Generally, if you are retired and receiving retiree coverage through a former employer, Medicare pays first and group coverage pays second. However, if you are retired, your spouse is not retired and you are covered under his or her policy with 20 or more employees, group coverage pays first and Medicare pays second. Additional Things to Consider
Who pays first – Medicare or group health?
Aug 23, 2018 · When there’s more than one payer, “coordination of benefits” rules decide who pays first. The “primary payer” pays what it owes on your bills first, and then your provider sends the rest to the “secondary payer” to pay. In some cases, there may also be a “third payer.” Whether Medicare pays first depends on a number of things. Be sure to tell your doctor and other health …
Who will pay the full premium for Medicare Part A?
Nov 10, 2016 · The Medicare Part A inpatient hospital deductible that beneficiaries pay when admitted to the hospital will be $1,316 per benefit period in 2017, an increase of $28 from $1,288 in 2016. The Part A deductible covers beneficiaries’ share of costs for the first 60 days of Medicare-covered inpatient hospital care in a benefit period.
How do I find out who pays first Medicare or Medicaid?
If you're enrolled in Part B but are not receiving Social Security payments, or the premiums are not deducted from them, you'll pay $134 a month in 2017. If you enroll in Part B for the first time in 2017 — regardless of whether you're receiving Social Security payments — you will pay $134 a month. If your Part B premiums are paid by your state because of low income, you will continue …
How much will Medicare Part B cost you in 2017?
decide who pays first. The “primary payer” pays what it owes on your bills first, and then you or your health care provider sends the rest to the “secondary payer” to pay. In some rare cases, there may also be a “third payer.” Whether Medicare pays first depends on a …

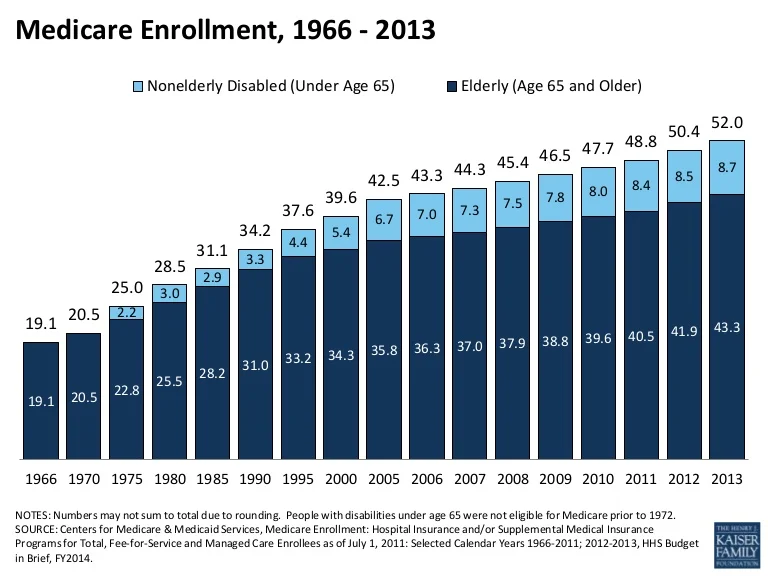
Who enrolls most in Medicare?
Is Medicare always the primary payer?
Who funds Original Medicare?
When did Medicare start charging?
Does Medicare pay first or second?
Does Medicare automatically forward claims to secondary insurance?
Is Medicare funded by taxpayers?
Where does funding for Medicare come from?
How does Medicare get paid for?
When did federal employees start paying Medicare?
Which US president became the first beneficiary of Medicare?
When did Medicare start and why?
What is the Medicare premium for 2017?
For the remaining roughly 30 percent of beneficiaries, the standard monthly premium for Medicare Part B will be $134.00 for 2017, a 10 percent increase from the 2016 premium of $121.80. Because of the “hold harmless” provision covering the other 70 percent of beneficiaries, premiums for the remaining 30 percent must cover most ...
What is Medicare Part A?
Medicare Part A Premiums/Deductibles. Medicare Part A covers inpatient hospital, skilled nursing facility, and some home health care services. About 99 percent of Medicare beneficiaries do not have a Part A premium since they have at least 40 quarters of Medicare-covered employment. The Medicare Part A inpatient hospital deductible ...
How much is Medicare Part A deductible?
The Medicare Part A inpatient hospital deductible that beneficiaries pay when admitted to the hospital will be $1,316 per benefit period in 2017, an increase of $28 from $1,288 in 2016. The Part A deductible covers beneficiaries’ share of costs for the first 60 days of Medicare-covered inpatient hospital care in a benefit period.
What is the COLA for Social Security?
Because of the low Social Security COLA, a statutory “hold harmless” provision designed to protect seniors, will largely prevent Part B premiums from increasing for about 70 percent ...
Why does Bill have Medicare?
Bill has Medicare coverage because of permanent kidney failure.He also has group health plan coverage through his company.Bill’s group health plan coverage will be the primary payer forthe first 30 months after he becomes eligible for Medicare. After30 months, Medicare becomes the primary payer.
What is the original Medicare plan?
The Original Medicare Plan—This a fee-for-service plan . Thismeans you are usually charged a fee for each health care service orsupply you get. This plan, managed by the Federal Government, isavailable nationwide. You will stay in the Original Medicare Planunless you choose to join a Medicare Advantage Plan.
Which Medicare plans cover more services?
Medicare Advantage Plans and Other Medicare HealthPlans—These plans, which include HMOs, PPOs, and PFFS plans,may cover more services and have lower out-of-pocket costs than theOriginal Medicare Plan. However, in some plans, like HMOs, youmay only be able to see certain doctors or go to certain hospitals.
What does Medicare Part B cover?
Medicare Part B—Medical Insurance, helps pay fordoctors’services and outpatient care. It also covers some other medicalservices that Medicare Part A doesn’t cover, such as some of theservices of physical and occupational therapists, and some homehealth care. Medicare Part Bhelps pay for these covered services andsupplies when they are medically necessary.
How old is Marge from ABC?
Marge is 72 years old and works full time for the ABC Company with75 employees. She has group health plan coverage through heremployer. Therefore, her group health plan will be the primary payerand Medicare will be the secondary payer.
Does Mary work for XYZ?
Mary works full-time for XYZ Company, which has 120employees. She has large group health plan coverage for herselfand her husband. Her husband has Medicare because of adisability. Therefore, Mary’s group health plan coverage paysfirst for Mary’s husband, and Medicare is his secondary payer.
Is Medicare the primary payer?
If you retire but still have group insurance through your former employer or your spouse’s employer, Medicare is the primary payer. This assumes you have both Part A and B (Original Medicare) and that your provider accepts assignment. Once it pays its share, Medicare sends the remaining bill to your secondary payer.
Is Medicare the primary payer for end stage renal disease?
Have End-Stage Renal Disease. If you have End-Stage Renal Disease (ESRD) and a group health plan, primary payer is determined by how long you’ve been eligible or entitled to Medicare. During the first 30 months of your eligibility or entitlement, Medicare is the secondary payer. After 30 months, Medicare becomes the primary payer.
What is the primary payer?
Primary payer: This is the payer who pays its portion of covered services first.
What is the difference between primary and secondary payer?
Secondary payer: After the primary payer pays, the bill is sent to the secondary payer so it can pay its share.
How to use VA benefits?
To use your VA benefits, simply receive care from a VA facility. If you prefer to see a civilian doctor, use Medicare. If you favor civilian healthcare over VA, you may wish to purchase a Medigap policy. This won’t cover services received via the VA. When you see a civilian provider, Medigap becomes the secondary payer.
What are the benefits of Medicare?
Medicare provides health care for more than 59.8 million Americans, but that does not mean it necessarily covers everything they need. Consider these common items that Medicare leaves you to pay for out of pocket: 1 Acupuncture 2 Care during foreign travel with rare exceptions 3 Chiropractor services except to correct subluxation of the spine 4 Corrective eye lenses (contact lenses or eyeglasses) 5 Custodial care (bathing, dressing, toileting) 6 Dentures 7 Foot care 8 Hearing aids 9 Long-term nursing home care 10 Non-emergency transportation with rare exceptions 11 Over-the-counter medications, vitamins, and supplements 12 Prescription medications in certain categories 13 Walking canes for the blind
What happens if you don't pay Medicare?
If you do not meet the criteria for Medicare to pay first, your employer-sponsored health plan will be billed instead. What they do not pay for will then be billed to Medicare. Medicare will pay for healthcare services that it would normally cover as long as it sees them as medically necessary. Medicare will pay first.
How long can you keep your health insurance after you leave your job?
Thanks to the Consolidated Omnibus Budget Reconciliation Act (COBRA) of 1985 you can continue your employer-sponsored health plan after you leave your job. The law requires employers of 20 or more full-time employees to offer continued access to their health plan for a period of time, usually 18 months, after your job ends by way of termination or a layoff. The duration of COBRA coverage may be extended up to 36 months if certain conditions are met.
When did Social Security retirement age change?
The retirement age for Social Security benefits used to be 65 years old, the same age that you become eligible for Medicare. That all changed in 1983 when Congress passed legislation to increase the retirement age based on your birthday. For people born between 1943 and 1954, the retirement age is now 66 years old.
What is the retirement age for Social Security?
The retirement age for Social Security benefits used to be 65 years old, the same age that you become eligible for Medicare. That all changed in 1983 when Congress passed legislation to increase the retirement age based on your birthday. For people born between 1943 and 1954, the retirement age is now 66 years old. The retirement age gradually increases to a maximum of 67 years of age for those born after 1960. Retiring earlier than this designated age will result in your getting lesser payments from Social Security.
When did the retirement age change?
That all changed in 1983 when Congress passed legislation to increase the retirement age based on your birthday. For people born between 1943 and 1954, the retirement age is now 66 years old. The retirement age gradually increases to a maximum of 67 years of age for those born after 1960.
What is the retirement age for people born in 1943?
For people born between 1943 and 1954, the retirement age is now 66 years old. The retirement age gradually increases to a maximum of 67 years of age for those born after 1960. Retiring earlier than this designated age will result in your getting lesser payments from Social Security.