Average Medicare payments increase significantly with the number of chronic conditions. Finally, we quantify the effect of individual conditions and find that "Stroke / Transient Ischemic Attack" and "Chronic Kidney Disease" are the costliest chronic conditions for Part A, and "Cancer" and "Chronic Kidney Disease" are the costliest for Part B.
What are the most common chronic conditions in Medicare beneficiaries?
Results: We find that the effect of chronic conditions on Medicare payments is dramatic. Average Medicare payments increase significantly with the number of chronic conditions. Finally, we quantify the effect of individual conditions and find that "Stroke / Transient Ischemic Attack" and "Chronic Kidney Disease" are the costliest chronic conditions for Part A, and "Cancer" and …
What is the CPT code for chronic care management?
About 41% of Part B beneficiaries have two or more chronic conditions and these beneficiaries account for approximately 70% of total Part B payments in both years. • Total Medicare payments for Part B benefits increased by 10.7% between 2008 and 2010. 76% of the increase ($9.2 billion) was for the care of those with 2 or more chronic conditions.
Why is Medicare spending on health care increasing?
Results: We find that the effect of chronic conditions on Medicare payments is dramatic. Average Medicare payments increase significantly with the number of chronic conditions. Finally, we quantify the effect of individual conditions and find that “Stroke / Transient Ischemic Attack” and “Chronic Kidney Disease” are the costliest ...
How to Bill chronic care management 99490 to Medicare?
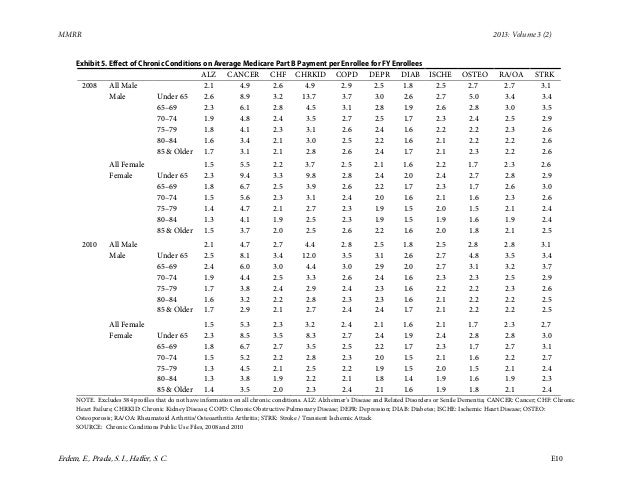
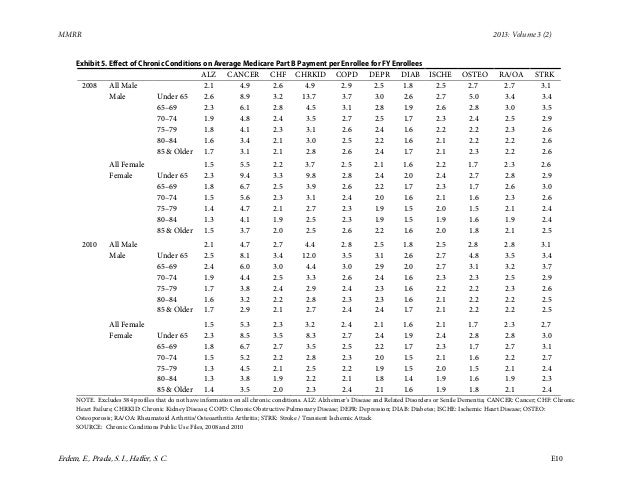
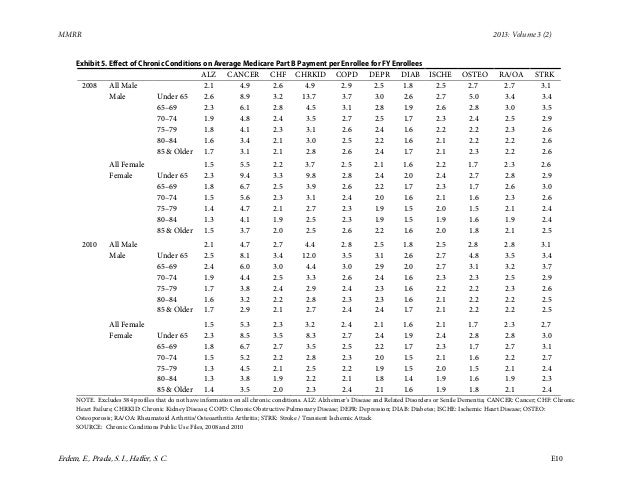
Jun 18, 2013 · The values in the tables provide the ratio of average payment with exactly one chronic condition and average payment without any chronic conditions. For example, having “Alzheimer's/Senile Dementia” increases the average Medicare payment for Part A by a factor of 7.3 for male enrollees who are in the under 65 age category in 2008.
What is considered a chronic condition for Medicare?
If you have 2 or more serious chronic conditions (like arthritis and diabetes) that you expect to last at least a year, Medicare may pay for a health care provider's help to manage those conditions. You pay a monthly fee, and the Part B.
How Much Does Medicare pay for CCM?
CCM is covered under Medicare Part B. This means that Medicare will pay 80 percent of the cost of service. You'll be responsible for a coinsurance payment of 20 percent.Apr 7, 2020
How many Medicare beneficiaries have 2 or more chronic conditions?
Chronic conditions are common among the Medicare population, with a significant share living with at least one chronic disease (Exhibit 1). Of all non-dual-eligible Medicare beneficiaries in 2017, 66 percent were living with two or more chronic conditions.Mar 18, 2021
Which conditions are considered chronic by Centers of Medicare and Medicaid Services?
Inquiries regarding this data can be sent to [email protected] Conditions.Alcohol AbuseDrug Abuse/ Substance AbuseCancer (Breast, Colorectal, Lung, and Prostate)Ischemic Heart DiseaseChronic Kidney DiseaseOsteoporosis8 more rows•Dec 1, 2021
Is hyperlipidemia considered a chronic condition?
Hyperlipidemia is usually chronic, requiring ongoing statin medication to control blood lipid levels.
Does chronic care management save money?
The effectiveness of the CCM program saves Medicare approximately $74 per patient, per month. Removing the patient cost burden would positively affect 72%4 of the Medicare population living with chronic conditions, and could save medicare nearly $3,700,000,000 per year in costs.Jul 15, 2019
Is COPD a chronic condition for Medicare?
Who is eligible for a Chronic Condition Special Needs Plan? If you are affected by one of the following conditions, you may be eligible for Medicare coverage even if you are under 65 years of age: Congestive Heart Failure (CHF) Chronic Obstructive Pulmonary Disease (COPD)
How does it affect the average Medicare beneficiary?
Our analysis shows that Medicare beneficiaries spent $5,460 out of their own pockets for health care in 2016, on average, with more than half (58%) spent on medical and long-term care services ($3,166), and the remainder (42%) spent on premiums for Medicare and other types of supplemental insurance ($2,294).Nov 4, 2019
How many Medicare beneficiaries have chronic illness?
In 2018, Medicare beneficiaries with four or more chronic conditions made up 40% of the population but accounted for 78% of total Medicare spending.
What conditions are considered chronic conditions?
Chronic diseases are defined broadly as conditions that last 1 year or more and require ongoing medical attention or limit activities of daily living or both. Chronic diseases such as heart disease, cancer, and diabetes are the leading causes of death and disability in the United States.
Are chronic conditions permanent?
Most chronic illnesses do not fix themselves and are generally not cured completely. Some can be immediately life-threatening, such as heart disease and stroke. Others linger over time and need intensive management, such as diabetes.
What are the top 10 chronic health conditions?
Trends show an overall increase in chronic diseases. Currently, the top ten health problems in America (not all of them chronic) are heart disease, cancer, stroke, respiratory disease, injuries, diabetes, Alzheimer's disease, influenza and pneumonia, kidney disease, and septicemia [14,15,16,17,18].Mar 1, 2018
What is Medicare DUALLY?
Medicare-Medicaid "dually" eligible beneficiaries are randomly assigned to a benchmark plan, which provides prescription drug coverage under the Part D benefit without consideration of their prescription drug profile. To date, the potential for beneficiary assignment to a plan with poor formulary coverage has been minimally studied and the resultant financial impact to beneficiaries unknown.
Did Medicare reduce readmission rates in 2012?
After years of holding steady, hospital readmission rates among fee-for-service Medicare beneficiaries declined significantly in 2012. Hospital readmissions have been shown to be costly and are a common metric for assessing care quality, so the Medicare program, hospitals, and other stakeholders have made reducing re-hospitalizations a high priority.