What is an MSP code for Medicare?
The 14-value code should only be used for an individual entitled to Medicare and was in an accident or other situation where no-fault or liability insurance is involved.Feb 15, 2016
What are MSP codes?
What is the purpose of the MSP questionnaire?
What is an MSP plan?
Is MSP required for Medicare Advantage plans?
How do I bill a MSP claim?
- Complete the claim form CMS-1500 or electronic equivalent in the usual manner.
- Report all claim coding usually required for the services including charges for all Medicare-covered services, not just the balance remaining after the primary payer's payment.
How often must MSP be completed?
Following the initial collection, the MSP information should be verified once every 90 days.
Are MSP questionnaire required?
How do you know if Medicare is primary or secondary?
What are the benefits of MSP?
- Cost saving and easier Budgeting. Most small and medium businesses are finding it very expensive to employ competent IT personnel to run their IT operations. ...
- Access to the Experts. ...
- Proactive Support and Quick Response time. ...
- Ready infrastructure. ...
- Better Business Focus.
What is not covered by MSP?
How does healthcare work in BC?
B.C's publicly-funded health care system ensures that all eligible B.C. residents have access to medically necessary health care services through the Medical Services Plan and to eligible prescription medications, medical supplies, and pharmacy services through the PharmaCare program.
Who is authorized to use CPT?
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials of Centers for Medicare and Medicaid Services (CMS) internally within your organization within the United States for the sole use by yourself, employees and agents .
Is CPT a warranty?
CPT is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this agreement.
What is the primary payer code for Medicare Part A?
Beneficiary must have Medicare Part A entitlement (enrolled in Part A) for this provision to apply. Primary Payer Code = G.
What is primary payer code?
Primary Payer Codes Primary Payer codes are not reported by the provider via electronic submission of a MSP claim. Primary Payer codes are applied to the claim upon transfer to the Fiscal Intermediary Standard System (FISS) based on the corresponding electronic data reported. Primary Payer Codes of A to L (except C) must match MSP VC reported on claim. For example, MSP VC 12 = Primary Payer Code A, etc.
What is the VC code for conditional payment?
Accident/Medical Payment Coverage – Date of accident/injury for which there is medical payment coverage. Reported with VC 14 or VC 47. If filing for a Conditional Payment, report with Occurrence Code 24.
What is an EGHP?
EGHP is a multi- or multiple-employer plan that elects to pay secondary to Medicare for employees and spouses aged 65 and older for those participating employers who have fewer than 20 employees. 29. Disabled beneficiary and/or family member's LGHP is secondary to Medicare.
What is the VC code for accident related to employment?
Accident/Employment-Related - Date of an accident/injury related to beneficiary's employment. Reported with VC 15 or VC 41. If filing for a Conditional Payment, report with Occurrence Code 24.
What is the code for no fault insurance?
Reported with VC 14 or 47. If filing for a Conditional Payment, report with Occurrence Code 24.
Is EGHP secondary to Medicare?
To navigate directly to a particular type of code, click on the type of code from the following list: Beneficiary's and/or spouse's EGHP is secondary to Medicare. Beneficiary and/or spouse are employed and there is an EGHP that covers beneficiary but either:
What is MSP in Medicare?
MSP provisions prevent Medicare paying items and services when patients have other primary health insurance coverage. In these cases, the MSP Program contributes:
What is Medicare Secondary Payer?
The Medicare Secondary Payer (MSP) provisions protect the Medicare Trust Fund from making payments when another entity has the responsibility of paying first. Any entity providing items and services to Medicare patients must determine if Medicare is the primary payer. This booklet gives an overview of the MSP provisions and explains your responsibilities in detail.
Why does Medicare make a conditional payment?
Medicare may make pending case conditional payments to avoid imposing a financial hardship on you and the patient while awaiting a contested case decision.
What is a COB in health insurance?
Coordination of Benefits (COB) allows plans to determine their payment responsibilities. The BCRC collects, manages, and uploads information to the Common Working File (CWF) about patients’ other health insurance coverage. Providers, physicians, and other suppliers must collect accurate MSP patient information to ensure that claims are filed properly.
Does Medicare pay first when there is no fault?
no-fault pays first when there’s Ongoing Responsibility for Medicals (ORM) reported. Medicare doesn’t make a payment.
Can Medicare make a payment?
Medicare can’t make payment when payment “has been made or can reasonably be expected to be made” under liability insurance (including self-insurance), no-fault insurance, or a WC law or plan of the United States, called a primary plan.
Who pays first for Medicare?
Primary payers must pay a claim first. Medicare pays first for patients who don’t have other primary insurance or coverage. In certain situations, Medicare pays first when the patient has other insurance coverage.
Is CPT copyrighted?
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All rights reserved. CPT is a registered trademark of the American Medical Association (AMA).
Is CPT a warranty?
CPT is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this agreement.
What is the MSP Auxiliary File number?
As a result of MSP litigation settlement agreements CMS negotiated, records were added to the MSP Auxiliary file under contractor number 33333 (litigation settlement). Under the settlement agreements, CMS was to receive records for only those Medicare beneficiaries for which Medicare was secondary payer per a settlement agreement However, some data provided to CMS contain records for Medicare beneficiaries covered under a retirement group health plan or supplemental plan. These records were added to the CWF, MSP Auxiliary File. As these erroneous records are identified, beneficiaries, providers and the primary health plan have been notifying contractors that the records need to be corrected to again reflect Medicare as primary. All MSP Auxiliary File records, including these litigation records, need to be corrected and complete to maintain the integrity of the MSP Auxiliary File. As they become aware of an erroneous record, intermediaries and carriers are to advise the COBC via ECRS.
What happens when the MSP effective date is not correct?
When this happens, the contractor shall advise the COB, via ECRS, of the need to change the MSP effective date and shall provide the COBC with documentation to substantiate the change.
What is the DX code for fractures?
Fractures are currently identified in the 800-829 DX code range. Codes within the 800 - 804 category (Fracture of Skull) are not related to codes within the 805 - 809 category (Fracture of the Neck and Trunk). For instance, if a beneficiary CWF MSP auxiliary record contains a DX code 800.2, but an 806.1 DX code is received on an incoming claim, CWF and the contractor shall not assume that the 806.1 DX code is related to the 800.2 DX code on the MSP record. Development actions by the contractor are required in this situation. Following are a few more specific examples:
What is the CWF MSP data base?
The CWF MSP data base integrity is totally dependent upon COBC input, supported by input by FIs and carriers to the COBC. The COBC is responsible for submitting to CWF MSP information it believes to be of the highest quality. It shall investigate information thoroughly before making changes to an existing CWF MSP auxiliary record.
How many MSP records can be stored in CWF?
maximum number of 17 MSP auxiliary records may be stored in CWF for each beneficiary. The COBC is responsible for deletion of a record when the maximum storage is exceeded using the following priority:
Can a beneficiary have MSP?
An MSP situation cannot exist when a beneficiary has GHP coverage (i.e., working aged, disability and ESRD) and is entitled to Part B only. CWF will edit to prevent the posting of these MSP records to CWF when there is no Part A entitlement date. Currently, if a contractor submits an Electronic Correspondence Referral System (ECRS) transaction to the coordination of benefits (COB) contractor to add a GHP MSP record where there is no Part A entitlement, the contractor will receive a reason code of 61. The COB contractor's system cannot delete these types of records once the records are posted to CWF by a contractor. Beginning April 2002 CWF will create a utility to retroactively delete all MSP GHP records where there is no Part A entitlement.
What is MSP billing?
MSP Billing & Coding. The MSP provisions apply to situations when Medicare is not the beneficiary’s primary health insurance coverage. Providers are responsible for gathering MSP data to determine whether or not Medicare is the primary payer by asking Medicare beneficiaries questions concerning the beneficiary’s MSP status.
What is Medicare's value code?
Medicare uses the amount the provider is obligated to accept as payment in full in its payment calculation. In such cases, the provider reports in value code 44 the amount it is obligated to accept as payment in full. Medicare considers this amount to be the provider’s charges.
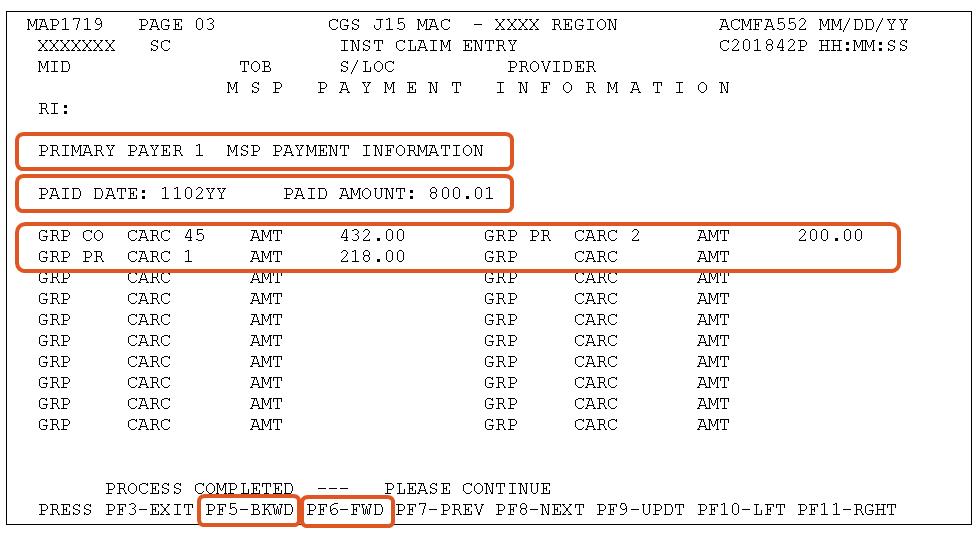
Why is it important to code CAS segments?
It is important for providers to code the CAS segments of their claims accurately so that Medicare will make the correct MSP payments. We created a Claim Adjustment Segment Coding Worksheet to help better understand CAS segments.
What is a payer code?
Payer Codes identify the type of insurance coverage.
What section of the claim must a provider indicate a denial of coverage?
Providers must indicate in the remarks section of the claim any denial reason from the primary insurance (when applicable).
When will MSP reject claims?
MSP claims will reject when the claim does not balance. The most common error is when the primary claim adjustment amounts found in the Claim Adjustment Segment (CAS) segments and the amount paid by the primary in the AMT segment do not equal the total charge.
When billing a claim and there is an open file that is diagnosis based for the patient and none of the diagnosis
When billing a claim and there is an open file that is diagnosis based for the patient and none of the diagnosis codes are related to the open file , indicate in remarks “Not related to open segment”.
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is a term used when Medicare is not responsible for paying first on a healthcare claim. The decision as to who is responsible for paying first on a claim and who pays second is known in the insurance industry as “coordination of benefits.”
What is Medicare data match?
This data match identifies persons that have had earnings in a given tax year. If a Medicare beneficiary and/or the spouse of a beneficiary has had earnings, that signifies employment, which means it is possible they also had Group Health Plan insurance coverage. A questionnaire is then sent to the employer inquiring about possible coverage that is primary to Medicare. If coverage exists or existed, dates of coverage are obtained, as well as the name and address of the insurer. Records obtained through this process are generally very reliable. 21
What is BCRC in Medicare?
The Benefits Coordination & Recovery Center (BCRC) consolidates the activities that support the identification, collection, management, and reporting of other primary insurance coverage for Medicare beneficiaries. They also collect and supply information on supplemental prescription drug coverage. The BCRC updates the Medicare systems with other insurance information.
What happens if a Medicare report is rejected?
If the record is rejected, the submitter is expected to research the record and submit a correction.
What is management of other insurance information?
Management of other insurance information is an ongoing process. Other insurance information for Medicare beneficiaries constantly changes. For example, Working Aged Medicare beneficiaries or their spouses retire, pending Liability cases get resolved, No-Fault insurance benefits become exhausted, and supplemental prescription drug coverage is dropped. All of these circumstances require updates to existing other insurance occurrences. All of the changes that occur must be updated on Medicare’s systems. The BCRC ensures appropriate updates are made to Medicare’s systems of records. 25
What is a group health plan?
A Group Health Plan is health coverage sponsored by an employer or employee organization (such as a union) for a group of employees, and possibly for dependents and retirees as well. The term GHP includes self-insured plans, plans of government entities (Federal, State, and local), and employee organization plans such as union plans, employee health and welfare funds, or other employee organization plans. The term also includes “employee-pay-all” plans which receive no financial contributions from the employer. The term does not include self-employed persons. 7
Is Medicare Supplement the same as Medicare Secondary Payer?
The term Medicare supplement (i. e., Medigap) should not be confused with Medicare Secondary Payer. Medicare supplemental is a private health insurance policy designed specifically to fill some of the “gaps” in Medicare’s coverage when Medicare is the primary payer. Medigap policies typically pay for expenses that Medicare does not pay for, such as deductible or coinsurance amounts or other limits under the Medicare program. Private "Medigap" insurance and Medicare secondary payer law and regulations are not the same. A “Medigap” policy is not a Medicare program benefit.