What are the different parts of Medicare?
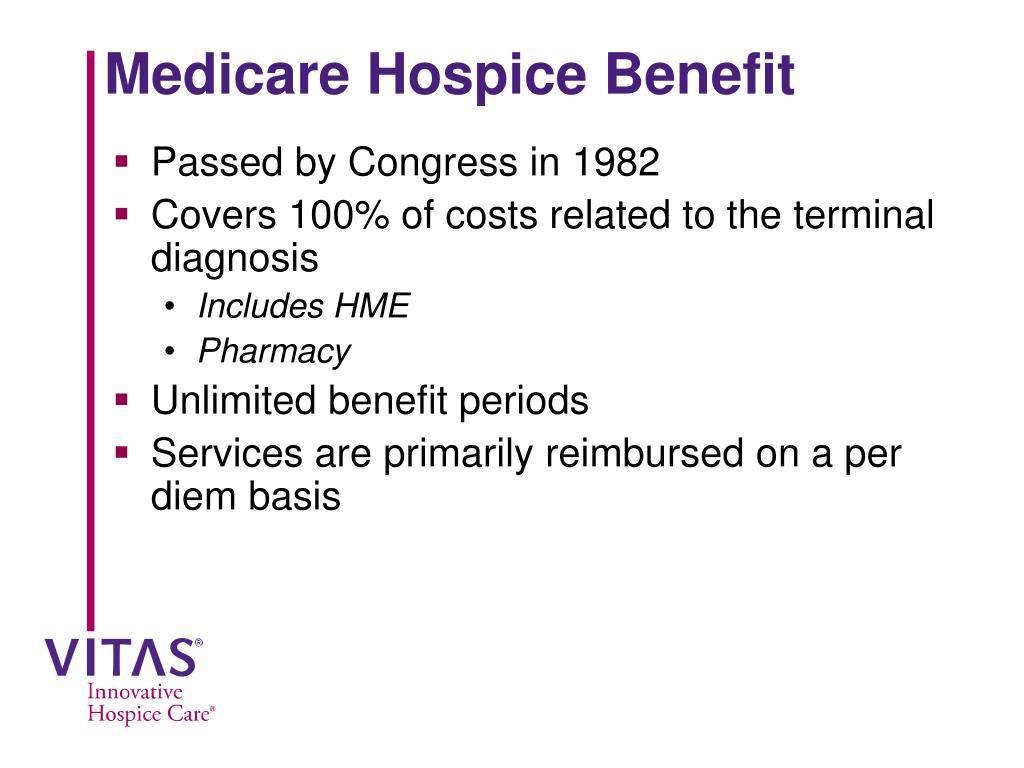
Medicare is divided into four Parts: A, B, C and D. Part A covers hospital (inpatient, formally admitted only), skilled nursing (only after being formally admitted to a hospital for three days and not for custodial care), and hospice services.
What is Medicare and how does it work?
The different parts of Medicare help cover specific services: Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. Medicare Part D (prescription drug …
What is the Medicare program?
a. Additional "private" insurance or Medicare supplement designed to pay for covered services in Medicare b. Insurance in which the state government matches the coverage of Medicare part B c. A joint federal and state program that helps cover low income individuals d. A federal assistance program to help provide payment for specialty services e.
What are the benefits of Medicare Part A?
Mar 22, 2021 · Diagnostic related groups, or DRGs, comprise a Medicare payment system designed to help control health care costs by paying hospitals a predetermined amount for each DRG. Learn more about how this system could affect your Medicare costs and coverage. by David Levine | Published March 22, 2021 | Reviewed by John Krahnert. A diagnosis related group, or …

Who is Medicare designed to assist?
Medicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
Who are the three groups covered by Medicare?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant).
What are the Medicare groups?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
Which group is covered under Medicare quizlet?
What is Medicare? Federal program that provides health insurance coverage to people ages 65 and older and younger people with permanent disabilities.
What are benefits of Medicare?
Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
Which of the following services are covered by Medicare Part B?
Medicare Part B helps cover medically-necessary services like doctors' services and tests, outpatient care, home health services, durable medical equipment, and other medical services.Sep 11, 2014
What is a Medicare group number?
Original Medicare is not a group policy, therefore there is no “group” in which to belong. Instead, you will see an 11-digit alphanumeric on your card which is used to identify you and file claims under your name. This is your Medicare number.Jan 20, 2022
What is Medicare quizlet?
Medicare is a social insurance program administered by the United States government, providing health insurance coverage to people who are aged 65 and over, or who meet other special criteria.
What is a Medicare accountable care organization?
What is an ACO? ACOs are groups of doctors, hospitals, and other health care providers, who come together voluntarily to give coordinated high-quality care to their Medicare patients.Dec 1, 2021
What are three groups of people covered by Medicare quizlet?
Medicare is the federal program that provides healthcare coverage for three groups of people. These groups are people over the age of 65, disabled persons, and end-stage renal disease patients of any age.
Which of the following does Medicare part A help pay for quizlet?
Medicare Part A provides coverage for inpatient hospital stays. Inpatient stays are those in which an individual must receive care or treatment in a hospital. Covered inpatient expenses include: semi-private room, meals, hospital services and supplies, drugs received during inpatient care, and general nursing services.
Which activity is covered by Medicare quizlet?
There are five main things that Medicare part A cover. What are they? In-patient hospitalization, skilled nursing facility care, In home care, hospice services, and blood.
What is Medicare for?
Medicare is the federal health insurance program for: 1 People who are 65 or older 2 Certain younger people with disabilities 3 People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
What is a medicaid supplement?
A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like copayments, coinsurance, and deductibles. Some Medigap policies also cover services that Original Medicare doesn't cover, like medical care when you travel outside the U.S.
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. at the start of each year, and you usually pay 20% of the cost of the Medicare-approved service, called coinsurance.
Does Medicare Advantage cover vision?
Most plans offer extra benefits that Original Medicare doesn’t cover — like vision, hearing, dental, and more. Medicare Advantage Plans have yearly contracts with Medicare and must follow Medicare’s coverage rules. The plan must notify you about any changes before the start of the next enrollment year.
Does Medicare cover prescription drugs?
Medicare drug coverage helps pay for prescription drugs you need. To get Medicare drug coverage, you must join a Medicare-approved plan that offers drug coverage (this includes Medicare drug plans and Medicare Advantage Plans with drug coverage).
What is the standard Part B premium for 2020?
The standard Part B premium amount in 2020 is $144.60. If your modified adjusted gross income as reported on your IRS tax return from 2 years ago is above a certain amount, you'll pay the standard premium amount and an Income Related Monthly Adjustment Amount (IRMAA). IRMAA is an extra charge added to your premium.
Do you pay Medicare premiums if you are working?
You usually don't pay a monthly premium for Part A if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A."
What is the DRG system?
One the one hand, the system prods hospitals to increase efficiency and use only the necessary treatments, to keep costs down. On the other hand, some hospitals may attempt to discharge patients as quickly as possible.
How does CMS penalize hospitals?
CMS is aware of these potential problems, and, in some circumstances, penalizes hospitals financially: 1 If a patient is re-admitted within 30 days–a sign that the patient may have been released too early. 2 If it discharges a patient to an inpatient rehab facility or to home with outside health support in order to discharge sooner. In this case, the hospital may have to share part of its DRG payment with that facility or provider.
What is a DRG?
A diagnosis related group, or DRG, is a way of classifying the costs a hospital charges Medicare or insurance companies for your care. The Centers for Medicare & Medicaid Services (CMS) and some health insurance companies use these categories to decide how much they will pay for your stay in the hospital. CMS and insurers have created metrics and ...
How does DRG work?
How DRGs Work. Medicare pays your hospital a pre-set amount for your care, which is based on your DRG or diagnosis. These payments are processed under what is known as the inpatient prospective payment system (IPPS). Medicare assigns you to a DRG when you are discharged from the hospital. The DRG is determined by your primary diagnosis, ...
How is DRG determined?
Medicare assigns you to a DRG when you are discharged from the hospital. The DRG is determined by your primary diagnosis, along with as many 24 secondary diagnoses. CMS determines what each DRG payment amount should be by looking at the average cost of the products and services that are needed to treat patients in that particular group.
What is the Tennessee State Health Insurance Assistance Program?
The Tennessee State Health Insurance Assistance Program is a statewide program that provides free and objective counseling and assistance to persons with questions or problems regarding Medicare and other related health insurances.
What is Sage Plus?
Aloha and welcome to the Sage PLUS Program website. We are Hawaii’s State Health Insurance Assistance Program (SHIP), a program that offers one-to-one counseling and assistance to people with Medicare and their families.
What is the glow program?
The SHINE Program (Serving the Health Insurance Needs of Everyone) is a state health insurance assistance program that provides free health insurance information, counseling and assistance to Massachusetts residents with Medicare and their caregivers.
What is HIICAP in New York?
HIICAP is the New York State SHIP that receives Federal Assistance from the Centers for Medicare and Medicaid Services (CMS) and the State of New York to educate the public about Medicare, Medicare Advantage plans and other health insurance issues.
What is a ship in Arizona?
SHIP is an independent program funded by federal agencies and is not affiliated with the insurance industry. This program is a partnership of the Department of Economic Security, Division of Aging and Adult Services and Arizona’s Area Agencies on Aging. Arkansas SHIIP.
What is HICAP in California?
California HICAP is part of a national network of State Health Insurance and Assistance Programs (SHIP). SHIP is a Federal grant program that helps States enhance and support a network of local programs, staff, and volunteers.
What is a Ship?
The State Health Insurance Assistance Program (SHIP or SHIIP) is a federally funded state program that has been providing free, local, one-on-one and sometime face-to-face medicare and health insurance counseling to Medicare Seniors. SHIP may have many different acronyms such as SHIIP, SHINE, HICAP, SHIBA, SHICK, but they all provide the same service. Remember if you are eligible for Medicare you are eligible for free counseling with SHIP. Please select your state below:
What is the Patient Protection and Affordable Care Act?
The Patient Protection and Affordable Care Act of 2010 includes a long list of reform provisions intended to contain Medicare costs while increasing revenue, improving and streamlining its delivery systems, and even increasing services to the program.
When did Medicare start?
But it wasn’t until after 1966 – after legislation was signed by President Lyndon B Johnson in 1965 – that Americans started receiving Medicare health coverage when Medicare’s hospital and medical insurance benefits first took effect. Harry Truman and his wife, Bess, were the first two Medicare beneficiaries.
How many people are covered by Medicare in 2019?
By early 2019, there were 60.6 million people receiving health coverage through Medicare. Medicare spending reached $705.9 billion in 2017, which was about 20 percent of total national health spending. Back to top.
Who signed Medicare into law?
Medicare’s history: Key takeaways. President Harry S Truman called for the creation of a national health insurance fund in 1945. President Lyndon B. Johnson signed Medicare into law in 1965. As of 2021, 63.1 million Americans had coverage through Medicare. Medicare spending is expected to account for 18% of total federal spending by 2028.
Is the Donut Hole closed?
The donut hole has closed, as a result of the ACA. It was fully eliminated as of 2020 (it closed one year early – in 2019 – for brand-name drugs, but generic drugs still cost more while enrollees were in the donut hole in 2019).
Can I get Medicare if I have ALS?
Americans younger than age 65 with amyotrophic lateral sclerosis (ALS) are allowed to enroll in Medicare without a waiting period if approved for Social Security Disability Insurance (SSDI) income. (Most SSDI recipients have a 24-month waiting period for Medicare from when their disability cash benefits start.)
What can a ship counselor do?
SHIP counselors can also help with Medicare coverage questions, problems and appeals if your health care or drug wasn't covered – either by Medicare or from a Medigap, Part D or Medicare Advantage plan.
Do you need to sign up for Medicare if you are 65?
SHIPs also provide help with Medicare sign-up issues. Unless you're already receiving early Social Security benefits at 65, you need to proactively sign up for Medicare. Your sign-up decisions can be complicated if you're still working past age 65 and have health insurance through your employer, especially if you lose your job ...
Is Medicare complicated?
Medicare can be complicated. It's easy to make mistakes when signing up that could result in lifelong penalties or coverage gaps, and people who lose their jobs after age 65 have an extra layer of complexity. Everyone on Medicare has the opportunity to choose a Medicare Part D or Medicare Advantage plan during open enrollment each year, ...
What is Medicare Supplement Insurance?
Medicare supplement insurance fills the gaps in coverage left by Medicare, which provides hospital and medical expense benefits for persons aged 65 and older. All Medicare supplement policies must cover 100% of the Part A hospital coinsurance amount for each day used from.
What is Medicaid in the US?
Medicaid is a federal and state program designed to help provide needy persons, regardless of age, with medical coverage. A contract designed primarily to supplement reimbursement under Medicare for hospital, medical or surgical expenses is known as. A) an alternative benefits plan. B) a home health care plan.
What is the core plan?
The benefits in Plan A, which is known as the core plan, must be contained in all other plans sold. Among the core benefits is coverage of Medicare Part A-eligible expenses for hospitalization, to the extent not covered by Medicare, from the 61st day through the 90th day in any Medicare benefit period.
How long does Medicare cover skilled nursing?
Medicare will cover treatment in a skilled nursing facility in full for the first 20 days. From the 21st to the 100th day, the patient must pay a daily co-payment. There are no Medicare benefits provided for treatment in a skilled nursing facility beyond 100 days. Medicare Part A covers.
What is intermediate care?
Intermediate care is provided under the supervision of a physician by registered nurses, licensed practical nurses, and nurse's aides. Intermediate care is provided in nursing homes for stable medical conditions that require daily, but not 24-hour, supervision. Tom is covered under Medicare Part A.
How old do you have to be to qualify for Medicaid?
To qualify for Medicaid nursing home benefits, an individual must be at least 65 years old, blind, or disabled; be a U.S. citizen or permanent resident alien; need the type of care that is provided only in a nursing home; and meet certain asset and income tests.