. This notice will show the items and services that providers and suppliers have billed ...
What is an organization determination in Medicare?
Those who have a Medicare Advantage Plan or other Medicare health plan can request that the plan provide or pay for items or services that they believe should be covered, provided , or continued. Commonly, this is referred to as an “organization determination.”
What to do if you disagree with a decision?
If you disagree with a decision, you can make an appeal. (The notice will have information about your right to appeal.) Should you decide to appeal, you should request any information that may help your case from your doctor, other health care provider, or supplier.
How to appeal a Medicare reconsideration?
Include this information in your written reconsideration request: 1 Your name, address, and the Medicare number on your Medicare card [JPG]. 2 The items or services for which you're requesting a reconsideration, the dates of service, and the reason (s) why you're appealing. 3 If you've appointed a representative, include the name of your representative and proof of representation.
What to include in appeal for reconsideration?
If you've appointed a representative, include the name of your representative and proof of representation. Include any other information that may help your case.
How long does it take for a health insurance company to respond to a request?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days. Payment request—60 days. You'll get a fast request if your plan determines, or your doctor tells your plan, that waiting for a standard service decision may seriously jeopardize your: Life. Health.
What level is an appeal sent to?
If the plan decides against you (fully or partially), your appeal is automatically sent to level 2.
What to do if you haven't gotten a service?
If your appeal is for a service you haven’t gotten yet, your doctor can ask for a reconsideration on your behalf and must notify you about it. You, your representative, or your doctor must file a written standard or expedited (fast) request, unless your plan allows you to file a request by phone, fax, or email.
How many levels of appeals are there for Medicare?
Your Medicare drug plan will send you a written decision. If you disagree with this decision, you have the right to appeal. The appeals process has 5 levels. If you disagree with the decision made at any level of the process, you can generally go to the next level.
What happens if a pharmacy can't fill a prescription?
If your network pharmacy can't fill a prescription, the pharmacist will show you a notice that explains how to contact your Medicare drug plan so you can make your request.
What are the levels of appeal?
At each level, you'll get instructions in the decision letter on how to move to the next level of appeal. Level 1: Redetermination from your plan. Level 2: Review by an Independent Review Entity (IRE) Level 3: Decision by the Office of Medicare Hearings and Appeals (OMHA) Level 4: Review by the Medicare Appeals Council ( Appeals Council) ...
Should prior authorization be waived?
You or your prescriber believes that a coverage rule (like prior authorization) should be waived. You think you should pay less for a higher tier (more expensive) drug because you or your prescriber believes you can't take any of the lower tier (less expensive) drugs for the same condition.
How to request a fast medical appeal?
Fast Medical (Expedited) Appeals. You or your doctor (without an appointment of representative form) can request a Fast Medical Appeal by phone or mail if waiting for a Standard Appeal could harm your health or your ability to function. You can get one: For medical care you have not yet received.
Who can act for you on a medical appeal?
You or your appointed representative (someone you name to act for you) may ask for a medical appeal. You can name a relative, friend, attorney, doctor, or someone else to act for you with an Appointment of Representative form. Under state law, others may already be allowed to act for you.
What is an appeal in insurance?
What is an appeal? An appeal, or redetermination, is a formal way to ask the plan to review a coverage decision about health care services and/or prescription drugs. You may ask for a review when you are not satisfied with our initial coverage decision.
How long does it take to get a fast appeal for a prescription?
If you are asking for a Fast Appeal for prescription drugs, we will give you an answer within 72 hours of receipt of your request.
What happens if you don't agree with a judge's decision?
If you do not agree with the decision the judge makes, you can move on to a Level 4 Appeal. At the Level 4 Appeal, the Medicare Appeals Council, who works for the federal government, will review your appeal and give you an answer.
How long does it take to get an appointment of representative for Medicare?
Under state law, others may already be allowed to act for you. Get an Appointment of Representative form [PDF] You must make your request within 60 days from the date of the coverage determination. A coverage determination is the first decision made by your Medicare drug plan (not the pharmacy) about your drug benefits.
How to appeal a level 3 drug?
To reach a Level 3 Appeal, the dollar value of the drug or medical care you are asking for must meet a minimum amount. If the dollar value is too low, you cannot make another appeal and the decision at Level 2 is final. The notice you get denying your Level 2 Appeal will tell you if the dollar value is high enough to move on to Level 3. If you qualify for a Level 3 Appeal, an Administrative Law Judge will review your appeal and make a decision. If you do not agree with the decision the judge makes, you can move on to a Level 4 Appeal.
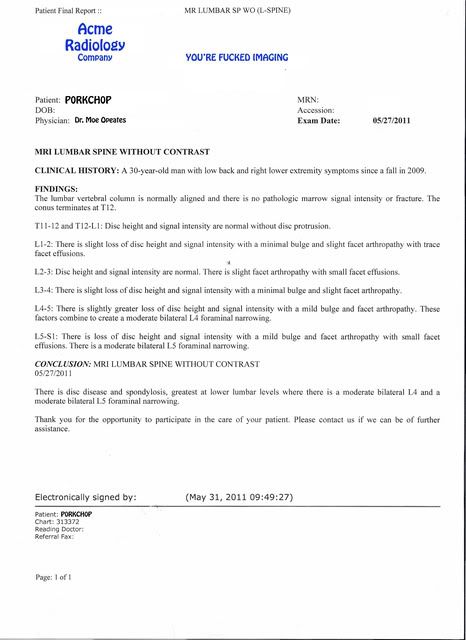
What is the Medicare deductible for MRI?
Medicare coverage takes care of 80 percent of the authorized costs, but you will be responsible for paying the Part B deductible. For 2019, the deductible is $185.00.
Who must prescribe MRI?
These requirements include the following criteria: The MRI must be prescribed by your doctor or health care provider as part of the treatment for a medical issue. All parties involved in the procedure, (i.e. the doctor who prescribes the. MRI and the provider administering the MRI) must accept Medicare assignment.
What is an MRI scan?
An MRI scan is a painless and non-invasive exam that provides invaluable diagnostic information helping your physician give you optimum care. If you are enrolled in a Medicare Advantage plan, check with your plan directly to find out your exact costs for an MRI. Related articles: Medicare Part C.
What is an MRI?
An MRI helps diagnose certain conditions such as stroke, brain injury or aneurysm, or multiple sclerosis. It also helps physicians detect tumors or other abnormalities in organs, bones, and joints. If your doctor suggests that you have an MRI scan, you need to know whether your Medicare insurance plan covers the cost.
How much does an MRI cost?
In the United States, the average cost of an MRI is around $2,600.00. Prices can range greatly, between a few hundred to several thousand dollars. Original Medicare Part B does take care of 80 percent of the final cost, but that means you still must pay 20 percent out-of-pocket, in most cases.
What is the deductible for a 2019 scan?
For 2019, the deductible is $185.00. Even if you have Medicare Part B or are enrolled in a Medicare Advantage plan, you must meet some additional requirements for Medicare to pay for the cost of the scan. These requirements include the following criteria:
When do you have to be 65 to get Medicare?
Most people automatically are enrolled in Part A when they turn 65 as long as they paid taxes while working for a certain period of time.