2020 Medicare Part A deductible and coinsurance fees
| 2020 Medicare Part A deductible and coin ... | |
| Inpatient hospital deductible (first 60 ... | $1,408 |
| Daily coinsurance (days 61–90) | $352 |
| Daily coinsurance for lifetime reserve d ... | $704 |
| 2020 Medicare Part A deductible and coinsurance fees | |
|---|---|
| Inpatient hospital deductible (first 60 days of inpatient stay and services) | $1,408 |
| Daily coinsurance (days 61–90) | $352 |
| Daily coinsurance for lifetime reserve days (60 additional days) | $704 |
How long will Medicare pay for a hospital stay?
Once the deductible is paid fully, Medicare will cover the remainder of hospital care costs for up to 60 days after being admitted. If you need to stay longer than 60 days within the same benefit period, you’ll be required to pay a daily coinsurance.
How does Medicare reimburse hospitals?
- asthma
- atrial fibrillation
- cellulitis
- congestive heart failure
- chronic kidney disease
- chronic obstructive pulmonary disease
- diabetes
- gout
- hypertension
- infections
What percent does Medicare cover?
Original Medicare Part A, which covers hospitalization, has a deductible of $1184. Original Medicare Part B, which covers out-of-hospital services, generally covers 80%. You can get these gaps in coverage filled by purchasing a medicare supplement (PPO) or a Medicare Advantage Plan (HMO).
Does Medicare cover hospital visits?
Under Medicare you can be treated as a public patient in a public hospital, at no charge. Medicare will also cover some or all the costs of seeing a GP or specialist outside of hospital, and some pharmaceuticals.

How Does Medicare pay a hospital?
Under the outpatient prospective payment system, hospitals are paid a set amount of money (called the payment rate) to give certain outpatient services to people with Medicare. For most services, you must pay the yearly Part B deductible before Medicare pays its share.
What percentage of hospital costs does Medicare cover?
Everyone with Medicare is entitled to a yearly wellness visit that has no charge and is not subject to a deductible. Beyond that, Medicare Part B covers 80% of the Medicare-approved cost of medically necessary doctor visits. The individual must pay 20% to the doctor or service provider as coinsurance.
Does Medicare pay 100 percent of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
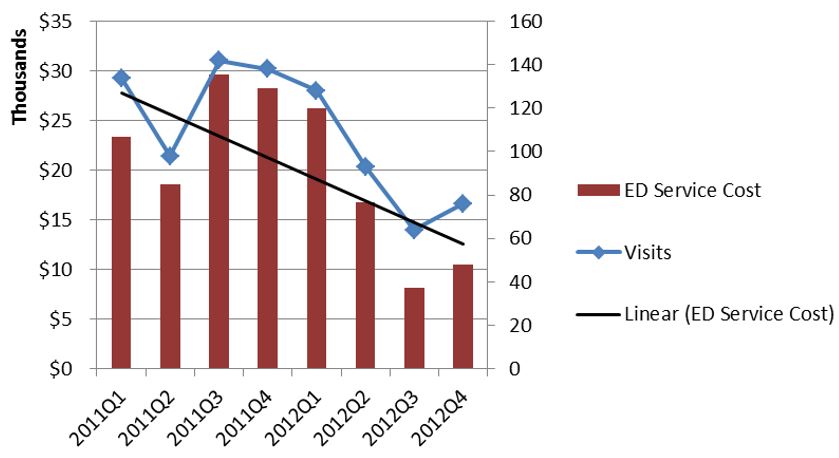
What percent of hospital revenue is from Medicare?
The percentage of the total payor mix from private/self-pay increased from 66.5% in 2018 to 67.4% in 2020. The Medicare percentage decreased from 21.8% to 20.5%.
Does Medicare pay for everything?
Original Medicare (Parts A & B) covers many medical and hospital services. But it doesn't cover everything.
What is the Medicare deductible for a hospital stay?
$1,556Part A Deductible: The deductible is an amount paid before Medicare begins to pay its share. The Part A deductible for an inpatient hospital stay is $1,556 in 2022. The Part A deductible is not an annual deductible; it applies for each benefit period.
Does Medicare only pay 80%?
You will pay the Medicare Part B premium and share part of costs with Medicare for covered Part B health care services. Medicare Part B pays 80% of the cost for most outpatient care and services, and you pay 20%. For 2022, the standard monthly Part B premium is $170.10.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
How much is a hospital stay per day?
Total health care spending in America went over $4 trillion in 2020 and more than 30% of that – or about $1.24 trillion – was spent on hospital services. Hospital costs averaged $2,607 per day throughout the U.S., with California ($3,726 per day) just edging out Oregon ($3,271) for most expensive.
How much profit does a hospital make?
The average profit margin for hospitals in the U.S. has been around 8% since 2012 even though more than 80% of hospitals admissions in the U.S. are to non-profit hospitals.
Which is the largest component of hospital costs?
The answer is labor costs, according to the new American Hospital Association (AHA) report, "The Cost of Caring." Labor cost increases are responsible for 35 percent of the overall growth in hospital costs.
Where does hospital revenue come from?
The majority of revenues for the provision of medical services comes from various government programs (Sullivan, 2015). The money that a hospital receives for the services it provides is called operating revenue. Other sources of hospital funding are research grants and donations.
What are Medicare covered services?
Medicare-covered hospital services include: Semi-private rooms. Meals. General nursing. Drugs as part of your inpatient treatment (including methadone to treat an opioid use disorder) Other hospital services and supplies as part of your inpatient treatment.
What does Medicare Part B cover?
If you also have Part B, it generally covers 80% of the Medicare-approved amount for doctor’s services you get while you’re in a hospital. This doesn't include: Private-duty nursing. Private room (unless Medically necessary ) Television and phone in your room (if there's a separate charge for these items)
What is an inpatient hospital?
Inpatient hospital care. You’re admitted to the hospital as an inpatient after an official doctor’s order, which says you need inpatient hospital care to treat your illness or injury. The hospital accepts Medicare.
How many days in a lifetime is mental health care?
Things to know. Inpatient mental health care in a psychiatric hospital is limited to 190 days in a lifetime.
What is Medicare insurance?
Medicare insurance is one of the most popular options for those who qualify, and the number of people using this insurance continues to grow as life expectancy continues to increase. Medicare policies come available with many different parts, including Part A, Part B, Part C, and Part D.
When a patient uses Medicare as their primary insurance company, is the hospital required to choose appropriate and accurate diagnoses that
When a patient uses Medicare as their primary insurance company, the hospital is required to choose appropriate and accurate diagnoses that apply to the patient so that they can bill for the associated care.
How long do you have to pay coinsurance for hospital?
As far as out-of-pocket costs, you will be responsible for paying your deductible, coinsurance payments if your hospital stay is beyond 60 days, and for any care that is not deemed medically necessary. However, the remainder of the costs will be covered by your Medicare plan.
Does Medicare pay flat rate?
This type of payment system is approved by the hospitals and allows Medicare to pay a simple flat rate depending on the specific medical issues a patient presents with and the care they require. In addition, In some cases, Medicare may provide increased or decreased payment to some hospitals based on a few factors.
Does Medicare cover inpatient care?
If you receive care as an inpatient in a hospital, Medicare Part A will help to provide coverage for care. Part A Medicare coverage is responsible for all inpatient care , which may include surgeries and their recovery, hospital stays due to illness or injury, certain tests and procedures, and more. As far as out-of-pocket costs, you will be ...
Medicare Advantage Plan (Part C)
Monthly premiums vary based on which plan you join. The amount can change each year.
Medicare Supplement Insurance (Medigap)
Monthly premiums vary based on which policy you buy, where you live, and other factors. The amount can change each year.
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
What happens if you don't buy Medicare?
If you don't buy it when you're first eligible, your monthly premium may go up 10%. (You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.) Part A costs if you have Original Medicare. Note.
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
How much is coinsurance for days 91 and beyond?
Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime). Beyond Lifetime reserve days : All costs. Note. You pay for private-duty nursing, a television, or a phone in your room.
How much is coinsurance for 61-90?
Days 61-90: $371 coinsurance per day of each benefit period. Days 91 and beyond: $742 coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime) Beyond lifetime reserve days: all costs. Part B premium.
Do you pay more for outpatient services in a hospital?
For services that can also be provided in a doctor’s office, you may pay more for outpatient services you get in a hospital than you’ll pay for the same care in a doctor’s office . However, the hospital outpatient Copayment for the service is capped at the inpatient deductible amount.
Does Medicare cover room and board?
Medicare doesn't cover room and board when you get hospice care in your home or another facility where you live (like a nursing home). $1,484 Deductible for each Benefit period . Days 1–60: $0 Coinsurance for each benefit period. Days 61–90: $371 coinsurance per day of each benefit period.
How many DRGs can be assigned to a patient?
Each DRG is based on a specific primary or secondary diagnosis, and these groups are assigned to a patient during their stay depending on the reason for their visit. Up to 25 procedures can impact the specific DRG that is assigned to a patient, and multiple DRGs can be assigned to a patient during a single stay.
What is Medicare reimbursement based on?
Reimbursement is based on the DRGs and procedures that were assigned and performed during the patient’s hospital stay. Each DRG is assigned a cost based on the average cost based on previous visits. This assigned cost provides a simple method for Medicare to reimburse hospitals as it is only a simple flat rate based on the services provided.
What is Medicare Part A?
What Medicare Benefits Cover Hospital Expenses? Medicare Part A is responsible for covering hospital expenses when a Medicare recipient is formally admitted. Part A may include coverage for inpatient surgeries, recovery from surgery, multi-day hospital stays due to illness or injury, or other inpatient procedures.
How much higher is Medicare approved?
The amount for each procedure or test that is not contracted with Medicare can be up to 15 percent higher than the Medicare approved amount. In addition, Medicare will only reimburse patients for 95 percent of the Medicare approved amount.
How much extra do you have to pay for Medicare?
This means that the patient may be required to pay up to 20 percent extra in addition to their standard deductible, copayments, coinsurance payments, and premium payments. While rare, some hospitals completely opt out of Medicare services.
Is Medicare reimbursement lower than private insurance?
This is mainly due to the fact that Medicare reimbursement amounts are often lower than those received from private insurance companies . For these providers, the patient may be required to pay for the full cost of the visit up front and can then seek personal reimbursement from Medicare afterwards.
Does Medicare cover permanent disability?
Medicare provides coverage for millions of Americans over the age of 65 or individuals under 65 who have certain permanent disabilities. Medicare recipients can receive care at a variety of facilities, and hospitals are commonly used for emergency care, inpatient procedures, and longer hospital stays. Medicare benefits often cover care ...
What is Medicare Supplement Insurance?
Some Medicare Supplement Insurance plans (also called Medigap) provide coverage for the Medicare Part B excess charges that may result when a health care provider does not accept Medicare assignment.
What is Medicare Part B excess charge?
What are Medicare Part B excess charges? You are responsible for paying any remaining difference between the Medicare-approved amount and the amount that your provider charges. This difference in cost is called a Medicare Part B excess charge. By law, a provider who does not accept Medicare assignment can only charge you up to 15 percent over ...
What does it mean when a doctor accepts Medicare assignment?
If a doctor or supplier accepts Medicare assignment, this means that they agree to accept the Medicare-approved amount for a service or item as payment in full. The Medicare-approved amount could potentially be less than the actual amount a doctor or supplier charges, depending on whether or not they accept Medicare assignment.
What is Medicare approved amount?
The Medicare-approved amount is the total payment that Medicare has agreed to pay a health care provider for a service or item. Learn more your potential Medicare costs. The Medicare-approved amount is the amount of money that Medicare will pay a health care provider for a medical service or item.
How much does Medicare pay for a doctor appointment?
Typically, you will pay 20 percent of the Medicare-approved amount, and Medicare will pay the remaining 80 percent .
How much can a provider charge for not accepting Medicare?
By law, a provider who does not accept Medicare assignment can only charge you up to 15 percent over the Medicare-approved amount. Let’s consider an example: You’ve been feeling some pain in your shoulder, so you make an appointment with your primary care doctor.
Does a specialist accept Medicare?
The specialist you visit agrees to treat Medicare patients but does not agree to accept the Medicare-approved amount as full payment. You still only pay 20 percent of the Medicare-approved amount for your primary care doctor appointment. But because your specialist does not agree to the Medicare-approved amount as full payment for their services, ...
How much does Medicare pay for a doctor's visit?
For example, you might pay $10 or $20 for a doctor's visit or prescription drug. for each emergency department visit and a copayment for each hospital service. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid.
Why don't you pay copays for emergency department visits?
If your doctor admits you to the same hospital for a related condition within 3 days of your emergency department visit, you don't pay the copayment because your visit is considered part of your inpatient stay.
What does Medicare Part B cover?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. usually covers emergency department services when you have an injury, a sudden illness, or an illness that quickly gets much worse.