
These are the steps you can take to void/cancel a claim:
- Contact the payer and advise that a claim was submitted in error. Ask if this claim should be voided/cancelled, so that...
- Some payers will allow you to void/cancel the claim over the phone. You can reference the claim using the client's name,...
- If the payer requires a voided/cancelled claim to be submitted,...
Full Answer
What to do if Medicare denies your medical claim?
You can also take other actions to help you accomplish this:
- Reread your plan rules to ensure you are properly following them.
- Gather as much support as you can from providers or other key medical personnel to back up your claim.
- Fill out each form as carefully and exactly as possible. If necessary, ask another person to help you with your claim.
What if Medicare denies my claim?
- Your bill will be sent directly to Medicare.
- The appeal must be filed within 120 days of receiving the Medicare Summary Notice (MSN) that shows that your claim was denied.
- If you disagree with a Medicare coverage decision in the MSN, you can appeal the decision.
How to void/cancel a claim?
These are the steps you can take to void/cancel a claim:
- Contact the payer and advise that a claim was submitted in error. Ask if this claim should be voided/cancelled, so that you can submit a claim with the correct information. ...
- If the payer requires a voided/cancelled claim to be submitted, request the original claim number. ...
- Open the claim that was submitted in error and click Edit to Resubmit. ...
How to cancel a Medicare claim you submitted yourself?
When and How to Cancel a Medicare Claim You've Filed
- You can call Medicare to cancel a claim that you’ve filed.
- Your doctor or provider will typically file claims for you.
- You might have to file your own claim if your doctor won’t or can’t.
- When you use original Medicare, you can file claims for Part B services or Part A services received in another country.
How to cancel a claim in B9997?
The claims correction, option 03, allows you to cancel paid claims in a status location P B9997. Once you select option 03, the claims and attachments correction menu appears. Once in the claim and attachments correction menu, to cancel a claim, key the claim cancels option that matches your provider type in the "ENTER MENU SELECTION" field and press "Enter."
What happens when a claim is cancelled in FISS?
Once the claim is cancelled, the inquiry screen in FISS will show both the original claim and the cancelled claim.
Can MSP claims be cancelled electronically?
MSP Claims can be cancelled electronically or through DDE / FISS.
Can you suppress a cancelled claim?
Note: If a cancelled claim, TOB XX8, returns to you in status T B9997, you are not able to make corrections nor can you suppress the canceled claim. You must allow time for these returned claims to drop off the system. However, a new cancel claim, XX8, may be submitted.
How to cancel Medicare self-filed claim?
If a person then decides to cancel the claim, they can call the general Medicare at 800-MEDICARE (800-633-4227) and explain they want to cancel a self-filed claim.
What happens if Medicare denies a claim?
If Medicare denies the claim, a person may decide to appeal.
What is Medicare appeals?
Medicare provides an appeals service so that if a doctor or other health service provider refuses to file a claim, a person can file a complaint. To get help with filing a complaint, a person can contact their State Health Insurance Assistance P rogram (SHIP).
What is Medicare reimbursed for?
Medicare reimburses health providers for the services and equipment supplied to Medicare beneficiaries. The supplier is responsible for submitting the bill, also known as a claim, to Medicare for the covered services. However, there may be occasions when a person self-files a claim and then wants to cancel it. ...
How long does it take to file a Medicare claim?
Because Medicare allows a 1-year period for a healthcare provider to file a claim, a person may have to wait until that deadline approaches before following up to find out if the provider has claimed.
How to check status of Medicare claim?
In general, if there are no delays due to incorrect documentation, Medicare processes claims within 60 days. A person will then get the Medicare decision by mail in a Medicare summary notice (MSN). A person can also check the status of their claim in the MyMedicare account.
How long does it take for Medicare to send an MRN?
Medicare will send an MRN within another 60 days that outlines their decision.
When is the claim void/cancel process used?
The claim void/cancel process is only used if a processed claim should never have been submitted.
When is a justification statement required for a claim adjustment?
A justification statement is required if the adjustment is submitted beyond the timely filing limit.
How to access RTP claims in DDE?
To access RTP claims in the DDE Claims Correction screen, select option 03 (Claims Correction) from the Main Menu and the appropriate menu selection under Claims Correction (21 – Inpatient, 23 – Outpatient, 25 – SNF).
What to do if you overpay a MSP?
If you identify an overpayment (e.g., due to a billing error or MSP involvement), you should submit an electronic adjustment or void the claim.
How long does it take for a RTP claim to be corrected?
The RTP claim is not corrected within 180 days (or no longer appears in the Claim Correction screen) and becomes inactive (IB9997)
What is claim adjustment?
The claim adjustment process is used to make corrections to processed or rejected claims. Adjustment claims may be submitted via DDE or your electronic software.
How to adjust a claim in DDE?
To adjust a claim via DDE, select option 03 (Claims Correction) from the Main Menu and the appropriate menu selection under Claim Adjustments (30 – Inpatient, 31 – Outpatient, 32 – SNF).
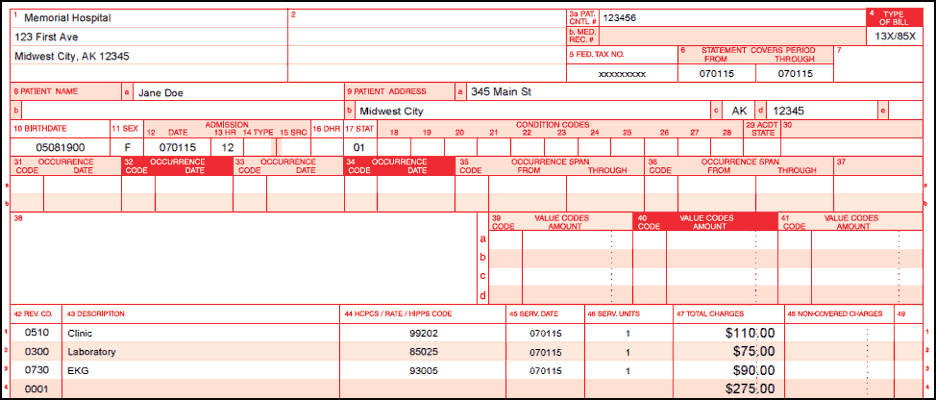
How to submit a paper void request for claims other than pharmacy and dental?
To submit a paper void request for claims other than pharmacy and dental, complete the void request form and attach a photocopy of the remittance advice (RA) containing the claims to be voided. Circle each claim internal control number (ICN) to be voided on the copy of the remittance advice (RA).
Do you send checks with a paper void request?
DO NOT send checks with the paper void request. Only include the Remittance Advice.
Can you have multiple claims voided?
If you need several claims voided for the same reason, you may batch them together with one Void Request Form.
What is the overarching adjustment claim logic?
“Overarching adjustment claim logic” is defined as the logic that CWF will employ, independent of a specific review of claim monetary changes, when a COBA trading partner’s COIF specifies that it wishes to exclude all adjustment claims.
Does CWF exclude Part B claims?
The CWF shall continue to exclude Part B claims paid at 100 percent by checking for the presence of claims entry code ‘1’ and determining that each claim’s allowed amount equals the reimbursement amount and confirming that the claim contains no denied services or service lines.
What is a void request?
A void request will be processed as a replacement to the original, incorrectly paid claim. When a claim is voided, the total payment for the original claim is deducted. There is no time limit on submitting a void. The provider can submit a paper void request on the remittance voucher, a legible photocopy of the#N#original claim, or an entirely new claim.
How to voide a remittance voucher?
A claim can be voided by photocopying the remittance voucher and in black ink circling the claim to be voided. Write “void” on the side of the remittance voucher and briefly explain why the void is requested. Sign and date the remittance voucher in the margin. Only one claim can be voided per copy of the remittance voucher. Additional claims on the same remittance voucher must be voided by submitting additional photocopies of the remittance voucher. Each copy of the remittance voucher can only have one claim circled on it.
What does it mean when a claim is voided?
Whenever a claim submission is successfully received by the payer, it begins processing right away. Simply deleting a submitted claim from your SimplePractice account will not delete the claim on the payer's end and the submission will continue to process as normal. In these instances, a voided claim can be used to indicate to the payer that they should stop processing the initial claim.
Where does the claim number come from when a claim is voided?
If the payer requires a voided/cancelled claim to be submitted, request the original claim number. This number will come directly from the payer.
What happens if you submit a claim and later determine that it was for an appointment that didn't occur?
If you submitted a claim and later determined that it was for an appointment that didn't occur, or if it listed incorrect information, you may need to void/cancel the original claim to stop the processing of the claim, or to allow you to submit a corrected version.
Can you delete a claim on SimplePractice?
Important: Deleting a claim from your SimplePractice account is permanent and deleted claims cannot be retrieved. Before deleting any claims, we recommend downloading them to save for your records and taking note of any reference numbers associated with the claim.
What is Medicare 935?
The limitation on recoupment (935), as required by Section 935 of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA) changes the process by which CGS can recoup an overpayment resulting from a post payment adjustment , such as a denial or Medicare Secondary Payer (MSP) recovery. For additional information, refer to the Medicare Financial Management Manual, (CMS Pub. 100-06), Ch. 3 §200.
What is the P B9997?
Claims/RAPs needing canceled must be in a finalized status/location (P B9997). Due to a change in the way FISS processes provider-submitted cancels to rejected claims, home health and hospice agencies will need to check FISS using Inquiry Option 12 to ensure their cancel has finalized prior to resubmitting the services to Medicare.
Can you adjust a P claim?
If a claim in a P status has been reviewed by Medical Review and has one or more line items denied, adjustments can be made to the paid line items. Please note: Adjustments cannot be made to any part of a denied line item on a partially paid claim.
Claim Corrections
- The claim correction process only applies to RTP claims. A claim correction may be submitted online via the Direct Data Entry (DDE) system.
- To access RTP claims in the DDE Claims Correction screen, select option 03 (Claims Correction) from the Main Menu and the appropriate menu selection under Claims Correction (21 – Inpatient, 23 – Ou...
- The claim correction process only applies to RTP claims. A claim correction may be submitted online via the Direct Data Entry (DDE) system.
- To access RTP claims in the DDE Claims Correction screen, select option 03 (Claims Correction) from the Main Menu and the appropriate menu selection under Claims Correction (21 – Inpatient, 23 – Ou...
- RTP claims remain in this location (TB9997) and are available for correction for 180 days.
- RTP claims are not finalized claims and do not appear on your Remittance Advice (RA). Therefore, you may submit a new (corrected) claim and it will not reject as a duplicate to the original claim.
Claim Adjustments
- The claim adjustment process is used to make corrections to processed or rejected claims. Adjustment claims may be submitted via DDE or your electronic software.
- Processed and rejected claims are finalized claims and appear on the RA. If a new claim is submitted, it will reject as a duplicate of the original claim.
- To determine the reason a claim/line item rejected, review the specific reason code assigned …
- The claim adjustment process is used to make corrections to processed or rejected claims. Adjustment claims may be submitted via DDE or your electronic software.
- Processed and rejected claims are finalized claims and appear on the RA. If a new claim is submitted, it will reject as a duplicate of the original claim.
- To determine the reason a claim/line item rejected, review the specific reason code assigned and/or the RA.
- Claim adjustments are subject to the same timely filing limit as new claims (i.e., within one calendar year of the "through" date of service on the claim). A justification statement is required if...
Claim Voids/Cancels
- The claim void/cancel process is only used if a processed claim should never have been submitted.
- To cancel a claim via DDE, select option 03 (Claims Correction) from the Main Menu and the appropriate menu selection under Claim Cancels (50 – Inpatient, 51 – Outpatient, 52 – SNF).
- Void/cancel claims must contain:
Clerical Error Reopenings
- The claim reopening process is available to correct clerical errors when the claim is beyond the timely filing limit.
- CMS defines clerical errors (including minor errors or omissions) as human or mechanical errors on the part of the provider or the contractor, such as:
- To request a claim reopening, complete the Clerical Error Reopening Request formand mail i…
- The claim reopening process is available to correct clerical errors when the claim is beyond the timely filing limit.
- CMS defines clerical errors (including minor errors or omissions) as human or mechanical errors on the part of the provider or the contractor, such as:
- To request a claim reopening, complete the Clerical Error Reopening Request formand mail it along with the corrected claim form to the J15 Part A Claims Department address listed on the form.
- To submit a claim reopening via DDE or your electronic software, please reference the following:
Overpayments
- MSP Overpayments
- Section 935 Overpayments If a full or partial overpayment is identified through the medical review process (i.e., due to a review by CGS, CERT, the Recovery Auditor, etc.):
Medical Review Additional Development Request
- The ADR process is used to notify you that a claim has been selected for medical review and is a request for you to send any medical documentation that supports the service(s) rendered and billed.
- CGS mails ADR letters to the correspondence address listed on the provider file (Section 2C of the CMS-855A form).
- The ADR process is used to notify you that a claim has been selected for medical review and is a request for you to send any medical documentation that supports the service(s) rendered and billed.
- CGS mails ADR letters to the correspondence address listed on the provider file (Section 2C of the CMS-855A form).
- To identify claims selected for medical review in DDE, select option 01 (Inquiries), option 12 (Claims), key the National Provider Identifier (NPI), tab to the S/LOC field, type SB6001, and press E...
- You may also identify claims selected for medical review and respond electronically in the myCGS Portal.
Redeterminations
- The redetermination process is the first level of appeal and applies to a claim or line item that receives a full or partial denial (identified as a claim in location DB9997 or a claim/line level r...
- If your claim was denied for non-receipt of records in response to an ADR (reason code 56900), or if you do not agree with a denial of a service, you may request a redetermination by completing the...
- The redetermination process is the first level of appeal and applies to a claim or line item that receives a full or partial denial (identified as a claim in location DB9997 or a claim/line level r...
- If your claim was denied for non-receipt of records in response to an ADR (reason code 56900), or if you do not agree with a denial of a service, you may request a redetermination by completing the...
- You may also complete the form and submit your documentation electronically in the myCGS Portal.
- Redetermination requests must be submitted within 120 days of the date on the Remittance Advice (RA).