Medicare Part D drug benefit eligibility. If you are eligible for Medicare coverage, you are also eligible for the Medicare drug benefit ( Part D ). You must be enrolled in Medicare Part A and/or Part B to enroll in Part D. Medicare drug coverage is only available through private plans.
Full Answer
Who has the best Medicare Part D plan?
Jul 24, 2021 · To be eligible for Medicare, you need to be either a U.S. citizen or a legal resident with a green card. Permanent legal residents must live in the country for at least five consecutive years. Not only that, five of those years must immediately precede their application to …
Who qualifies for a Medicare Part D prescription drug plan?
Qualifying for Medicare Part D To be eligible for a Medicare Part D plan, you must first be enrolled in Medicare Part A and Part B. Thus, you must be eligible for Medicare. To be eligible for Medicare, you must be either 65 or older or have a disability and receive disability benefits for at least 24 months.
What are the qualifications for Medicare Part D?
Jul 24, 2021 · Medicare Part D eligibility is dependent on Medicare Part A and Part B enrollment. To be eligible for Medicare Part D, you must first enroll in Medicare Part A, Medicare Part B, or both. Medicare Part D provides beneficiaries with coverage for the cost of prescription drugs. For many, prescription medications are an essential element in maintaining a healthy lifestyle.
What are the rules of Medicare Part D?
Mar 07, 2022 · Eligibility For Part D Below are the qualifications for Medicare Part D. A. You’re aged 65 years or older and enrolled in Medicare Part A and B. B. You’ve received your Social Security disability payments for at least 2 years. C. You are diagnosed with end-stage renal disease or kidney failure.
Why is Medicare Part D important?
For many, prescription medications are vital to maintaining a healthy lifestyle. The costs of medications can drain finances, Medicare Part D prescription helps those who need assistance with medications .
What happens if you don't enroll in Medicare Part D?
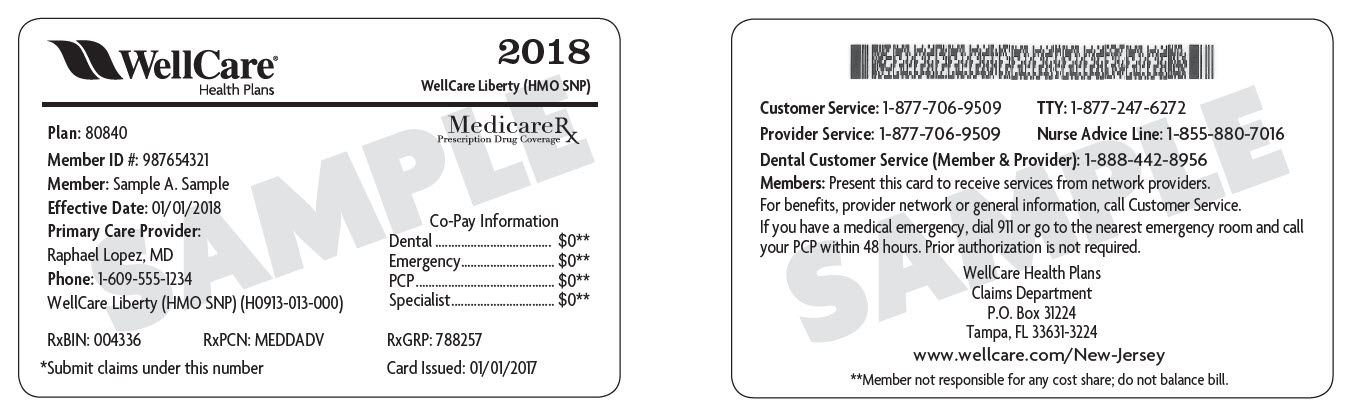
If you don’t enroll when you’re first eligible and don’t have creditable coverage, you could face a late enrollment penalty. Let’s take a closer look at using an example. Tip: Medicare Plan D and Part D aren’t the same things.
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare.
Is Medicaid a federal or state program?
Medicaid is another Federal and State government medical health insurance program. Medicaid provides coverage for individuals and families that have low incomes or limited resources. Not all will qualify for Medicaid coverage in addition to Medicare coverage. Medicare beneficiaries with full Medicaid benefits are dually eligible.
Does Medicare add late enrollment penalties?
Medicare may add a Part D Late Enrollment Penalty to your Part D premium each month you have Part D coverage. Unless you enroll in a Part D plan when you’re first eligible during your IEP.
What is Medicare Part D?
Medicare Part D is an important benefit that helps pay for prescription drugs not covered by original Medicare (parts A and B). There are private medication plans that you can add to your original Medicare coverage, or you can choose a Medicare Advantage plan (Part C) with drug coverage.
When do you have to enroll in Medicare Part D?
For most people, you first become eligible to enroll in Medicare Part D from 3 months before your 65 th birthday to 3 months after your birthday. When you find a plan to join, you’ll need to provide your unique Medicare number and the date you became eligible.
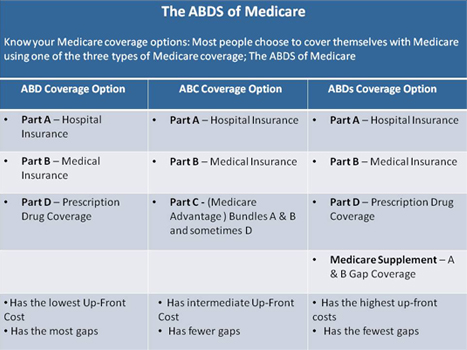
What are the different types of Medicare coverage?
What are the Medicare prescription drug coverage options? 1 Part D. These plans cover prescription medications for outpatient services. All plans have to offer some basic level of drug coverage based on Medicare rules. Specific plan coverage is based on the plans’ formulary, or drug list. If your doctor wants a drug covered that’s not part of that plan’s list, they’ll need to write a letter of appeal. Each nonformulary medication coverage decision is individual. 2 Part C (Advantage plans). This type of plan can take care of all your medical needs (parts A, B, and D), including dental and vision coverage. Premiums might be higher and you might have to go to network doctors and pharmacies. 3 Medicare supplement (Medigap). Medigap plans help pay for some or all out-of-pocket costs like deductibles and copays. There are 10 plans available. You can compare the rates and coverage with your original Medicare coverage gap and premiums. Choose the best option to give you maximum benefits at the lowest rates.
What is a Part C plan?
Part C (Advantage plans). This type of plan can take care of all your medical needs (parts A, B, and D), including dental and vision coverage. Premiums might be higher and you might have to go to network doctors and pharmacies. Medicare supplement (Medigap).
How old do you have to be to qualify for Medicare?
To be eligible for Medicare, you must qualify in one of the following ways: You’re age 65 and you can enroll in Medicare parts A and B. You’ve received Social Security disability payments for at least 2 years. The waiting period for Medicare is waived if you receive a diagnosis of amyotrophic lateral sclerosis (ALS).
What is Medicare Supplement?
Medicare supplement (Medigap). Medigap plans help pay for some or all out-of-pocket costs like deductibles and copays. There are 10 plans available. You can compare the rates and coverage with your original Medicare coverage gap and premiums.
How long do you have to be on disability to receive Part D?
If you’re not 65 but have a disability that qualifies you to receive Social Security or Railroad Retirement Disability benefits, you’re eligible for Part D 3 months before the 25 th month of benefit payments until 3 months after your 25 th month of receiving benefits.
