Under MIPS, the three categories that require submission of data (Quality, Promoting Interoperability and Improvement Activities) can be submitted through a single vendor. You may also mix and match submission data and group/individual submissions and CMS will credit you with whichever score is highest.
Full Answer
What does MIPS stand for in Medicare?
Medicare's current quality reporting programs are being consolidated and streamlined into 1 merit-based incentive payment system, referred to as "MIPS." This consolidation will reduce the aggregate level of financial penalties physicians otherwise could have faced, and it also provides a greater potential for bonus payments.
What is the MIPS payment adjustment for Medicare Part B?
The MIPS score earned by a clinician or group for the performance period determines the adjustment applied to every Medicare Part B payment to the clinician. The payment adjustment occurs in the second calendar year after the performance year. So, for PY2021, the payment adjustment would occur beginning with 2023 reimbursements.
When can I submit MIPS data for 2019 to Medicare?
MIPS data for 2019 can be submitted to Medicare at any time up until March 31, 2020 [8 pm EDT] when the submission window closes. See the Quality Payment Program (QPP) website for the 2019 MIPS Scoring Guide & 2019 MIPS 101 Guide.
Are outpatient diagnostic services subject to MIPS payment adjustments?
Radiology and other diagnostic services furnished to hospital outpatients are paid under the Outpatient Prospective Payment System (OPPS) to the hospital and aren’t subject to MIPS payment adjustments. Q: Are payments for anesthesiology services subject to 2022 MIPS payment adjustments?

How do I report MIPS?
Clinicians who are both MIPS APM participants and who are MIPS eligible at the individual or group level can report to traditional MIPS and/or report to MIPS via the APM Performance Pathway (APP). Qualifying APM Participants (QPs) and Partial QPs who elect not to report to MIPS, aren't required to report to MIPS.
How does Medicare MIPS work?
The Merit-Based Incentive Payment System (MIPS) is the program that will determine Medicare payment adjustments. Using a composite performance score, eligible clinicians (ECs) may receive a payment bonus, a payment penalty or no payment adjustment.
Do I need to report MIPS?
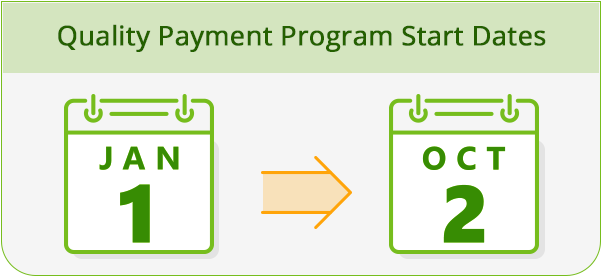
The 2022 MIPS quality category has a full-year performance period ranging from January 1, 2022 – December 31, 2022. This year, physicians may choose to report data on quality measures at the individual, group, or Virtual Group level using one reporting mechanism.
What is the deadline for MIPS submission?
March 31 is the deadline for MIPS-eligible clinicians who participated in the 2021 performance year of the Quality Payment Program to get their data into CMS and avoid penalties.
How does MIPS payment adjustment work?
A MIPS eligible clinician with a Final Score of 85 points or higher will receive an additional payment adjustment factor for exceptional performance. The MIPS payment adjustment factor(s) are determined by the MIPS eligible clinician's Final Score.
What are the MIPS requirements?
2022 Low Volume Threshold Participation in MIPS is required if, in both 12-month segments of the MIPS Determination Period if: Excluded individuals or groups must have ≤ $90,000 Part B allowed charges OR ≤ 200 Part B patients OR ≤ 200 covered professional Part B services.
What happens if you dont report MIPS?
What happens if I choose not to report any data to MIPS? Unless you qualify for an exemption from MIPS in 2022, you will receive a -9% payment adjustment to your Medicare Part B fee-for-service (FFS) claims in 2024.
What is the penalty for not reporting MIPS?
Penalties for failing 2021 MIPS range up to 9% levied on your 2023 Part B professional service reimbursements. Penalty avoidance strategies can be split based on whether or not you are going to report the Promoting Interoperability (PI) category and whether or not you will be picked up in the Cost performance category.
Is MIPS reporting only for Medicare patients?
MIPS reporting of individual measures applies to all patients. Eligibility for a measure is based on CMS documentation (denominator criteria).
What is the deadline for 2021 MIPS reporting?
MIPS 2021—Key Dates for Performance Year 20212020March 31Last day to submit 2021 MIPS data if reporting directly to the CMS QPP attestation portal.JulyCMS will provide you with feedback based on your 2021 performance year data. Targeted review starts after release of feedback data.Aug. 31Targeted review ends.20 more rows
What are CMS reports?
The cost report contains provider information such as facility characteristics, utilization data, cost and charges by cost center (in total and for Medicare), Medicare settlement data, and financial statement data. CMS maintains the cost report data in the Healthcare Provider Cost Reporting Information System (HCRIS).
What does Macra stand for?
Medicare Access and CHIP Reauthorization Act of 2015The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) is a bipartisan legislation signed into law on April 16, 2015. MACRA created the Quality Payment Program that: Repeals the Sustainable Growth Rate (PDF) formula. Changes the way that Medicare rewards clinicians for value over volume.
When will Medicare release MIPS data?
MIPS data for 2019 can be submitted to Medicare at any time up until March 31, 2020 [8 pm EDT] ...
What is MIPS in Medicare?
The Merit-based Incentive Payment System (MIPS) implemented by the Centers for Medicare & Medicaid Services (CMS) is the result of the Medicare Access & CHIP Reauthorization Act of 2015. This mandate established the Quality Payment Program (QPP) as part of medical billing reform related to Obamacare, originally passed as the Affordable Care Act ...
How many CAHPS are needed for MIPS?
The CAHPS for MIPS Survey. The minimum number of documented sources from small scale medical practitioners and healthcare institutions is six in 2019. For clinics with more than 16 physicians, the minimum requirement is 200 peer-reviewed statistical samples.
What is the minimum MIPS score for 2020?
Medical institutions need to keep a minimum score of 45/100 in 2020 and 60/100 in 2021 to avoid any penalties under the new MIPS guidelines established by the CMS for submission methods. The MIPS score is also used for the Medicare & Medicaid quality payment program systematics within a socially-distributed public dispensary ...
What is MIPS in Medicare?
Medicare's legacy quality reporting programs were consolidated and streamlined into the Merit-based Incentive Payment System, referred to as "MIPS." This consolidation reduced the aggregate level of financial penalties physicians otherwise faced, and it also provides a greater potential for bonus payments.
Does Medicaid include CDS?
However, the Medicaid Meaningful Use program continues to include CPO E and CDS measures. While CPOE and CDS functionality will still be included in EHRs, CMS will no longer require a certain number of orders, that a physician enter the orders, and that physicians implement a certain number of CDS tools.
Does Medicare have CPOE?
Following years of advocacy by the AMA, the Centers for Medicare and Medicaid Services (CMS) has removed the computerized physician order entry (CPOE) and clinical decision support (CDS) measures from the Medicare MU program and the ACI component of the Quality Payment Program (QPP). However, the Medicaid Meaningful Use program continues to include CPOE and CDS measures.
What Are Case Units for MIPS Quality Measures?
In every quality measure, a measure case has a particular unit. These units include patients, periods, episodes, encounters/visits, and procedures. These units also determine when it is too late to complete a measure within the performance period (figure 6).
What Are Collection Types for MIPS Quality Measures?
CMS defines collection types as “a set of quality measures with comparable specifications and data completeness criteria.” The key word in that definition is “specifications.” The word “specifications” is key because measure specifications dictate what data in your PM or EHR can be used to calculate measure results.
How CMS Calculates Bonus Points for MIPS Quality Measures
I n addition to measure achievement points, your measures may earn bonus points. You earn bonus points on both your highest-performing six measures and any additional measures you submit that qualify.
Differences Between Measures
Some measures require clinicians to document several data points. Other measures don’t. Balance the opportunity and the opportunity cost of each measure.
Differences Between Submission Methods for the Same Measure
Different submission methods use different data fields for the same measure. This question returns to an image shown previously in this guide:
Additional Reading
Would you like to learn more about this topic? Here are some articles we suggest:
PowerPoint Slides
Would you like to use or share these concepts? Download the presentation highlighting the key main points.
When does CMS publish MIPS scores?
MACRA requires CMS to publish each eligible clinician’s annual MIPS score and performance category scores within approximately 12 months after the end of the performance year.
When will MIPS be applied to a new organization?
For example, if a clinician earns a MIPS score for 2021 and moves to another organization in 2022, the new organization will inherit the MIPS payment adjustment applied in 2023 based on the 2021 score earned by the clinician at the previous organization.
How many records are needed for a measure to be scored?
Measures must have at least 20 records in the denominator (and contain at least 70% of eligible cases) to be scored against national benchmarks (e.g. receive a score higher than 3 points). A clinician may choose to report a specialty measure set, defined by CMS for a particular specialty.
How is each measure scored?
Each measure is scored on performance based on the submission of a numerator and denominator or a “yes or no”. Must submit a numerator of at least 1 or a “yes” to fulfill the required measures. The scores for each of the individual measures are added together to calculate a final score.
How many solo practitioners can join a virtual group?
But, there are no limits on how many solo practitioners and groups can join a virtual group. If a group chooses to join a virtual group, all of the eligible clinicians in that group have to be included in the virtual group. Any group that wants to be part of a virtual group must have 10 or fewer eligible clinicians.
Do you have to be individually eligible for MIPS?
At least 1 clinician must be individually eligible for MIPS. Important: The decision to report individually or as a group, applies across all MIPS categories for a given performance year. A clinician cannot choose to report as an individual in some categories while reporting as a group for other categories.
Is there a CMS enrollment process?
There is no CMS enrollment process or deadline f or reporting as a group. An organization must include the data from all the clinicians in the group, including clinicians who are otherwise excluded from MIPS individually due to low volume, newly Medicare enrolled status or QP status from an Advanced APM.