Fill out the Patient Request for Medical Payment form (CMS-1490S). You'll find the address for form submission in the instructions. Follow the instructions on the second page to submit the form to your carrier.
Full Answer
What do the letters after a Medicare number mean?
The most common letter at the end of a Medicare number is “A”. If you have the letter “A” at the end of your Medicare Number this means you have worked and paid into Social Security for at least 10 years to be entitled to receive Medicare. Government employees will see a “TA”. Disabled individuals will see a “HA” after their Medicare Number.
What is the letter after the Medicare number?
The Medicare number displayed on Medicare cards (known as an MBI, or Medicare Beneficiary Identifier) is 11 characters long: The 2nd, 5th, 8th and 9th characters are always a letter, and the 3rd and 6th characters are sometimes a letter.
What to do if Medicare denies your medical claim?
You can also take other actions to help you accomplish this:
- Reread your plan rules to ensure you are properly following them.
- Gather as much support as you can from providers or other key medical personnel to back up your claim.
- Fill out each form as carefully and exactly as possible. If necessary, ask another person to help you with your claim.
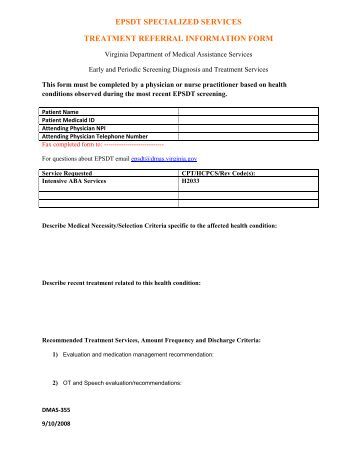
How to obtain Medicaid denial letter?
You can submit a letter stating that you were denied Medicaid or CHIP, and explaining the reason you can’t provide documents. Use this form, and fill out the "Denial of Medicaid or CHIP Coverage" section. When you complete the form, select "Letter of explanation" from the drop-down menu when you're on the upload documents screen in the application.
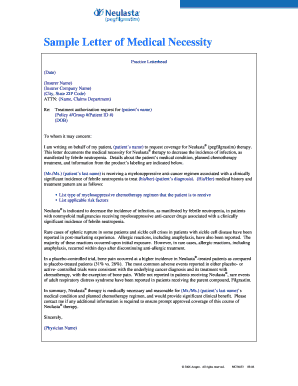
How do I submit a letter of medical necessity?
Dear [Pharmacy Director/Payer Contact Name]: I am writing on behalf of my patient, [Patient Name], to document the medical necessity to treat their [Diagnosis] with [Product Name]. This letter serves to document my patient's medical history and diagnosis and to summarize my treatment rationale.
How do I file medical necessity?
Documentation of medical necessity should do the following:Identify a specific medical reason or focus for the visit (e.g., worsening or new symptoms)Document the rationale for ordering tests or referrals.More items...•
How does Medicare prove medical necessity?
Proving Medical NecessityStandard Medical Practices. ... The Food and Drug Administration (FDA) ... The Physician's Recommendation. ... The Physician's Preferences. ... The Insurance Policy. ... Health-Related Claim Denials.
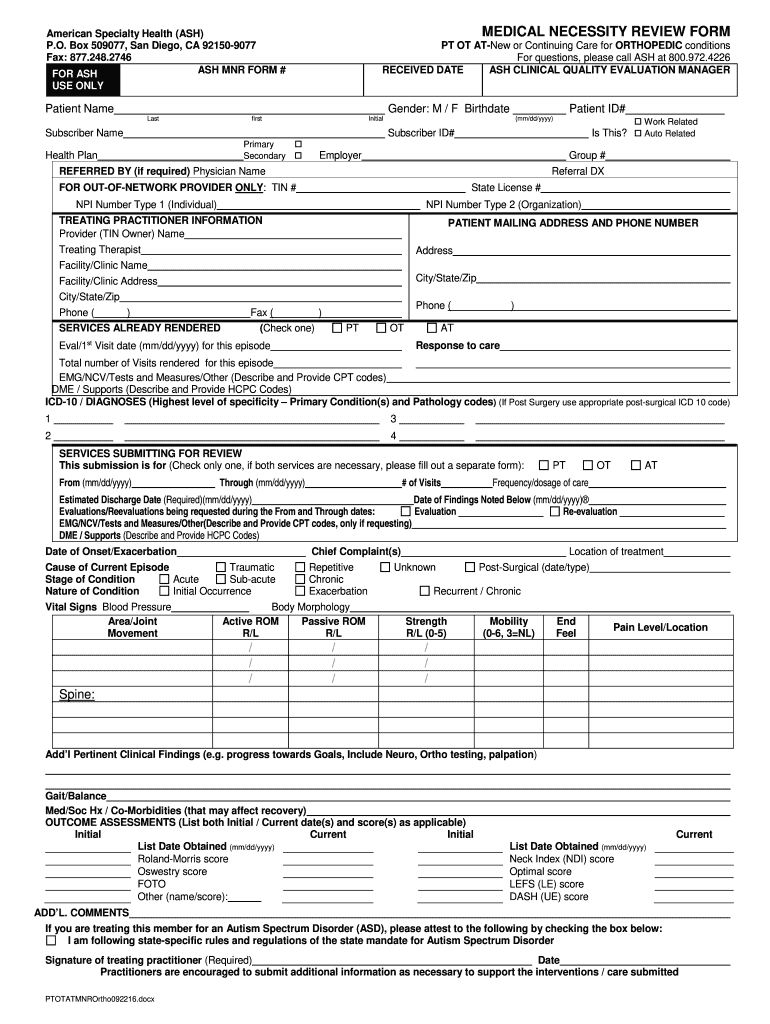
What is a CMN form for Medicare?
A Certificate of Medical Necessity (CMN) or a Information Form (DIF) is a form required to help document the medical necessity and other coverage criteria for selected durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) items.
How do you explain medical necessity?
"Medically Necessary" or "Medical Necessity" means health care services that a physician, exercising prudent clinical judgment, would provide to a patient. The service must be: For the purpose of evaluating, diagnosing, or treating an illness, injury, disease, or its symptoms.
What is an example of a medical necessity?
The most common example is a cosmetic procedure, such as the injection of medications, such as Botox, to decrease facial wrinkles or tummy-tuck surgery. Many health insurance companies also will not cover procedures that they determine to be experimental or not proven to work.
Can I submit CMS L564 online?
You can complete form CMS-40B (Application for Enrollment in Medicare – Part B [Medical Insurance]) and CMS-L564 (Request for Employment Information) online. You can also fax the CMS-40B and CMS-L564 to 1-833-914-2016; or return forms by mail to your local Social Security office.
Can a CMN be used as a written order?
The CMN can serve as the physician's detailed written order if the narrative description in section C is sufficiently detailed. This would include quantities needed and frequency of replacement for accessories and supplies.
How do I fill out a CMS L564?
1:328:29How to Fill Out CMS-40b Form and CMS-L564 Form - YouTubeYouTubeStart of suggested clipEnd of suggested clipName their address and course city state and zip you have to have one of these filled out for everyMoreName their address and course city state and zip you have to have one of these filled out for every employer. That you've had since 65..
Letter of Medical Necessity Sample
Janine Baker has recently been diagnosed with a rare form of lung disease, which causes great difficulty breathing and respiratory problems for the patient. The symptoms have gotten progressively worse, to the point where they are beginning to affect the lifestyle that Janine can live.
Letter of Medical Necessity for Speech Therapy Sample
My patient Mr. Shaun Lesley has suffered from hearing loss for five years after loud machinery damaged his inner ear at work. Though he can hear moderately well with a digital hearing aid, most sounds are still quiet and distorted to him.
Letter of Medical Necessity for Orthotics Sample
I am writing to request that my child patient Laurence Holwell, be granted coverage for the use of an orthotic device to correct a poorly developed bone in his left ankle, that over time will impede his ability to walk correctly and eventually cause a noticeable limp.
Letter of Medical Necessity for Physical Therapy Sample
I am writing to inform you that my patient of 10 years, Mrs. Bunting, who is covered by your medical insurance, was recently the victim of a fall at work and has a partially slipped disc in her back.
Letter of Medical Necessity for Wheelchair Sample
My 70 year old patient Dwight Morgan is suffering from severe arthritis of the legs and has just been diagnosed with spinal cancer. He is also weak throughout the body.
Letter of Medical Necessity for Bariatric Surgery Sample
My patient of 20 years, Mr. Jeff Delacey, is in dire need of bariatric surgery to reduce his weight and prevent several serious health problems, each in early stages of development.
Letters of Medical Necessity: Examples & Samples
These letters need to be thorough with all relevant information that the insurance company may need to decide. Request your healthcare provider to be as specific as possible with the details.
FAQs
A letter of medical necessity needs to include the following points to be appropriate.
Conclusion
We hope your search for a letter of medical necessity template ended here. You never know when the need for a LOMN arises. So, it’s best to be prepared with all the templates. This way, you can get done with the formalities in time and return to work soon.
What is a DIF in medical billing?
A DIF is completed and signed by the supplier. It does not require the cost, a narrative description of equipment or a physician's signature. For certain items or services billed to a DME MAC, the supplier must receive a signed CMN from the treating physician or a signed DIF from the supplier.
Do you have to maintain a copy of a faxed CMN?
It is in the supplier's interest to maintain a copy of what they faxed to the physician. Suppliers must maintain a copy of the completed CMN or DIF in their records. However, if the physician only faxes the front of the completed CMN then the supplier is only required to maintain the front portion of the CMN.
Do you have to send a CMN to a physician?
The CMN sent to the physician must be two-sided with instructions on the back. If the CMN is mailed to the physician, the supplier must send the two-sided form. If the CMN is faxed, the supplier must fax both the front and back of the form.
What is a letter of medical necessity?
A letter of medical necessity, abbreviated as LOMN, is a form or letter your doctor fills out stating that the medication or service prescribed is necessary for your health. Your doctor would submit it to the insurance company to be reviewed from there.
What happens if you fill out a letter of medical necessity?
For a letter of medical necessity to be accepted by the insurance, certain information has to be filled out correctly. If there is any misinformation or if the doctor fills out the incorrect form, then the insurance will most likely reject it. Here is the typical information that is needed for this legal document.
What to do if you are denied medical insurance?
You should keep a copy of the letter of medical necessity for your own records as well.
What information is included in a patient identification letter?
The patient identification will include the patient’s name, date of birth, and insurance information such as group and policy number. The date that the letter was written should also be included.
What is the diagnosis of what led up to the need for the treatment being prescribed?
The diagnosis of what led up to the need for the treatment being prescribed has to be very specific. Stating that the patient has general pain, or a heart condition will not suffice. If the patient has diabetes, then the specific type of diabetes should be stated.
How long does it take for a doctor to sign a prescription?
The insurance company will then have a team of professionals review the letter, which can take three to four days.
What is supporting literature?
Supporting Literature. Any information that would support the patient’s need for the treatment should be added. This would be including any other publications supporting the letter of medical necessity, as well as any lab or test results. Providing lab results gives hard evidence of the severity of the medical condition.
What is medical necessity?
The APTA’s definition of medical necessity (as detailed in this source) addresses the authority, purpose, scope, evidence, and value of the provided treatment. Per the APTA, physical therapy treatment is medically necessary if: A licensed PT determines it is so based on an evaluation;
Why is documentation important in medical care?
Documentation is a cornerstone of ensuring not only high care standards, but also accurate payment—and keeping it defensible it is the key to documenting for medical necessity.
Is APTA medical necessity strict?
The APTA’s definition of medical necessity is actually a little more strict than CMS’s—but that’s not necessarily a bad thing. The more thorough your documentation, the better. And if you adhere to the most stringent standards of medical necessity, your chances for claim denials drop substantially.
What Is The Letter of Medical Necessity?
Can A Patient Write It?
- A patient can write the letter, but it needs to be made official by a doctor. Any arguments for any service ultimately have to come from a treating physician. That means the doctor needs to know you, have some history with you, and in the end either write or ‘sign off on’ the letter.
Medical Need
- The LOMN must show medical need. For instance, the service in question will (or is reasonably expected to) 1. prevent the onset of an illness or a disability 2. reduce or improve the effects of an illness or disability 3. achieve (or maintain) the maximum functional capacity of the specific patient in performing daily activities given age and baseline functionality. In other words, ‘withou…
Appeals
- The letter of medical necessity is a LEGAL document and patients need legal supportagainst giant corporations that want to spend as little as possible on care. It is the formal medical judgement of a licensed physician as to why a patient needs a specific treatment and why other treatments are not appropriate. An insurer may still deny the treatment, but the LOMN is your best chance at get…