In Year 4 (2020), an Advanced APM Entity must do one of the following for its eligible clinicians to meet the criteria of Qualifying APM Participants (QPs): Receive at least 50% of its Medicare Part B payments through the Advanced APM See at least 35% of its Medicare patients through the Advanced APM
Full Answer
What are advanced advanced alternative payment models (APMs)?
advanced alternative payment modules (Advanced APMs) include new ways for CMS to reimburse health care providers for care provided to Medicare beneficiaries; providers who participate in an Advanced APM through Medicare Part B may earn an incentive payment for participating in the innovative payment model alternative payment models (APMs)
What is an Accountable Care Organization (APM)?
Accountable care organizations Providers who participate in an Advanced APM through Medicare Part B may earn an incentive payment for participating in the innovative payment model. Which documents health care services provided to a patient and includes patient demographic (or identification) data,
What are the benefits of qualifying for Advanced Practice Manager (APM)?
Qualifying APM Participant Potential Benefits: Select your performance year. Advanced APMs allow eligible clinicians to become a QP for an opportunity to receive a 5 percent APM incentive payment and to be excluded from MIPS.
What is an other-payer Advanced Medicare Advantage plan (APM)?
Other-Payer Advanced APMs are non-Medicare payment arrangements that meet criteria that are similar to Advanced APMs under Medicare. Learn more about All-Payer Advanced APMs.
Which does a provider participate in through Medicare Part B to earn an incentive?
Terms in this set (65) include new ways for CMS to reimburse health care providers for care provided to Medicare beneficiaries; providers who participate in an Advanced APM through Medicare Part B may earn an incentive payment for participating in the innovative payment model.
What is an APM provider?
An Alternative Payment Model (APM) is a payment approach that gives added incentive payments to provide high-quality and cost-efficient care. APMs can apply to a specific clinical condition, a care episode, or a population.
What is an advanced APM?
Advanced Alternative Payment Models (APMs) Advanced Alternative Payment Models (APMs) is a track of the Quality Payment Program that offers incentives for meeting participation thresholds based on your levels of payments or patients through Advanced APMs.
Who is eligible for APM?
Access to Disability Employment Services Have a diagnosed injury, illness or disability. Are aged at least 14 to 65. Are at or above the minimum legal working age in your state or territory. Are able to work at least eight hours per week (with support when required)
What are the criteria to be considered an advanced alternative payment model APM )?
In order for a clinician to receive a bonus payment through an APM, the APM must be considered an Advanced APM (AAPM) by meeting the following eligibility requirements: Use of quality measures comparable to measures under MIPS; Use of a certified electronic health record (EHR) technology; and.
What is Medicare APM?
An APM is a payment model that deviates from traditional fee-for-service. The traditional process for reimbursing physicians for their services under Medicare Part B is to pay for services according to the Physician Fee Schedule (PFS). Under this approach, practices are paid a set fee for each service delivered.
Is Medicare Advantage an APM?
Other Payer Advanced APMs are non-Medicare Fee For Service (FFS) payment arrangements with other payers such as Medicaid, Medicare Health Plans (including Medicare Advantage, Medicare-Medicaid Plans, 1876 Cost Plans, and Programs of All Inclusive Care for the Elderly (PACE) plans), payers with payment arrangements in ...
What is the difference between MIPS and APM?
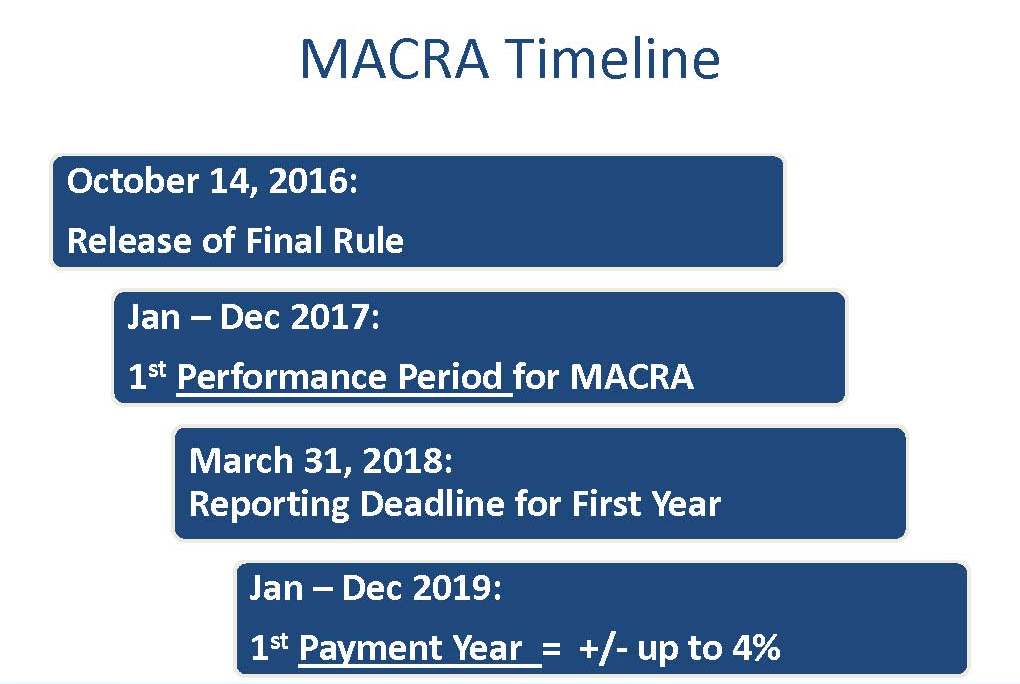
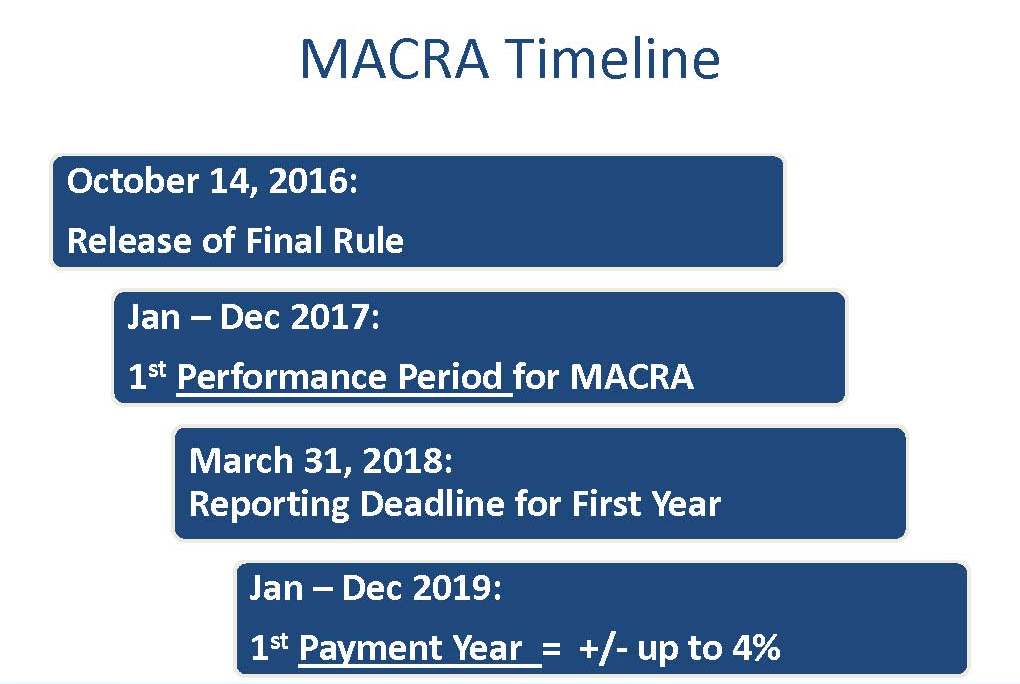
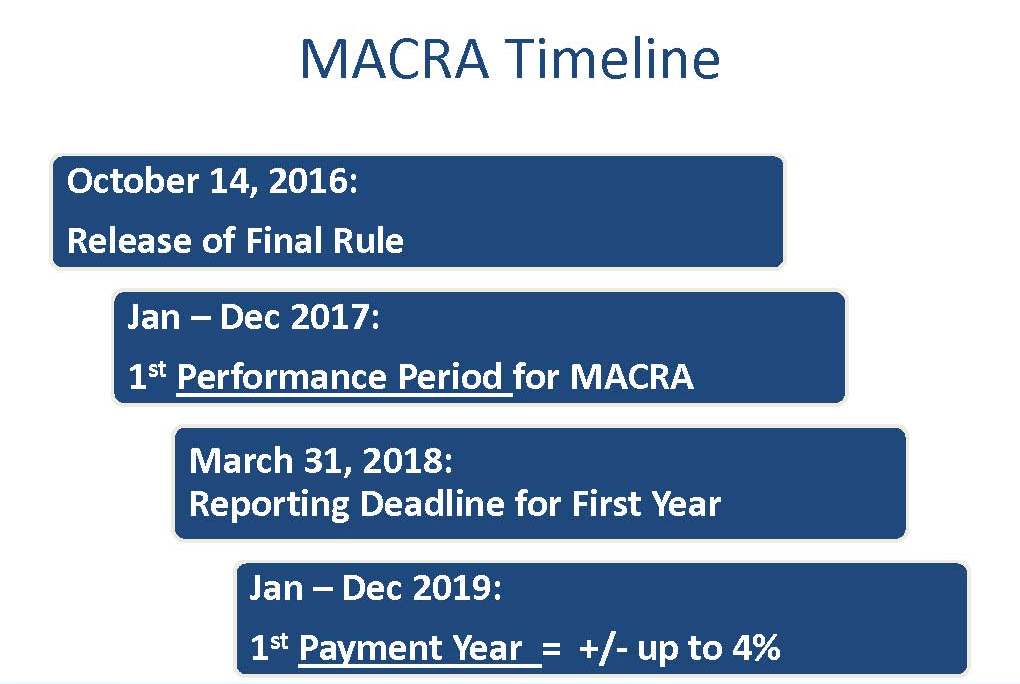
MIPS stands for Merit-Based Incentive Payment System, while APM stands for Alternative Payment Model. Health care providers need to begin the verification process this year, and the first payments under these systems will be made in 2019. Both MIPS and APMs are processes that use value-based payment models.
Is PCF an advanced APM?
PCF is expected to qualify as a Medicare Advanced APM. Additionally, for any private payers that participate, it would count as an Other Payer Advanced APM towards the All Payer Combination Threshold. Practices must use Certified EHR Technology (CEHRT) to qualify, which is required of all Advanced APMs.
What is APM performance pathway?
The APM Performance Pathway (APP) is a MIPS reporting and scoring pathway for MIPS eligible clinicians who are also participants in MIPS APMs. The APP is designed to reduce reporting burden, create new scoring opportunities for participants in MIPS APMs, and encourage participation in APMs.
How is APM funded?
While APM delivers programs and services to individual clients, the services are funded via contracts, licences, grants, and individual fee for service arrangements. APM's customers include government departments and agencies (at a local, state, and federal level), employers and insurers.
What is APM employable?
Employable Me is a new recruitment platform from APM which helps job seekers to find employment more simply and quickly. By connecting job seekers to employers who need to hire new staff, Employable Me helps people looking for work find sustainable employment in roles they are best suited for.
How much of Medicare Part B is APM?
Receives at least 40% of its Medicare Part B payments through the Advanced APM. Sees at least 25% of its Medicare Part B patients through the Advanced APM. While QPs will be excluded from MIPS reporting requirements, Partial QPs can opt to participate in MIPS and will be scored using the APM Scoring Standard.
What is an APM in healthcare?
As the name suggests, though, an APM is simply a model of a new, or alternative, payment approach that’s based on quality and cost metrics.
What is the APM requirement?
The APM must require that APM Entities include at least one MIPS eligible clinician on a participation list. The APM must base payment on quality measures and cost/utilization.
What is MIPS APM?
CMS identifies these as MIPS APMs. MIPS APMs include APMs that don’t meet Advanced APM criteria.
What is an APM model?
As the name suggests, though, an APM is simply a model of a new, or alternative, payment approach that’s based on quality and cost metrics. Examples of APMs include: Pay-for-Performance. Bundled Payment Models (also known as Episode-based Payment Models)
How to become a QP for Medicare Part B?
To become a QP through the All-Payer Combination Option, an eligible clinician must still meet minimum thresholds under the Medicare arrangement, which include: Receive at least 25% of Medicare Part B payments through the Medicare Advanced APM. See at least 20% of Medicare patients through the Medicare Advanced APM.
How much Medicare Part B payment do you need to be a partial QP?
Partial QPs must still meet Medicare’s minimum thresholds: Receive at least 20% of Medicare Part B payments through the Medicare Advanced APM.
What is an advanced APM?
An Advanced APM is a track of the Quality Payment Program that offers a 5 percent incentive for achieving threshold levels of payments or patients through Advanced APMs. If you achieve these thresholds, you are excluded from the MIPS reporting requirements and#N#payment adjustment#N#.
What is alternative payment model?
An Alternative Payment Model (APM) is a payment approach that gives added incentive payments to provide high-quality and cost-efficient care. APMs can apply to a specific clinical condition, a care episode, or a population.
What is QP in 2019?
Starting in#N#Performance Year#N#2019, eligible clinicians will be able to become Qualifying Alternative Payment Model Participants (QPs) through the All-Payer Option. To attain this Option, eligible clinicians must participate in a combination of Advanced APMs with Medicare and Other-Payer Advanced APMs. Other-Payer Advanced APMs are non-Medicare payment arrangements that meet criteria that are similar to Advanced APMs under Medicare.
Is MIPS APM?
Most Advanced APMs are also MIPS APMs. MIPS Eligible clinicians participating in Advanced APMs are included in MIPS if they do not meet the threshold for payments or patients sufficient to become a. (QP). The MIPS eligible clinician will be scored under MIPS according to the APM scoring standard.
AAPM: One of Two Payment Tracks Under the Quality Payment Program (QPP)
The Advanced Alternative Payment Model (AAPM) offers physicians incentives to provide high-quality, cost-effective care and move away from the fee-for-service (FFS) model. The other track created under MACRA is the Merit-based Incentive Payment System (MIPS) track.
AAPMs: Criteria for Qualifying Participants
For the 2020 performance period, an AAPM entity must do one of the following for all its eligible clinicians to be qualifying participants (QPs):
What is an Alternative Payment Model (APM)?
MACRA defines any of the following as a qualifying Alternative Payment Model (APM):
Which Alternative Payment Models (APMs) are eligible for the bonus?
Only AAPMs are eligible for the 5% bonus. The following APMs apply to primary care and are (AAPMs) for the performance period beginning in 2020:
When will I know my QP status?
CMS will make QP determinations three times during the performance period. QPs will be identified on the following schedule: March 31 of the performance period; June 30 of the performance period; and August 31 of the performance period.
What is the All-Payer Combination Option?
The All-Payer Combination Option allows ECs to become QPs or Partial QPs by meeting QP thresholds through a pair of calculations that assess a combination of both Medicare Part B covered professional services furnished through Advanced APMs and services furnished through Other Payer AAPMs.
What is an Other Payer Advanced APM?
Other Payer APMs are non-Medicare fee-for-service payment arrangements that meet the AAPM criteria – required use of CEHRT, payment based on quality measures comparable to those in MIPS, and assumption of nominal risk.
How will I be paid under an APM?
If you are a QP, from 2019 through 2024, you will receive an annual 5% lump-sum bonus. The amount of the bonus is based on your Medicare Part B payments from the previous year’s claims. This bonus will be in addition to the incentive paid through existing contracts with the AAPM.
What are the mandated reporting and disclosure requirements for group life and health plans?
mandated reporting and disclosure requirements for group life and health plans (including managed care plans), permitted large employers to self-insure employee health care benefits, and exempted large employers from taxes on health insurance premiums. Evaluation and Management (E/M)
What is a contract between a policyholder and a third-party payer or government program?
contract between a policyholder and a third-party payer or government program to reimburse the policyholder for all or a portion of the cost of medically necessary treatment or preventive care by health care professionals. health insurance exchange. see health insurance marketplace. health insurance marketplace.
What is a consumer driven health plan?
consumer-driven health plan (CDHP) health care plan that encourages individuals to locate the best health care at the lowest possible price, with the goal of holding down costs; also called consumer-directed health plan.
What is the BBA Act?
Balanced Budget Act of 1997 (BBA) addresses health care fraud and abuse issues, and provides for Department of Health and Human Services (DHHS) Office of the Inspector General (OIG) investigative and audit services in health care fraud cases.
Why did the Hill Burton Act provide grants to hospitals?
provided federal grants for modernizing hospitals that had become obsolete because of a lack of capital investment during the Great Depression and WWI (1929-1945); in return for federal funds, facilities were required to provide services free, or reduced rates, to patients unable to pay for care.
What is E/M in healthcare?
Evaluation and Management (E/M) services that describe patient encounters with providers for evaluation and management of general health status. Federal Employees' Compensation Act (FECA) provides civilian employees of the federal government with medical care, survivors' benefits, and compensation for lost wages.