The act of moving a person with limited function from one location to another. This may be accomplished by the patient or with assistive devices. Medical Dictionary, © 2009 Farlex and Partners Patient discussion about transferring Q. can hepatitis be transferred from fathers sperm when concieving a child?
What does it mean when a transfer occurs between two hospitals?
The transfer occurs between two different hospitals. The transfer is between different facilities that are commonly owned but do not have “merged records” (more on that below).
How does Medicare work with other insurance?
How Medicare works with other insurance. If you have Medicare and other health insurance or coverage, each type of coverage is called a "payer.". When there's more than one payer, " Coordination of benefits " rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to...
What happens to my Medicare if I move to another state?
In addition to alerting Medicare of your new address, you may also need to notify your carrier if you have a Medicare Supplement plan, a Medicare Advantage plan, and a Medicare Part D prescription drug plan. In some cases, you might not be able to keep your plan when you move. How Do I tell Medicare I’m Moving to Another State?
What is an “acute care transfer”?
An “acute care transfer” occurs when a Medicare beneficiary in an IPPS hospital (with any MS-DRG) is: Transferred to another acute care IPPS hospital or unit for related care - Patient Discharge Status Code 02 (or 82 when an Acute Care Hospital Inpatient Readmission is planned); or

What is Medicare transfer?
An acute care transfer occurs when a Medicare patient in an IPPS hospital (with any MS- DRG) is: 1. Transferred to another acute care IPPS hospital or unit for related care (Patient. Discharge Status Code 02 or Planned Acute Care Hospital Inpatient Readmission.
What does it mean when a patient is transferred?
Transfers are defined as moving a patient from one flat surface to another, such as from a bed to a stretcher (Perry et al., 2014). Types of hospital transfers include bed to stretcher, bed to wheelchair, wheelchair to chair, and wheelchair to toilet, and vice versa.
Why would a patient be transferred?
Patients could undergo transfer to receive higher quality care in the form of clinical expertise and vigilance, to receive a specific test or procedure, for family convenience, or because either they or their families are unsatisfied with the care received at the referring hospital.
What does transfer care mean?
Transfer of care occurs when a physician or other qualified professional providing management for some or all of a patient's problems has not provided consultative services from the initial encounter, and relinquishes responsibility.
What should you assess before transferring a patient?
When preparing to safely transfer a patient from a bed to a wheelchair, the nurse should first:Determine the patient's arm strength.Assess the patient's weight-bearing ability.Assess the patient's willingness to cooperate.Decide upon the most appropriate transfer method.
What is important before transferring a patient to another facility?
A written and informed consent of patient's relatives along with the reason to transfer is mandatory before the transfer. In some countries, dedicated critical care transfer groups have been established to coordinate and facilitate the patient transfer.
What is the process of transferring a patient from one hospital to another?
The receiving hospital must have adequate space and staff to attend to the patient. The receiving hospital must have agreed to accept the transfer. The transfer is done with qualified medical staff and transportation equipment, including the use of necessary and appropriate life support measures.
Can a patient on life support be transferred?
Yes. Hospitals can transfer or discharge you if you request a transfer or discharge against medical advice and provide informed consent to receive such a transfer or discharge.
When should a patient be transferred to ICU?
Intensive care is needed if someone is seriously ill and requires intensive treatment and close monitoring, or if they're having surgery and intensive care can help them recover. Most people in an ICU have problems with 1 or more organs. For example, they may be unable to breathe on their own.
Why is transfer of care important?
The transfer of care process plays an important role in enhancing patient outcomes, reducing readmissions, improving hospital efficiency and improving patient flow through health services.
How do you transfer a patient from one bed to another?
1:173:36B 404 Transferring from bed to stretcher - YouTubeYouTubeStart of suggested clipEnd of suggested clipSupport the patient's head while you remove the pillow. Next. Lower the side rails on the bed. ThenMoreSupport the patient's head while you remove the pillow. Next. Lower the side rails on the bed. Then cross the patient's arms over her chest.
How do I transfer my residency from a wheelchair to a bed?
2:193:30Instructional Video for Transfer a Patient from Bed to WheelchairYouTubeStart of suggested clipEnd of suggested clipWhile you grasp the gate belt around the patient's back bend your knees and lift with your legsMoreWhile you grasp the gate belt around the patient's back bend your knees and lift with your legs lifting. The patient up and over to the wheelchair seating. Them into the wheelchair in one motion.
transferring
The act of moving a person with limited function from one location to another. This may be accomplished by the patient or with assistive devices.
Patient discussion about transferring
Q. can hepatitis be transferred from fathers sperm when concieving a child? My partner has hepatitis C and he has gotten me pregnant will our baby have it too?
What would happen if Medicare transfer criteria were not met?
If Medicare’s transfer criteria were not met and both services occurred on the same day, you would bill a combined subsequent visit code for both services. The answer would be the same if the patient was transferred from hospital “B.”.
What does "no merged records" mean?
Instead, “no merged records” means that the acute care record is considered closed and a new record has been initiated for that patient in the new unit, facility or hospital to which he or she has been transferred.And a quick reminder: PPS refers to a Medicare reimbursement method based on a predetermined, fixed amount.
Can a physician bill both a hospital discharge code and an initial hospital care code?
Under certain circumstances, physicians transferring patients may bill both a hospital discharge code and an initial hospital care code. To do so, the first requirement is that two physicians in the same group (or even the same physician) must have performed the discharge and the elements of an initial hospital care code.
Can you bill a subsequent visit and an initial hospital code on the same day?
Because the subsequent visit codes are “per day” codes, you cannot bill a subsequent visit code and an initial hospital care code on the same day. The exception for billing two codes on the same day is if the patient is transferred to a nursing home; in that case, if a physician in your group performed the discharge, ...
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What happens when there is more than one payer?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) to pay. In some rare cases, there may also be a third payer.
What is a health care provider?
Tell your doctor and other. health care provider. A person or organization that's licensed to give health care. Doctors, nurses, and hospitals are examples of health care providers. about any changes in your insurance or coverage when you get care.
What do the letters on my Medicare card mean?
What do the letters on your Medicare card mean? The Medicare number displayed on Medicare cards (known as an MBI, or Medicare Beneficiary Identifier) is 11 characters long: The 2nd, 5th, 8th and 9th characters are always a letter, and the 3rd and 6th characters are sometimes a letter. All other characters will be numbers, and the letters S, L, O, ...
What is Medicare Part B?
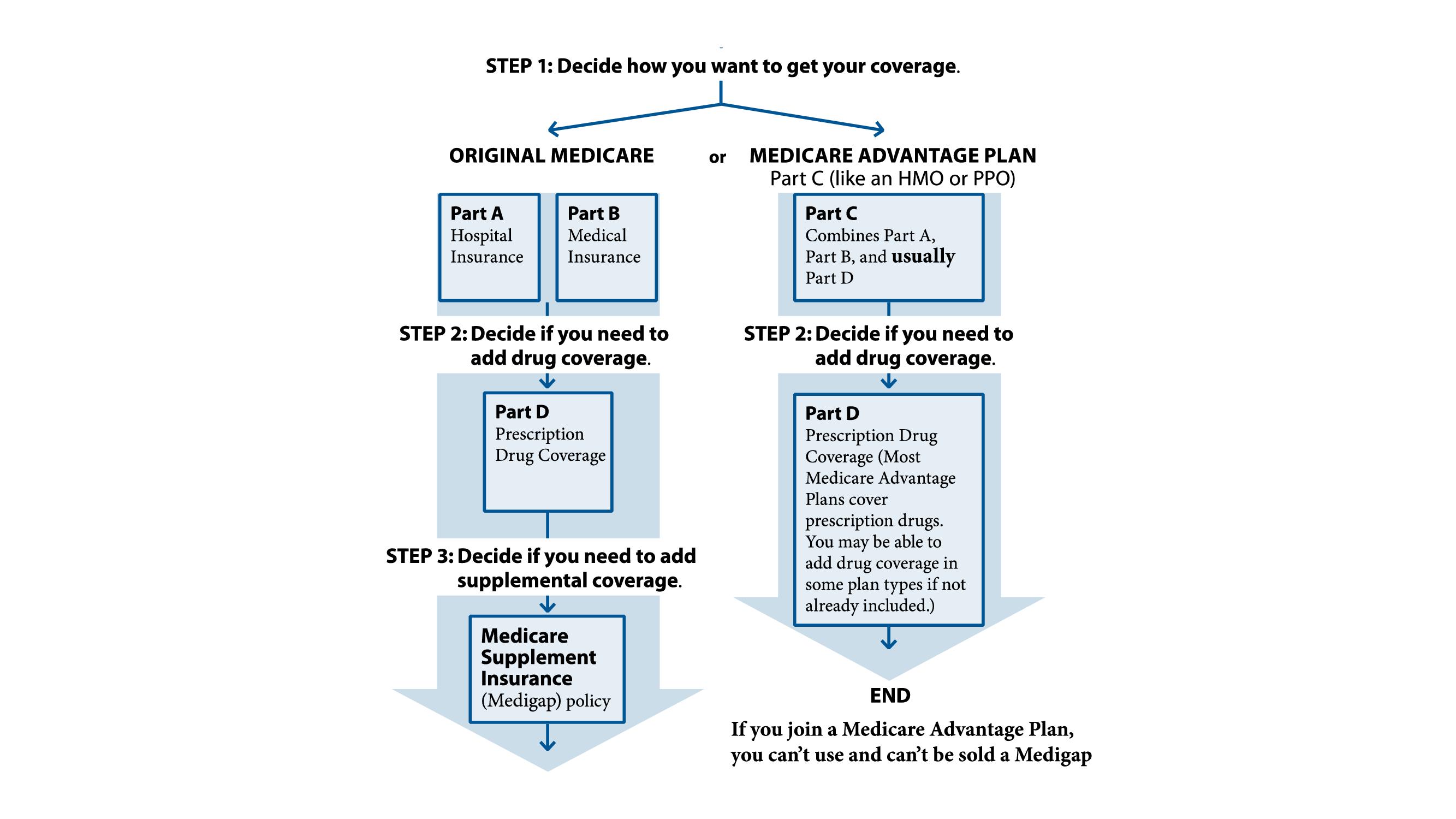
Medicare Part B is medical insurance and provides coverage for outpatient doctor’s appointments and medical devices. Medicare Part C, also known as Medicare Advantage, provides coverage for everything found in Part A and Part B through one plan provided by a private insurer.
What is Medicare Supplement Insurance?
Medicare Supplement Insurance, also called Medigap, uses a letter system to identify its plans. Medicare Supplement Insurance is used in conjunction with Part A and Part B of Medicare to provide coverage for certain out-of-pocket expenses like some Medicare deductibles and coinsurance.
Does Medicare cover dental insurance?
Many Medicare Advantage plans may also cover additional benefits not covered by Part A and Part B, such as prescription drugs, dental, vision, hearing, wellness programs like SilverSneakers and more. Medicare Part D provides coverage exclusively for prescription drugs.
What to do if you move to a new state with Medicare?
If you are moving, no matter what type of Medicare coverage you have, you must inform the Social Security Administration of your new address. If you cannot keep your current healthcare providers, perhaps they can recommend people in your new state.
What is a SEP in Medicare?
You can take advantage of a Special Enrollment Period (SEP) to make changes to a Part C or D plan. SEPs are available for Medicare recipients who experience certain life events. If you are moving outside your plan’s area of service and need a new plan, or if you are moving within the plan’s area of service and wish to include new plan options ...
How to enroll in Medicare Supplement Plan?
1. Enroll in a Medicare Supplement Plan through your current Medigap provider if it covers the same, or fewer benefits than your current SELECT plan. 2. Enroll in a Medigap plan offered by any provider in your new area of service. Also, if you have a Medicare Advantage plan in your current state but there are no available Part C plans in the state ...
How to change my Social Security mailing address?
When you move, you should also contact the Social Security Administration to change your on-file mailing address. You can do this online at the official S.S.A. site which is www.ssa.gov, or you can phone them at 1-800-772-1213 Monday through Friday from 7:00 a.m. to 7:00 p.m.
Does Medicare require you to use a hospital?
Medicare does not require you to use healthcare providers or hospitals in networks, as is the case with some Medicare Advantage plans. Once you have moved, you can choose any physician, hospital, or other healthcare provider as long as they accept Medicare assignment. Using healthcare providers who accept Medicare assignment ensures ...
Do you need to change your Medicare plan when you move?
Generally speaking, if your plan requires that you use a set network for healthcare service providers, you will need to make more changes when you move . Because having continuous healthcare coverage is so important, you should have all the facts about how your Medicare benefits are affected by your move before you start packing.
Does moving affect Medicare?
Does moving affect your Medicare Advantage or Medicare Prescription Drug Plan? If you have a Medicare Advantage (Part C) or Prescription Drug (Part D) Plan, your coverage is likely restricted to a specific service area. If you are moving outside your current plan’s area, you must enroll in a new plan which includes the area where your new home is.
Key takeaways
What costs should you expect if you’re moving from expanded Medicaid to Medicare?
Millions under expanded Medicaid will transition to Medicare
There are currently almost 20 million people covered under expanded Medicaid, accounting for almost a quarter of all Medicaid enrollees nationwide. Under ACA rules, there are no asset limitations for Medicaid eligibility for pregnant women, children, or adults eligible due to Medicaid expansion.
Moving from expanded Medicaid to Medicare Advantage
Depending on your circumstances, you might choose to enroll in a Medicare Advantage plan that provides prescription, dental, and vision coverage – and caps enrollees’ annual out-of-pocket costs for Parts A and B, which traditional Medicare does not do.
Transitioning from expanded Medicaid to Medigap
The more expensive way to cover the gaps in traditional Medicare is to buy a Medigap policy, which generally costs anywhere from a minimum of $25/month to more than $200/month to cover out-of-pocket costs for Parts A and B. That’s on top of premiums for Medicare Parts B and D (prescription drugs).
Medicare can pull you out of the coverage gap
Although the transition from expanded Medicaid to Medicare can be financially challenging, eligibility for Medicare will likely come as a welcome relief if you’ve been in the coverage gap in one of the 11 states that have refused to expand Medicaid.
What steps do I need to take to move from expanded Medicaid to Medicare?
If you’re enrolled in expanded Medicaid and you’ll soon be 65, you’ll want to familiarize yourself with the health coverage and assistance programs that might be available to you.
Legislation aims to make Medicare more affordable for lower-income Americans
The Improving Medicare Coverage Act, introduced in the U.S. House in September by Washington Representative Pramila Jayapal, would do away with cost-sharing and premiums for Medicare beneficiaries with income up to 200% of the poverty level (it would also lower the Medicare eligibility age to 60).
What percentage of your income is taxable for Medicare?
The current tax rate for Medicare, which is subject to change, is 1.45 percent of your gross taxable income.
Is Medicare payroll tax deductible?
If you are retired and still working part-time, the Medicare payroll tax will still be deducted from your gross pay. Unlike the Social Security tax which currently stops being a deduction after a person earns $137,000, there is no income limit for the Medicare payroll tax.
What happens if you drop Medicare?
If you drop Medicare and don’t have creditable employer coverage, you’ll face penalties when getting Medicare back. Before you decide to drop any part of Medicare, there are some things you’ll want to think about, especially as some choices could end up being costly.
How long do you have to enroll in Medicare after you lose your employer?
NOTE: While you have eight months for Parts A & B, you only get two months after losing the employer coverage or leaving work to re-enroll in a Medicare Part D prescription drug plan or a Medicare Advantage (Part C) plan. If you enroll later, you’ll face late enrollment penalties for Part D.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
How long do you have to wait to enroll in Medicare after dropping it?
There are rules for re-enrolling in Medicare after you’ve dropped it for an employer-sponsored health plan. You’ll have an 8-month Special Enrollment Period in which to re-enroll in Medicare Part A and Part B. If you miss this window, you’ll have to wait to enroll in the Medicare General Enrollment Period (January 1 – March 31) ...