
If Medicare refuses to pay for a service under Original fee-for-service Part A or Part B, the beneficiary should receive a denial notice. The medical provider is responsible for submitting a claim to Medicare for the medical service or procedure. If Medicare denies payment of the claim, it must be in writing and state the reason for the denial. This notice is called the Medicare Summary Notice (MSN) and is usually issued quarterly.
Why did Medicare deny my claim?
Though Medicare is designed to give seniors and certain disabled individuals the most unobstructed access to healthcare possible, there are some rare circumstances that may unfortunately lead to a Medicare claim denial. When a Medicare claim is denied, you will receive a letter notifying you that a specific service or item is not covered or no longer covered. This …
How to appeal a Medicare claim denial decision?
B, the beneficiary should receive a denial notice. The medical provider is responsible for submitting a claim to Medicare for the medical service or procedure. If Medicare denies payment of the claim, it must be in writing and state the reason for the denial. This notice is called the Medicare Summary Notice (MSN) and is usually issued quarterly. Look for the reason for denial.
Can someone be denied Medicare?
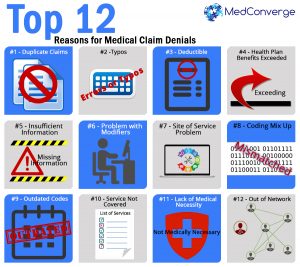
Feb 28, 2021 · The common reasons why a claim gets denied include: The claim is not considered that of a medical necessity. The claim has some payer/contractor issues. The expenses in the claim were incurred before or after the beneficiary was insured by Medicare. It’s a duplicate claim; How To Reverse a Denial or Rejection from Medicare.
When do insurance companies deny claims?
Q: Medicare denied payment for services I recently had and indicated I could appeal the decision. How do I start this process? A: Denial of payment for services can occur for many reasons. Before starting the appeal process it would be wise to talk with the provider’s office to …
What happens when Medicare denies a claim?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: A request for a health care service, supply, item, or drug you think Medicare should cover.
Who pays for Medicare claims?
Medicare claim payments at a glanceMedicare planWho pays?*ORIGINAL MEDICARE Coverage from the federal governmentMedicare Part A: Covers hospitalizationMedicare is primary payer for Part A services Member pays the rest6 more rows•Sep 1, 2016
How do you handle a denied Medicare claim?
File your appeal within 120 days of receiving the Medicare Summary Notice (MSN) that lists the denied claim. Circle the item on your MSN that you are appealing and clearly explain why you think Medicare's decision is wrong. You can write on the MSN or attach a separate page.
Will secondary pay if primary denies?
If your primary insurance denies coverage, secondary insurance may or may not pay some part of the cost, depending on the insurance. If you do not have primary insurance, your secondary insurance may make little or no payment for your health care costs.
Why is Medicare not paying on claims?
If the claim is denied because the medical service/procedure was “not medically necessary,” there were “too many or too frequent” services or treatments, or due to a local coverage determination, the beneficiary/caregiver may want to file an appeal of the denial decision. Appeal the denial of payment.
Do Medicare benefits have to be repaid?
The payment is "conditional" because it must be repaid to Medicare if you get a settlement, judgment, award, or other payment later. You're responsible for making sure Medicare gets repaid from the settlement, judgment, award, or other payment.
How successful are Medicare appeals?
People have a strong chance of winning their Medicare appeal. According to Center, 80 percent of Medicare Part A appeals and 92 percent of Part B appeals turn out in favor of the person appealing.Jun 20, 2013
Can you be denied Medicare?
In all but four states, insurance companies can deny private Medigap insurance policies to seniors after their initial enrollment in Medicare because of a pre-existing medical condition, such as diabetes or heart disease, except under limited, qualifying circumstances, a Kaiser Family Foundation analysis finds.Jul 11, 2018
How do you win a Medicare appeal?
To increase your chance of success, you may want to try the following tips: Read denial letters carefully. Every denial letter should explain the reasons Medicare or an appeals board has denied your claim. If you don't understand the letter or the reasons, call 800-MEDICARE (800-633-4227) and ask for an explanation.Nov 12, 2020
Is it better to have Medicare as primary or secondary?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
How do you know if Medicare is primary or secondary?
Medicare pays first and your group health plan (retiree) coverage pays second . If the employer has 100 or more employees, then the large group health plan pays first, and Medicare pays second .
Does Medicare automatically send claims to secondary insurance?
Medicare will send the secondary claims automatically if the secondary insurance information is on the claim. As of now, we have to submit to primary and once the payments are received than we submit the secondary.Aug 19, 2013
Why is my Medicare claim denied?
The common reasons why a claim gets denied include: The claim is not considered that of a medical necessity. The claim has some payer/contractor issues. The expenses in the claim were incurred before or after the beneficiary was insured by Medicare. It’s a duplicate claim.
What are the reasons for denying a claim?
Denied claims, on the other hand, have all the necessary information and are valid to be processed but are not going to get paid. The common reasons why a claim gets denied include: 1 The claim is not considered that of a medical necessity. 2 The claim has some payer/contractor issues. 3 The expenses in the claim were incurred before or after the beneficiary was insured by Medicare. 4 It’s a duplicate claim
What is Medicare insurance?
Medicare is a federal health insurance program for certain individuals in the country. Medicare’s main goal is to subsidize healthcare services for select individuals that need the most help. These include the following:
How many types of Medicare are there?
As mentioned above, there are 4 types of Medicare coverage, and each one has its own “specialties”. Basic Medicare coverage includes Part A and B and is often called Original Medicare.
What is part A of Medicare?
Also called “hospital insurance”, Part A covers expenses incurred for hospital stays, care in a skilled nursing facility, some home health care, and hospice care. It is worth noting that this plan does not cover long-term care or custodial care.
What is the Medicare deductible for 2021?
Medicare Part B. Part B covers the cost of outpatient care. This includes doctor visits, preventative services, mental health coverage, and ambulance services. For the year 2021, the standard monthly premium is $148.50 and the deductible sits at $203. The premium increases for people who have an annual income of $88,000 or more.
Can you appeal a claim that was denied?
When your claim was denied simply due to incorrect information, you can easily reopen the claim using a Clerical Error Reopening or CER. When a claim is denied for reasons that cannot be addressed with a CER then it should be appealed. To appeal, you need to write a letter and there are five appeal levels you can pursue.
Does Medicare Supplement cover medical expenses?
Your Medicare Supplement plan typically wouldn’t cover those costs . So, if Medicare Part A and/or Part B deny a claim for medical services you had or wish to have, generally a Medicare Supplement plan won’t cover it. There might be items and services that a Medicare Supplement plan may cover that Medicare doesn’t typically approve for coverage.
Does Medicare Supplement pay for deductibles?
Medicare Supplement insurance typically helps pay for Medicare Part A and Part B coinsurance and copayments. It also may help pay Original Medicare deductibles and certain other out-of-pocket costs . Medicare Supplement insurance only works alongside Original Medicare, Part A and Part B. As the name implies, it’s a supplement – it adds ...
Does Medicare Supplement Insurance cover copayments?
Summary: With most of its benefits, Medicare Supplement insurance depends on Medicare’s approval in order to help pay Medicare copayments and coinsurance. If Medicare doesn’t cover it, in most cases, neither will Medicare Supplement insurance.
What is a denial of a request?
Denials of a request you or your doctor made for a health care service, supply or prescription. For example: Medicare determines that a wheelchair is not medically necessary for your condition. Denials of a request you and your doctor have made to change the price you pay for a prescription drug. For example: Your Medicare Part D drug plan rejects ...
How long does it take to appeal Medicare?
The final level of appeal is to the federal courts. You generally have 60 days to file appeals before an ALJ, the Medicare Appeals Council and to federal court.
How to request a plan exception?
Requests for plan exceptions can be made by phone or in writing if you are asking for a prescription drug you haven’t yet received. If you are asking to be reimbursed for the price of drugs you have already bought, you must make your request in writing.
Can you appeal a Part D plan?
If your life or health could be at risk by having to wait for a medication approval from your plan, you or your doctor can request an expedited appeal by phone. If you disagree with your Part D plan’s decision, you can file a formal appeal.
Can you appeal a Medicare Advantage plan?
Medicare Advantage plans, which are administered by private insurance companies, are required by Medicare to have an appeals process by which you can get a redetermination if your plan denies you a service or benefit you think should be covered. If you disagree with the decision, you can request an independent review.
What is an ABN in Medicare?
reimbursed by Medicare and may be billed to the patient. An ABN must: (1) be in writing; (2) be obtained prior to the beneficiary receiving the. service; (3) clearly identify the particular service; (4) state that the provider believes.
What is an ABN form?
An Advance Beneficiary Notice (ABN), sometimes called a patient waiver form, is used to. document that the patient is aware that Medicare may not pay for a test or procedure and. has agreed to pay the provider in the event payment is denied. Each ABN must be specific.
Can Medicare deny payment?
However, when a Medicare carrier is. likely to deny payment because of medical necessity policy (either as stated in their written. Medical Review Policy or upon examination of individual claims) the patient must be. informed and consent to pay for the service before it is performed. Otherwise, the patient.
Does Medicare cover cholesterol screening?
Medicare patients may be billed for services that are clearly not covered. For example,#N#routine physicals or screening tests such as total cholesterol are not covered when there is#N#no indication that the test is medically necessary. However, when a Medicare carrier is#N#likely to deny payment because of medical necessity policy (either as stated in their written#N#Medical Review Policy or upon examination of individual claims) the patient must be#N#informed and consent to pay for the service before it is performed. Otherwise, the patient#N#has no obligation to pay for the test.
