How does Medicare pay for mdpp?
If requirements are met, Medicare will pay the MDPP supplier or its billing agent (if applicable). Additionally, the MDPP supplier is held accountable for compliance with all appropriate regulations and requirements, regardless of its use of a third party entity.
Do I need a new billing system for the mdpp?
Yes. Existing providers with a billing system can continue to use that system for submitting claims to Medicare and are not required to purchase or establish additional infrastructure specifically for the MDPP expanded model.
Can I bill Medicare for mdpp and DSMT services simultaneously?
Yes, under certain circumstances, organizations may offer MDPP services in addition to MNT and DSMT services and bill Medicare concurrently. MDPP suppliers can only bill for MDPP services under their MDPP enrollment.
Can the FQHC/RHC bill Medicare for mdpp services?
Once enrolled as an MDPP supplier, the FQHC/RHC may bill Medicare for MDPP services, but only using the MDPP HCPCS G-codes that were finalized in the CY2018 Physician Fee Schedule final rule (see table in response to question 17). MDPP services would be billed using a separate NPI on a CMS-1500 paper claim form or its electronic equivalent.
What is Medicare Mdpp coverage?
The MDPP is covered under Medicare Part B as a preventive service once per lifetime. Medicare cost sharing does not apply to MDPP services. Benefit description: Core services period is 12 months: 16 weekly core sessions over months 1-6, and 6 monthly core maintenance sessions in months 6-12.
Does Medicare pay for DPP?
You pay nothing for this program if you're eligible. The Medicare Diabetes Prevention Program is a proven health behavior change program to help you prevent type 2 diabetes. The program begins with 6 months of weekly group sessions.
What is a Mdpp supplier?
Medicare Diabetes Prevention Program (MDPP) Supplier Requirements Checklist. Organizations should use this checklist as a tool to understand the requirements to enroll and maintain enrollment as MDPP suppliers.
How do I get Medicare diabetes Prevention Program?
There are two steps to become a Medicare Diabetes Prevention Program Supplier. Submit an application online to become a CDC- recognized organization. The process is handled by CDC. Offer group-based sessions to help participants eat healthier, lose weight, and increase physical activity.
Does Medicare cover diabetic medicine?
Medicare covers various diabetes medications, supplies and services to help treat diabetes and keep your blood glucose in a healthy range. Medicare Part B covers blood glucose testing and other supplies you may need plus some medical and education services.
Are diabetes prevention programs free?
USPM Offers a Free Online Diabetes Prevention Program As a DPP provider, USPM partners with employers, health insurance payors, and other organizations to make our lifestyle change program available to as many at-risk individuals as possible. In many cases, your participation may be 100% free to you.
How long is diabetes prevention program?
1 yearOver the course of 1 year, CDC-recognized lifestyle change programs offer about 24 hours of instruction to lower your patients' risk of type 2 diabetes by more than half. There are also online programs available for patients who have difficult schedules or mobility and transportation issues.
What benefits are diabetics entitled to?
Type 2 diabetes can cause severe complications that may make a person eligible for disability benefits. There are two types of benefits: SSDI, which requires a qualifying length of time in work, and SSI, which can support people with disabilities at any age and time in their work career.
Is prediabetes covered by insurance?
However, Medicare and most insurance plans cover diabetes testing for people suspected of having diabetes. People at risk for diabetes are also at risk for pre-diabetes. Since the test is the same and the risk factors are the same for both conditions, a prediabetes test may be covered.
When is the MDPP quarterly due date?
This means that the MDPP supplier will have furnished services for six months on March 1, 2019. The next quarterly due date after March 1 is April 15; therefore, the MDPP supplier’s first crosswalk file is due on April 15, 2019.
How many sessions can a beneficiary attend in MDPP?
Once the MDPP services period is initiated through attendance at the first core session, there are no attendance requirements for beneficiaries to attend core sessions or core maintenance sessions in months 0-12. During months 0-12, a beneficiary can attend as many or as few sessions as he or she wishes.
What is a MDPP crosswalk?
MDPP suppliers are required to maintain a crosswalk file, which lists MDPP crosswalk data, including beneficiary identifiers used for the Centers for Disease Control and Prevention (CDC) performance data submissions, and the corresponding Medicare identifiers for each beneficiary who receives MDPP services.
How long does it take to get a CDC recognition?
How long does it take to obtain MDPP preliminary or full CDC recognition?#N#It takes at least 12 months to obtain CDC Preliminary Recognition and up to 24 additional months to achieve Full Recognition. Preliminary recognition requires a submission of 12 months of data from a National DPP cohort. Full CDC recognition requires that organizations deliver the year-long diabetes prevention lifestyle change program with fidelity to all CDC Diabetes Prevention Recognition Program (DPRP) Standards. This recognition status could be achieved within 36 months if all requirements are met. All requirements to achieve CDC Full Recognition status are listed in the CDC DPRP standards and include using a CDC-approved curriculum, meeting attendance-based requirements, and meeting standards related to the rate at which participants achieve the final 5 percent or more weight loss goal.
When is the MDPP crosswalk file due?
The quarterly due dates are: January 15, April 15, July 15, and October 15. For example, an MDPP An MDPP supplier begins furnishing services on September 1, 2018.
When should a CMS crosswalk be provided?
The crosswalk should be supplied to CMS beginning 6 months after the organization begins furnishing MDPP services, and quarterly thereafter. The crosswalk would be maintained in a spreadsheet (for example, an Excel file or a CSV file), in a form and manner specified by CMS.
Can you bill Medicare for MDPP?
No, enrolled MDPP suppliers can only bill Medicare for MDPP services furnished on or after April 1, 2018 according to their effective date of billing privileges. For approved enrollment applications submitted prior to April 1, 2018, the effective date of billing privileges will be April 1, 2018.
What is MDPP in Medicare?
Medicare Diabetes Prevention Program (MDPP) The Medicare Diabetes Prevention Program expanded model is a structured intervention with the goal of preventing type 2 diabetes in individuals with an indication of prediabetes. The clinical intervention consists of a minimum of 16 intensive "core" sessions of a Centers for Disease Control ...
What is the minimum BMI for Medicare?
Enrolled in Medicare Part B. Have a body mass index (BMI) of at least 25 (or at least 23 if self-identified as Asian) At first core session, height and weight must be measured in person and used to calculate BMI. Met one of the following three blood test requirements within the 12 months of first core session.
What is the purpose of the DPP?
The purpose of this section is to provide a framework to ensure the National Diabetes Prevention Program (DPP) lifestyle change program is reimbursed appropriately and in a timely manner. Submitting improper codes or claims to payers may result in non-payment or added time and expense for re-submission of the claim or invoice.
What is CPT code?
Current Procedural Terminology (CPT) Codes are a group of procedure codes used in medical billing. These codes were created by the American Medical Association (AMA) in 1996 to standardize reporting of medical, surgical, and diagnostic services and procedures and serve as a common language between providers and payers.
How often is 0488T billable?
The 0488T code is only billable once per 30 days, so typically the payment associated with 0488T would be higher than the payment for 0403T (see the Oregon example below). Neither of these codes should be used for individuals with established diabetes.
What is the HCPCS level 2 code?
If Medicare or Medicaid is the payer, the HCPCS code and its modifiers may be used (level III codes listed below). Level II codes are the HCPCS (alphanumeric) code set and are primarily concerned with products, supplies, and procedures that are not covered by the CPT codes.
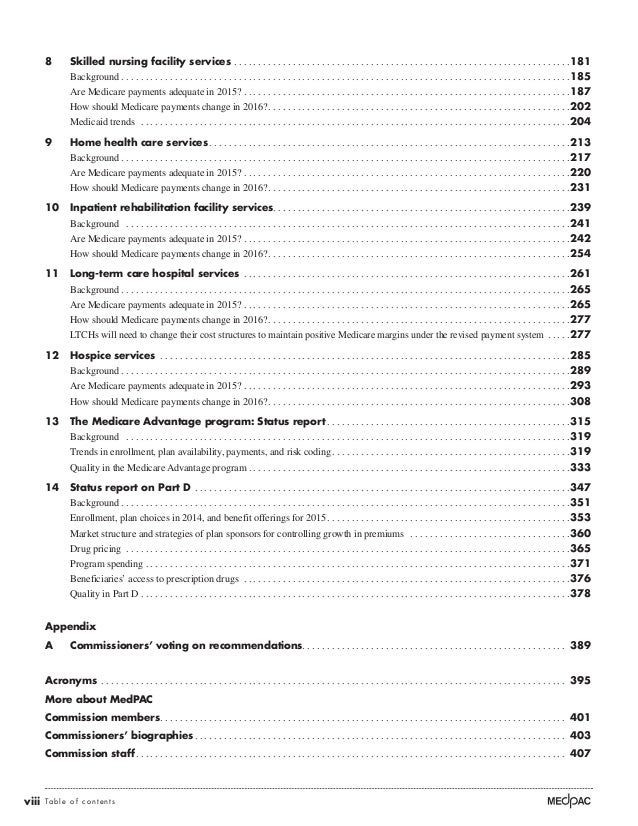
What is Medicare Advantage Plan?
There are two main ways for beneficiaries to receive Medicare coverage—Original Medicare(Part A and Part B benefits) or aMedicare Advantage plan (Part C), which is a type of Medicare health plan offered by a private company that contracts with Medicare to provide, at a minimum, Part A and Part B benefits. Medicare Advantage (MA) plans may also offer coverage of supplemental health benefits that are not covered by Medicare Parts A or B.
Do MA plans cover Medicare?
MA plans must provide enrollees with all Medicare Part A and Part B services. MA plans that limit enrollees to a specified network of providers and suppliers must ensure that all Medicare-covered services are available and accessible under the plan. In order to do so, MA plans will need to contract with Medicare-enrolled MDPP suppliers to provide MDPP services to their enrollees or the MA plan may enroll in Medicare as an MDPP supplier itself. MDPP services rendered to enrollees in-network must be provided without cost-sharing. MA plans that permit enrollees to use out-of-network providers and suppliers may require enrollees to pay cost-sharing for MDPP services furnished out-of-network; however, MA plans are still required to cover MDPP services without cost-sharing if MDPP services cannot be provided in-network because there is no in-network provider.
Can Medicare Advantage beneficiaries receive MDPP?
Medicare beneficiaries, including Medicare Advantage enrollees, who meet MDPP eligibility requirements are entitled to receive only one set of MDPP services in their lifetime. MA plans have the option to offer, as a supplemental benefit, an extended length of coverage for these services. MA plans may also offer, as supplemental benefit, diabetes prevention services in a 100% virtual format and other types of prediabetes services that do not qualify as MDPP services; however, we note that services offered as a supplemental benefit are not MDPP services, and cannot be used as a substitute for the provision of MDPP services under Part B. To aid MDPP suppliers in complying with the once-per-lifetime coverage requirement, CMS is exploring how existing systems can be used to verify whether beneficiaries have previously received MDPP services through Original Medicare, and intends to release additional details on this support in the future. MDPP suppliers may need to rely on beneficiary attestation or information from the MAO to determine whether a beneficiary has previously received MDPP services under Part C coverage.