In many instances, Medicare Part B covers ultrasound testing in an outpatient setting. Preventative services such as examinations, lab tests and screening, supplies and other types of medically required outpatient care are included in Part B plans. While Part B is optional, your monthly premium may go up if you don’t sign up for it.
Full Answer
What does Medicare cover for outpatient hospital services?
Outpatient hospital services. Medicare Part B (Medical Insurance) covers Medically necessary diagnostic and treatment services you get as an outpatient from a Medicare-participating hospital. Covered outpatient hospital services may include: Emergency or observation services, which may include an overnight stay in the hospital or outpatient...
Does Medicare cover outpatient diagnostic services?
diagnostic and treatment services you get as an outpatient from a Medicare-participating hospital. Covered outpatient hospital services may include: Emergency or observation services, which may include an overnight stay in the hospital or outpatient clinic services, including same-day surgery. Laboratory tests billed by the hospital.
What procedures are covered by Medicare?
What Procedures Does Medicare Cover? Medicare covers a number of inpatient and outpatient procedures. Find out if your procedure will be covered by Medicare, how much it may cost and what you can do to get help paying for it. Medicare Part A and Part B make up what is known as “Original Medicare.”
Does Medicare Part a cover the emergency room?
The Emergency room is an outpatient service. Only if a doctor orders admission will Part A charges occur. The ambulance is also a Part B service. Does Medicare Part A cover outpatient surgery? Any outpatient services have coverage under Part B. Only an inpatient surgery would fall under Part A benefits.
What procedures are covered by Medicare?
Click on each item in the list to learn more about how it's covered by Medicare and how much they may cost.Acupuncture.Air Ambulance transportation.Annual physicals.Auto accident injury treatment.Back surgery.Blood tests.Breast reduction surgery.Long term care in a hospital or skilled nursing facility.More items...
What is an example of an outpatient procedure?
Common procedures that are now routinely performed on an outpatient basis include tonsillectomies, hernia repairs, gallbladder removals, some cosmetic surgeries, and cataract surgeries. Given the millions of procedures performed every year, complications from outpatient procedures are relatively uncommon.
What does the outpatient portion of a policy cover?
Covered outpatient hospital services may include: Emergency or observation services, which may include an overnight stay in the hospital or services in an outpatient clinic (including same-day surgery). Laboratory tests billed by the hospital.
Does Medicare cover in office procedures?
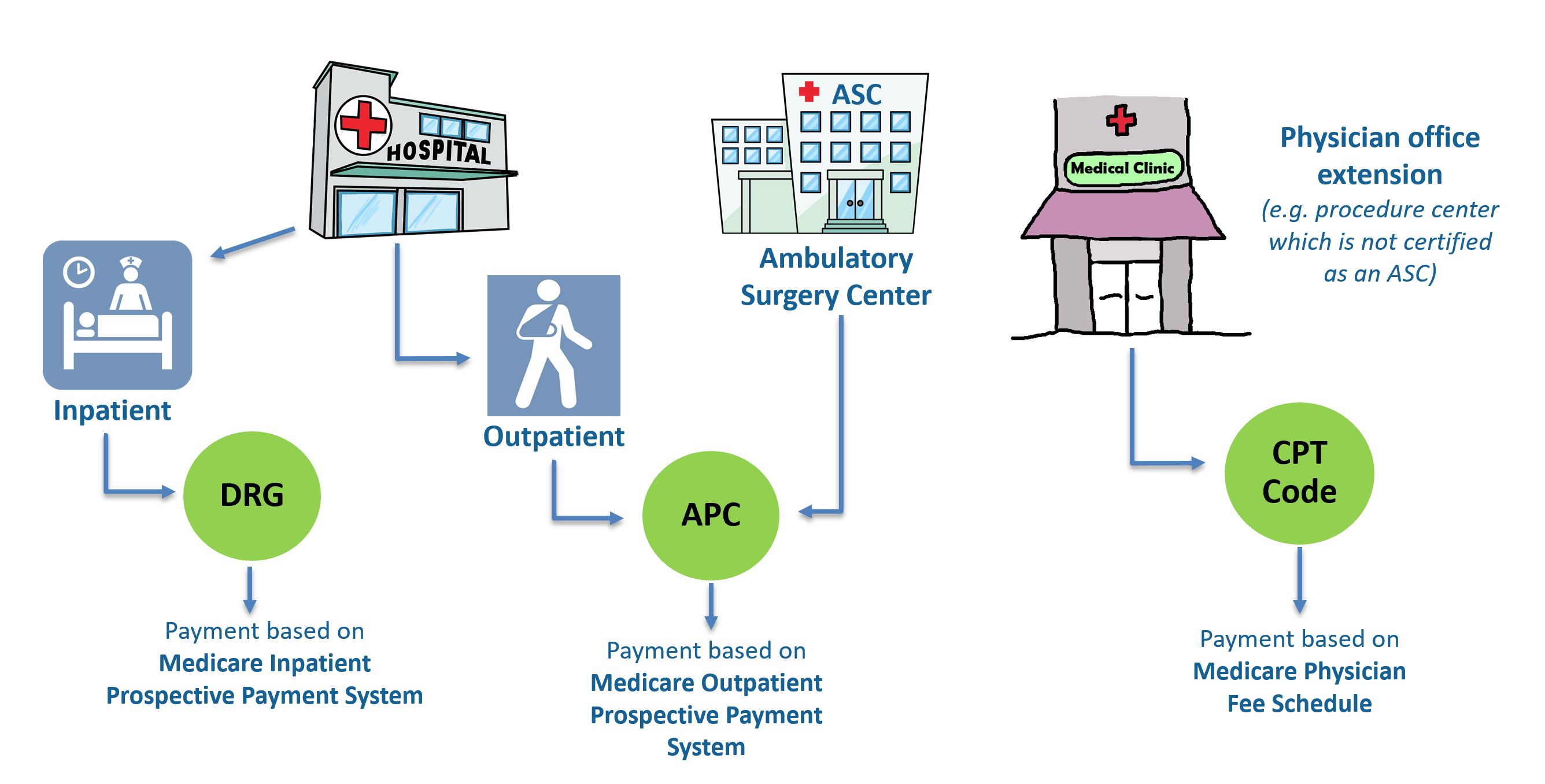
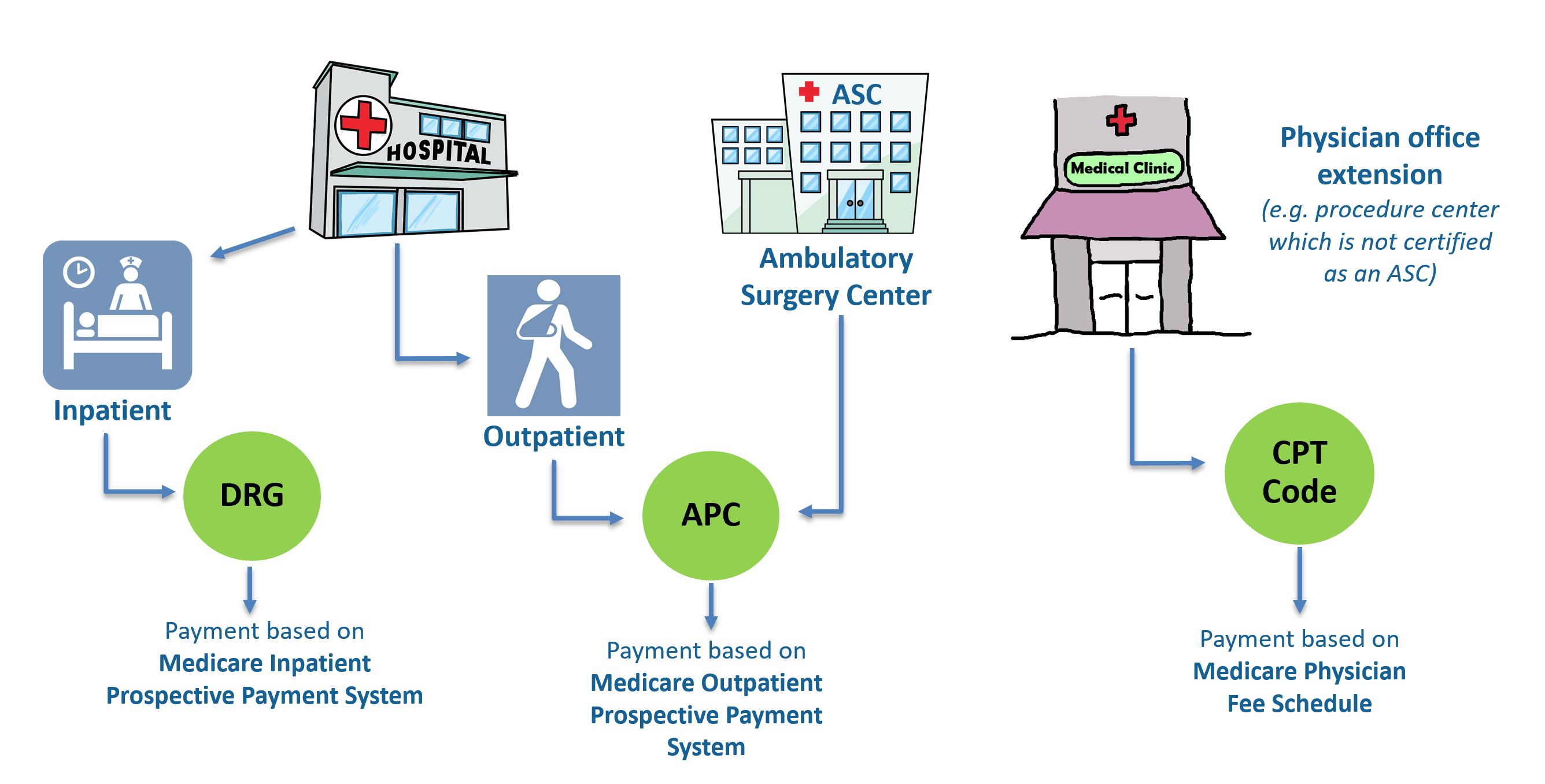
Outpatient procedures usually take place in a doctor's office, an ambulatory surgical center or a hospital. Medicare Part B covers outpatient surgery. Typically, you pay 20% of the Medicare-approved amount for your surgery, plus 20% of the cost for your doctor's services.
What procedures can be performed in an ASC?
ASC ProceduresDiagnostic Laparoscopy. ... Laser Laparoscopy. ... Laparoscopic Hysterectomy.Laparoscopic hysterectomy is a procedure to remove the uterus through a few tiny incisions in the abdomen below the navel. ... Hysteroscopy (with or without endometrial ablation) ... D&C. ... Tubal Ligation. ... Laser Ablation of Condyloma.More items...
What is done outpatient?
Outpatient surgery allows a person to return home on the same day that a surgical procedure is performed. Outpatient surgery is also referred to as ambulatory surgery or same-day surgery.
How does Medicare define outpatient?
You're an outpatient if you're getting emergency department services, observation services, outpatient surgery, lab tests, X-rays, or any other hospital services, and the doctor hasn't written an order to admit you to a hospital as an inpatient.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
Which of the following is excluded from Medicare coverage?
Non-medical services, including a private hospital room, hospital television and telephone, canceled or missed appointments, and copies of x-rays. Most non-emergency transportation, including ambulette services. Certain preventive services, including routine foot care.
Is day surgery covered by Medicare?
Despite paying for private health insurance, the total cost of your day surgery may not be covered by your policy. Regarding any private day hospital admission, all procedures carry a government-assigned Medicare item number.
What tests are covered by Medicare?
Medicare Part B covers outpatient blood tests ordered by a physician with a medically necessary diagnosis based on Medicare coverage guidelines. Examples would be screening blood tests to diagnose or manage a condition. Medicare Advantage, or Part C, plans also cover blood tests.
Does Medicare cover elective surgeries?
Medicare covers many expenses related to essential surgical procedures, but it does not cover elective surgeries (such as cosmetic surgeries) unless they serve a medical purpose.
What does Medicare Part A cover?
Part A provides coverage for inpatient hospital services. Part B covers outpatient care and durable medical equipment (DME). Original Medicare coverage typically requires the care to be “medically necessary” in order for it to be covered by ...
What is the number to call for Medicare?
1-800-557-6059 | TTY 711, 24/7. The services and items below are not necessarily a complete list of procedures that are covered by Original Medicare. Click on each item in the list to learn more about how it’s covered by Medicare and how much they may cost. Acupuncture. Air Ambulance transportation.
Does Medicare Advantage cover prescriptions?
Many Medicare Advantage plans also offer prescription drug coverage, and some plans offer benefits like dental, vision, hearing, gym and wellness program memberships and more, all of which aren't typically covered by Original Medicare.
Does Medicare cover assisted living?
Procedures Medicare typically doesn't cover may be covered by some Medicare Advantage plans. Some procedures that aren't typically covered by Original Medicare may sometimes be covered by certain Medicare Advantage (Medicare Part C) plans. These procedures may include but are not limited to the following: Assisted living.
Does Medicare cover coinsurance?
Certain other restrictions may apply, depending on the procedure you need. Depending on the type of service you get and how Medicare covers it, you may face certain deductible, coinsurance and/or copayment costs.
How does hospital status affect Medicare?
Inpatient or outpatient hospital status affects your costs. Your hospital status—whether you're an inpatient or an outpatient—affects how much you pay for hospital services (like X-rays, drugs, and lab tests ). Your hospital status may also affect whether Medicare will cover care you get in a skilled nursing facility ...
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. , coinsurance. An amount you may be required to pay as your share of the cost for services after you pay any deductibles.
What is an ED in hospital?
You're in the Emergency Department (ED) (also known as the Emergency Room or "ER") and then you're formally admitted to the hospital with a doctor's order. Outpatient until you’re formally admitted as an inpatient based on your doctor’s order. Inpatient after your admission.
How long does an inpatient stay in the hospital?
Inpatient after your admission. Your inpatient hospital stay and all related outpatient services provided during the 3 days before your admission date. Your doctor services. You come to the ED with chest pain, and the hospital keeps you for 2 nights.
When is an inpatient admission appropriate?
An inpatient admission is generally appropriate when you’re expected to need 2 or more midnights of medically necessary hospital care. But, your doctor must order such admission and the hospital must formally admit you in order for you to become an inpatient.
What is a copayment?
copayment. An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug. A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor's visit or prescription drug.
Is an outpatient an inpatient?
You're an outpatient if you're getting emergency department services, observation services, outpatient surgery, lab tests, or X-rays, or any other hospital services, and the doctor hasn't written an order to admit you to a hospital as an inpatient. In these cases, you're an outpatient even if you spend the night in the hospital.
How much is the deductible for inpatient surgery in 2021?
Medicare Part A covers the majority of surgical costs, and you will pay a deductible of $1,484 in 2021 in addition to 20% of doctor fees.
How long do you have to be in a skilled nursing facility to be eligible for Medicare?
In order for traditional Medicare to pay for a stay in a skilled nursing facility, you need to have been admitted for at least three consecutive days as an inpatient. Medicare Advantage plans have the option of waiving the three-day rule.
Can an inpatient be performed in an ASC?
Surgeries on the inpatient-only list cannot be performed in an Ambulatory Surgery Center (ASC). In fact, CMS publishes a specific list of outpatient surgeries that can be performed at an ASC. This list is referred to as Addendum AA. 2
Is there an inpatient only list?
Every year CMS releases an updated inpatient-only surgery list. 1 The surgeries on this list are not arbitrarily selected. Due to the complexity of the procedure, the risk for complications, the need for post-operative monitoring, and an anticipated prolonged time for recovery, CMS understands that these surgeries require a high level of care. Many of these are cardiovascular surgeries and procedures .
Can you perform surgery in a hospital?
For these reasons, all procedures on the Inpatient Only list must be performed in a hospital. However, that does not mean that other surgeries won 't be performed in a hospital setting. If a surgery is not on the inpatient-only list and not on addendum AA, it must also be performed in a hospital.
Can you transfer an ASC patient to a hospital?
This may necessitate transferring a patient to a nearby hospital. Since care in an ASC is limited to a 24- hour stay, if a patient required more time for recovery, the patient would also need to be transferred to a hospital. For these reasons, all procedures on the Inpatient Only list must be performed in a hospital.
Does Medicare pay for surgery?
Updated on November 12, 2020. Surgery doesn't come cheap and you will want to know how (or if) Medicare is going to pay for it long before you go under the knife. Simply put, Medicare will cover your surgery under either Part A or Part B. The latter could cost you thousands more in out of pocket expenses.
Why are inpatient only procedures performed?
First, staff involved at each level, including clinical, financial, and administrative, may not be aware that patients must be admitted as inpatients before certain procedures are performed. Educating staff can be a complex process that begins at the point of surgery scheduling and registration, and carries through to denial of payment. Creating a hospital policy that promotes communication will encourage consistency in training and rapid identification of an inpatient-only procedure during various points of care.
Why is it important to create a hospital policy that promotes communication?
Creating a hospital policy that promotes communication will encourage consistency in training and rapid identification of an inpatient-only procedure during various points of care. Second, inpatient-only procedures may not always be planned.
Value Based Purchasing Program for Ambulatory Surgical Centers
The Affordable Care Act requires the Secretary of Health and Human Services to develop a plan to implement a value-based purchasing (VBP) program for payments under the Medicare program for ambulatory surgical centers (ASCs). The Secretary submits a report to Congress containing this plan.
Ambulatory Surgical Center (ASC) Approved HCPCS Codes and Payment Rates
These files contain the procedure codes which may be performed in an ASC under the Medicare program as well as the ASC payment group assigned to each of the procedure codes. The ASC payment group determines the amount that Medicare pays for facility services furnished in connection with a covered procedure.
ASC CENTER
For a one-stop resource for Medicare Fee-for-Service (FFS) ambulatory surgical centers, visit the Ambulatory Surgical Centers (ASC) Center page.
What is inpatient vs outpatient?
Many people ask, “what is inpatient vs. outpatient?” Inpatient care means you’re admitted to the hospital on a doctor’s order. As soon as your admission occurs, you’re an inpatient care recipient.
How long can you stay outpatient?
Outpatient is when you get care without admission or have for a stay of fewer than 24 hours, even if overnight. Health services you get at a facility can be outpatient care.
Is an emergency room outpatient or inpatient?
For example, when you visit the emergency room, you’re initially outpatient, because admission to the hospital didn’t happen. If your visit results in a doctor ordering admission to the hospital, then your status becomes inpatient. The care you get is inpatient until discharge. Despite a stay in the hospital, your care may be outpatient ...
Does Medicare cover skilled nursing?
Medicare only covers a skilled nursing facility when a qualifying inpatient hospital stay precedes the need for such services. You need to get inpatient hospital care for at least three consecutive days to qualify. It will include the first day that you’re inpatient and exclude the day of discharge.
Does Medicare cover Part B coinsurance?
If Medicare covers, the Medigap policy will cover; however, you must have a plan that includes the Part B coinsurance. Plan K and Plan L only cover a portion of the costs. Whereas, Medigap Plan G or Plan F covers the Part B coinsurance as well as excess charges.
