Common mistakes include:
- Joining a Medicare Advantage or Part D plan based on premium alone
- Relying on the advice of a friend or family member
- Not knowing how to access all available plans
- Waiting until the last minute, not leaving yourself time to research your options
- Purchasing a plan or policy at the top of your budget
Full Answer
What should I look for when choosing a health provider for Medicare?
Assuming Your Medicare Coverage Will Stay the Same It’s quite common for Medicare plans to change from year-to-year, so... Forgetting to Compare Medicare Plans & Shop Around Even if you’re satisfied with your current Medicare plan, there …
What happens if you sign up for Medicare late?
Medicare Mistake #10: Costly Financial Moves when You Retire In Medicare Mistake #9 we talked about how expensive it can be to go out-of-network in a Medicare Advantage plan and what you can do about it. Similarly, retiring can also be costly with Medicare. In this tenth and final edition of our Medicare … [Read More...]
What happens if I delay enrolling in Medicare Part B?
Common mistakes include: Joining a Medicare Advantage or Part D plan based on premium alone Relying on the advice of a friend or family member Not knowing how to access all available plans Waiting until the last minute, not leaving yourself time to research your options Purchasing a plan or policy ...
How can I pay for Medicare out-of-pocket costs?
Nov 25, 2012 · Mistake No. 1: Not bothering to give your current coverage a checkup The first step is to take stock of what you have. Even if you like your drug coverage, make sure you review your plan’s annual notice of change, a letter from the companies that Part D enrollees should have received by now, Riccardi says.
How do I decide what Medicare plan is best for me?
To compare Medicare plans, use the Medicare Plan Finder at www.medicare.gov/find-a-plan, on the official U.S. government site for people with Medicare, which allows you to compare plans by cost, by quality and by other features that may be of importance to you.
Does Medicare make mistakes?
It's easy to make mistakes when it comes to Medicare. And the biggest one to avoid is to not take charge of evaluating your Medicare coverage every year. Medicare Annual Enrollment (Oct. 15 – Dec.
What they don't tell you about Medicare?
'Medicare Part A covers hospital stays' What they don't tell you: There's either a deductible or daily copay. And if the hospital hoodwinks you into being “under observation,” rather than formally admitting you, your costs are going to be even higher. If you're in Original Medicare, Part A covers hospital stays.Oct 31, 2021
What happens if you don't choose a Medicare plan?
If you don't switch to another plan, your current coverage will continue into next year — without any need to inform Medicare or your plan. However, your current plan may have different costs and benefits next year.
Is Medicare confusing?
Despite evidence of a widespread lack of knowledge about Medicare – and a high percentage of beneficiaries admitting that Medicare is confusing and difficult to understand – many of the same beneficiaries reported a high amount of confidence in their knowledge of Medicare terms, their understanding of Medicare coverage ...
Can I avoid Medicare?
If you do not want to use Medicare, you can opt out, but you may lose other benefits. People who decline Medicare coverage initially may have to pay a penalty if they decide to enroll in Medicare later.
Does Medicare look at your bank account?
Medicare plans and people who represent them can't do any of these things: Ask for your Social Security Number, bank account number, or credit card information unless it's needed to verify membership, determine enrollment eligibility, or process an enrollment request.
Does Medicare care how much money you have in the bank?
You may have up to $2,000 in assets as an individual or $3,000 in assets as a couple.
Is Medicare determined by income?
Medicare premiums are based on your modified adjusted gross income, or MAGI. That's your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS.
What is the biggest disadvantage of Medicare Advantage?
The primary advantage is the monthly premium, which is generally lower than Medigap plans. The top disadvantages are that you must use provider networks and the copays can nickel and dime you to death.Dec 12, 2021
What are 4 types of Medicare Advantage plans?
Medicare Advantage PlansHealth Maintenance Organization (HMO) Plans.Preferred Provider Organization (PPO) Plans.Private Fee-for-Service (PFFS) Plans.Special Needs Plans (SNPs)
Are you automatically enrolled in Medicare if you are on Social Security?
Yes. If you are receiving benefits, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. (Medicare is operated by the federal Centers for Medicare & Medicaid Services, but Social Security handles enrollment.)
What is mistake 5?
Mistake #5 – Using the Wrong Criteria to Make a Purchase Decision. Sure, your friends will tell you how great their Medicare plan is. But your prescriptions are not the ones they take, and their doctors are not yours. So, their plan will not typically be the best one for you.
When can I switch to Medicare Advantage?
You can also switch to a different plan or switch to original Medicare during the Medicare Advantage Open Enrollment Period (January 1 through March 31), though only one plan change is allowed during this window.
What is the difference between Medicare Advantage and Medicare Part D?
By far the biggest difference among Medicare Advantage plans with Part D is the price you’ll pay for your prescriptions. Each plan has its own formulary (a list of prescriptions) that it covers. That’s why the prices of individual prescription drugs vary widely among plans.
What to do if your doctor is out of network?
If they are out-of-network, ask the doctor to bill your insurance company or you can seek reimbursement from the Medicare Advantage plan, at the out-of-network level, as long as the doctor hasn’t opted out completely.
Is a PPO plan more expensive than an HMO?
See Plans. A PPO (Preferred Provider Organization) plan will generally cost you a little more in premiums than an HMO and have slightly higher copayments. However, it will include out-of-network coverage. That gives you a greater choice of doctors, which is important if you travel often or have many specialists to see.
Does Medicare have a closed network?
Some Medicare Advantage plans – particularly HMOs – have “closed” networks. That means that your insurer will only pay the medical professionals that are part of their network, and won’t pay for you to see anyone else. Of course, some HMOs are so huge that they have thousands of doctors signed up who take their insurance, especially around large metropolitan areas.
Is HMO coverage good?
Not good. If you have an HMO, you can call your insurer before traveling and ask for a list of its doctors in that area. Typically, HMO coverage is best near major cities. Being able to travel and still have coverage is one of the strengths of Medicare Advantage PPO plans over Medicare Advantage HMOs.
What is Medicare Part A?
Medicare Part A is hospital inpatient coverage for people with Original Medicare, whereas Part B is medical coverage for doctor visits, tests, etc.... and Medicare Part B. Medicare Part B is medical coverage for people with Original Medicare.
How much is the deductible for Medicare 2021?
In Original Medicare, you’ll pay the Part A deductible ($1,452 in 2021) plus a 20 percent coinsurance for all Medicare-approved costs (e.g., your doctor, tests, medications, supplies, etc.). And if you required ambulance transportation to get to the hospital, you’ll pay 20 percent of that cost, too.
What states have Medigap?
Medigap protections cited above are mandated by federal law. However, states have the ability to add additional protection if they so choose. These states have specific rules: 1 California – The birthday rule in California allows you to change policies within a 60-day window. The birthday rule begins 30 days before your birthday and ends 30 days after. Residents can switch to a policy with the same or less coverage. 2 Connecticut – Guaranteed issue year-round. Residents can make changes to their Medigap policy at any time. 3 Maine – Residents have an extension on the standard Medicare Advantage “trial right” rule. In Maine, you can “try” a Medicare Advantage plan for up to three years. You have 90 days after dropping the policy to buy a Medigap policy with guaranteed issue rights. 4 Missouri – If you have a Medigap policy, you can switch plans within 60 days of your enrollment anniversary. 5 New York – Resident may enroll in a Medigap plan without underwriting throughout the year. 6 Oregon – The birthday rule applies in Oregon. 7 Vermont – Residents can enroll in a Medigap plan without underwriting throughout the year. 8 Washington – Allows residents to switch Medigap plans (except for Plan A) at any time.
What is Medicare Supplement?
Medicare Supplements are additional insurance policies that Medicare beneficiaries can purchase to cover the gaps in their Original Medicare (Medicare Part A and Medicare Part B) health insurance coverage.... offers solid protection from deductibles.
What is a copay in health insurance?
, copayments. A copayment, also known as a copay, is a set dollar amount you are required to pay for a medical service....
What is out of pocket medical expenses?
out-of-pocket costs. Out-of-pocket costs (aka, out-of-pocket medical expenses) are costs that a beneficiary must pay because their health insurance does not cover them . Out-of-pocket costs are found in the deductibles, copayments, and coinsurance outlined in each health... (deductibles, coinsurance, and copayments).
What is guaranteed issue?
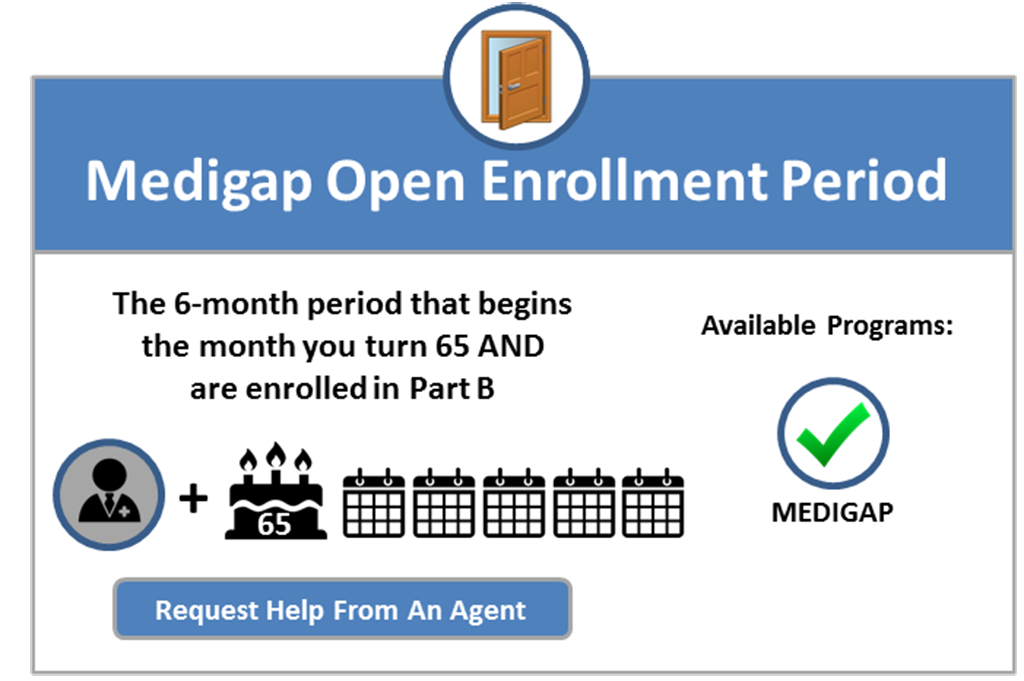
Guaranteed-issue is a right granted to Medicare beneficiaries and applies to Medicare Supplement insurance (aka, Medigap plans). All states and the federal government enforce this essential right, which protects Medicare beneficiaries from medical underwriting.... and cannot be turned down.
