How Does Medicare Prior Authorization Work? Prior authorization works by having your health care provider or supplier submit a prior authorization form to their Medicare Administrator Contractor (MAC).
Full Answer
What is Medicare prior authorization?
Prior authorization is a requirement that a health care provider obtain approval from Medicare to provide a given service. Prior Authorization is about cost-savings, not care. Under Prior Authorization, benefits are only paid if the medical care has been pre-approved by Medicare. Private, for-profit plans often require Prior Authorization.
Does Medicare cover Prolia?
If you are eligible, Medicare covers 80 percent of the Medicare approved cost. You must also pay the deductible for Medicare Part B which is $185.00 in 2019. Many Medicare recipients enroll in Part D prescription drug plans to help cover the costs of medications. Most Part D plans will include Prolia on its formulary, or list of covered drugs.
What are the contraindications for Prolia?
Prolia® is contraindicated in women who are pregnant and may cause fetal harm. In women of reproductive potential, pregnancy testing should be performed prior to initiating treatment with Prolia®. Prolia® is contraindicated in patients with a history of systemic hypersensitivity to any component of the product.
What happens if you take Prolia every year?
The result is that your bones can become brittle and can break more easily. Prolia works by preventing the development of cells that remove old bone. The drug is administered as a twice-a-year injection that is administered under one’s upper arm, upper thigh or abdomen.
Does Medicare require prior authorization for Prolia?
All requests for Xgeva (denosumab), Prolia (denosumab) require a prior authorization and will be screened for medical necessity and appropriateness using the criteria listed below.
How do I bill Medicare for Prolia injection?
The administration of denosumab, when billed, should be billed using the therapeutic administration code 96372 (Therapeutic prophylactic, or diagnostic injection (specify substance or drug); subcutaneous or intramuscular. Correct coding requires that a bone metastasis diagnosis (ICD-10-CM code C79.
How do I submit an authorization to Medicare?
To do so, you can print out and complete this Medicare Part D prior authorization form, known as a Coverage Determination Request Form, and mail or fax it to your plan's office. You should get assistance from your doctor when filling out the form, and be sure to get their required signature on the form.
Does Medicare do pre authorizations?
Prior authorization is a requirement that a health care provider obtain approval from Medicare to provide a given service. Prior Authorization is about cost-savings, not care. Under Prior Authorization, benefits are only paid if the medical care has been pre-approved by Medicare.
Does Medicare Part B pay for Prolia injections?
Injectable Drugs Coverage Medicare Part A or Medicare Part B will pay for a portion of the cost of osteoporosis medications delivered intravenously or by injection. These medications may include ibandronate (Boniva), zoledronic acid (Reclast), denosumab (Prolia) and sometimes calcitonin (Miacalcin).
Does Medicare Part D pay for Prolia?
The average out-of-pocket (OOP) cost for Prolia® through Medicare Part D is $115‡ every 6 months, which equals $19.16 per month. For patients with limited income: Medicare beneficiaries may qualify for Extra Help, a program to help pay for medication costs through Medicare Part D.
What is the prior authorization process?
Prior authorization—sometimes called precertification or prior approval—is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.
What CPT codes does Medicare require prior authorization?
When the trial is rendered in a setting other than the OPD, providers will need to request prior authorization for CPT code 63650 as part of the permanent implantation procedure in the hospital OPD. Please see additional information in the Operational Guide (PDF) and Frequently Asked Questions (PDF).
Does Medicare supplement plans require prior authorization?
No, we don't require any prior authorizations. We follow Medicare's guidelines to determine if a procedure is medically necessary and eligible for coverage.
What services does not require prior authorization?
No pre-authorization is required for outpatient emergency services as well as Post-stabilization Care Services (services that the treating physician views as medically necessary after the emergency medical condition has been stabilized to maintain the patient's stabilized condition) provided in any Emergency Department ...
How do I fill out Medicare HCFA 1500 form?
14:5319:58How-to Accurately Fill Out the CMS 1500 Form for Faster PaymentYouTubeStart of suggested clipEnd of suggested clipField 1 is the very first field on the CMS 1500 form and it tells the insurance carrier the categoryMoreField 1 is the very first field on the CMS 1500 form and it tells the insurance carrier the category of insurance that the policy falls into. It can be left blank.
How do I know if Medicare will cover a procedure?
Ask the doctor or healthcare provider if they can tell you how much the surgery or procedure will cost and how much you'll have to pay. Learn how Medicare covers inpatient versus outpatient hospital services. Visit Medicare.gov or call 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048.
What is the best treatment for osteoporosis?
If you are a post-menopausal woman who has osteoporosis, your physician may suggest taking Prolia. Prolia, or the generic denosumab, is a prescribed injectable medication can be prescribed for post-menopausal women to reduce the incidence of vertebral, non-vertebral, or hip fractures.
Does Medicare cover Prolia?
Many Medicare recipients enroll in Part D prescription drug plans to help cover the costs of medications. Most Part D plans will include Prolia on its formulary, or list of covered drugs. Through Medicare Part D, Prolia is covered for approximately 95 percent of its beneficiaries, 50 percent of whom do not need prior authorization. Because this coverage depends on your individual medical benefit coverage plan, it is best to discuss the details with your plan and your physician.
Does Prolia help with osteoporosis?
It can also be prescribed to increase bone mass in men with osteoporosis. Prolia helps bones retain mass and strength. It is worth your time to find out more about whether your Medicare insurance plan pays for treatment, if you are eligible, what to expect from this treatment, and if Prolia is right for you.
What is prior authorization in Medicare?
Medicare Prior Authorization. Prior authorization is a requirement that a health care provider obtain approval from Medicare to provide a given service. Prior Authorization is about cost-savings, not care. Under Prior Authorization, benefits are only paid if the medical care has been pre-approved by Medicare.
Do Medicare Advantage plans require prior authorization?
Private, for-profit plans often require Prior Authorization. Medicare Advantage (MA) plans also often require prior authorization to see specialists, get out-of-network care, get non-emergency hospital care, and more.
How does Prolia work?
The result is that your bones can become brittle and can break more easily. Prolia works by preventing the development of cells that remove old bone. The drug is administered as a twice-a-year injection that is administered under one’s upper arm, upper thigh or abdomen.
What are the requirements for home health care?
Meet Medicare’s requirements for getting home health services. Have a bone fracture that is related to post-menopausal osteoporosis. Have received a doctor’s certification that they (or their caretaker) are unable to administer the injection.
How much is Medicare Part B deductible in 2021?
You must meet your Medicare Part B deductible ( $203 per year in 2021) before Medicare will pay its share. You can also consider enrolling in a Medicare Part D prescription drug plan to get help paying for some of your prescription drugs.
Does Medicare cover Prolia?
If Medicare covers your Prolia treatment, you will typically be required to pay certain Medicare out-of-pocket costs.
How long does it take to monitor calcium levels after Prolia?
In patients predisposed to hypocalcemia and disturbances of mineral metabolism, including treatment with other calcium-lowering drugs, clinical monitoring of calcium and mineral levels is highly recommended within 14 days of Prolia® injection.
What are the symptoms of Prolia?
Symptoms have included hypotension, dyspnea, throat tightness, facial and upper airway edema, pruritus, and urticaria. If an anaphylactic or other clinically significant allergic reaction occurs, initiate appropriate therapy and discontinue further use of Prolia®.
Is Prolia contraindicated for hypocalcemia?
Contraindications: Prolia ® is contraindicated in patients with hypocalcemia. Pre-existing hypocalcemia must be corrected prior to initiating Prolia ®. Prolia® is contraindicated in women who are pregnant and may cause fetal harm. In women of reproductive potential, pregnancy testing should be performed prior to initiating treatment with Prolia®.
Why do we need prior authorization?
Prior authorization can help protect a beneficiary’s rights to covered Medicare benefits, and it can also act as a means of reducing improper billing, waste and fraud within the Medicare system . It also helps to cut down on over-utilization of unnecessary care.
Do you need prior authorization for Medicare Part C?
It’s not uncommon, however, for beneficiaries of Medicare Advantage (Medicare Part C) plans and Medicare Part D Prescription Drug plans to need prior authorization before receiving some types of care. Prior authorization is most common for getting certain prescription drugs covered by your plan.
Is Prolia Covered by Medicare?
Prolia is often covered by Medicare. Which part of Medicare provides coverage and how much you can expect to pay out of pocket for the treatment depends on numerous factors, but Part B is usually what covers Prolia.
What Does Prolia Do?
Throughout your life, your body breaks down existing bone and builds new bone in its place to keep your skeleton strong. Osteoclasts are the cells that drive the process. As you age, the bone-building process slows down while the work of osteoclasts continues at the same pace. This leads to a loss of bone density.
How Much Does Prolia Cost Per Year?
The list price for one dose of Prolia was around $1,300 as of October 2021, according to Amgen, the manufacturer of the drug. Most people get one Prolia injection every six months, making the average cost for one year of treatment with no insurance or Medicare coverage around $2,600.
What Part of Medicare Pays for Prolia?
For those who meet the criteria prescribed above, Medicare Part B covers Prolia. If you don't meet the above criteria, your Medicare Part D plan may cover the drug. GoodRx reports that 98% of surveyed Medicare prescription plans cover the drug as of October 2021. With Medicare Part D coverage, you’re likely to pay coinsurance or a copay.
Is There a Generic Version of Prolia?
The generic name for Prolia is denosumab. As of October 2021, no generic forms of the drug have been approved by the FDA.
What Tier Is Prolia?
Your Medicare Part D plan has a formulary that spells out which drugs it covers. In the formulary, drugs are divided into the following tiers:
How Much Does Prolia Cost With Medicare?
If you qualify for coverage for Prolia under Medicare Part B, your plan will typically pay 80% of the injection while you pay the remaining 20%. Based on the list price of the drug, the 20% coinsurance would amount to roughly $250. You'll usually need to satisfy your Medicare Part B deductible before your plan will cover the drug.
What is pre claim review?
Under pre-claim review, the provider or supplier submits the pre-claim review request and receives the decision prior to claim submission; however, the provider or supplier can render services before submitting the request. A provider or supplier submits either the prior authorization request or pre-claim review request with all supporting medical ...
What is CMS in Medicare?
The Centers for Medicare & Medicaid Services (CMS) runs a variety of programs that support efforts to safeguard beneficiaries’ access to medically necessary items and services while reducing improper Medicare billing and payments. Through prior authorization and pre-claim review initiatives, CMS helps ensure compliance with Medicare rules.
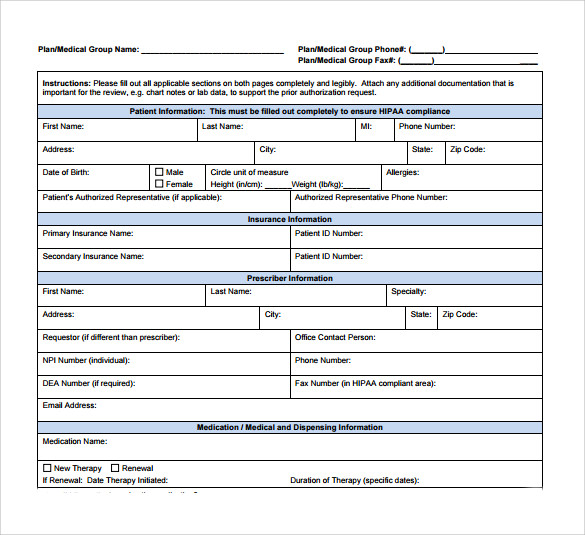
What is a prior authorization form for Medicare?
Medicare Prior (Rx) Authorization Form. Medicare members who have prescription drug coverage (Part D) will be covered for almost all their medication costs. Original Medicare members most likely have chosen to join a Medicare Prescription Drug Plan (PDP) for an additional premium.
How to get a fax number for a Medicare plan?
Step 1 – Enter the name, phone number, and fax number of the member’s plan. Step 2 – In the “Patient Information” section, provide the patient’s name, ID number, address, phone number, gender, and date of birth.
How long does it take for a health insurance plan to respond?
Call your plan or check on their website to look up the proper mailing address or fax number. Plans must respond within 72 hours of receiving your request form. If the physician feels the request is an emergency situation, an expedited review of 24 hours should take place.