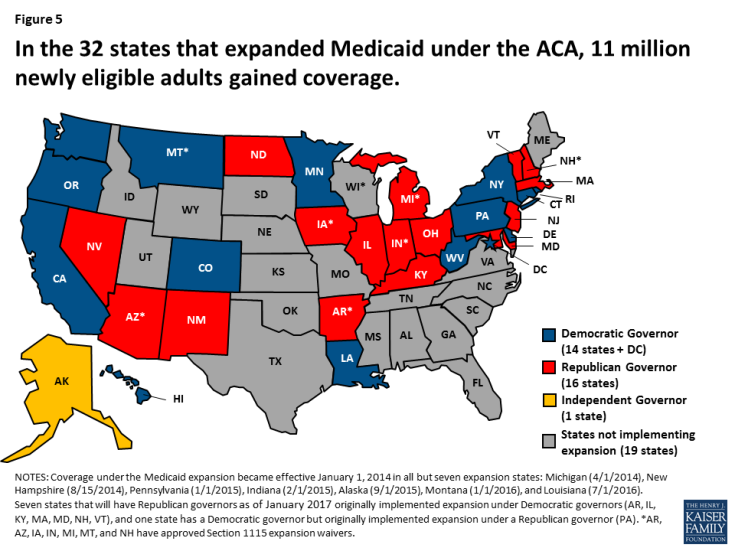
The 17 states are: California, Colorado, Connecticut, Maine, Maryland, Massachusetts, Minnesota, Montana, Nevada, New Jersey, New York, Oregon, Pennsylvania, Rhode Island, Vermont, Washington, and Wisconsin.
Full Answer
Does Medicaid pay for gender reassignment surgery?
Gender Reassignment Surgery. The Centers for Medicare & Medicaid Services has not issued a national coverage determination on gender reassignment surgery, and therefore, leaves coverage determination up to local Medicare Administrative Contractors (MACs).
Does Medicare cover transgender surgery?
Many transgender people seek further surgery to make their outer appearance match more closely with their internal gender. For example, a transgender woman may want facial feminization surgery to reduce the size of her chin and nose. Medicare usually only covers transition surgery that alters a person’s primary sex characteristics.
Does health insurance cover gender reassignment surgery in Iowa?
While the current policy still generally excludes gender-affirming care from coverage, which includes medical treatments, surgical procedures, hormones, and other medications, it does allow coverage specifically for medication related to gender transition if the beneficiary has a court order affirming his or her gender change.41 Iowa.
Does Medicare cover hormone therapy for gender reassignment?
In preparation for gender reassignment surgery, Medicare will cover hormone therapy through Part D prescription drug coverage. If you have Original Medicare, you will need to be enrolled in a stand-alone Prescription Drug Plan (PDP).
Does Medicare cover gender reassignment surgery?
Medicare provides coverage for gender reassignment surgery, although it needs to be deemed as medically necessary. A person can appeal the decision if surgery is denied. While Medicare coverage is nationwide, there may be state variations in policies and guidelines.
Does Medicare cover gender affirming care?
Medicare covers gender affirmation procedures when they're deemed medically necessary. Procedures covered by Medicare may include hormone therapy, gender affirmation surgeries, and counseling before and after surgery.
Does Medicare cover facial feminization?
Medicare does not cover certain cosmetic surgery procedures, such as laser hair removal and facial feminization surgery, because these are not considered medically necessary.
Is gender reassignment covered?
Many health plans are still using exclusions such as “services related to sex change” or “sex reassignment surgery” to deny coverage to transgender people for certain health care services.
How do you pay for gender reassignment surgery?
Consider these options to pay for gender-affirming surgery and care:Online personal loan.Credit union personal loan.Credit card.CareCredit.Home equity line of credit.Family loan.
Does Medicare cover hormone therapy?
Medicare covers medically necessary hormone therapy. These medications are part of Medicare Part D lists of covered medications and should be covered when prescribed. Private Medicare plans should provide coverage for these prescriptions.
What does condition code 45 mean?
Ambiguous Gender CategoryPolicy: For Part A claims processing, institutional providers shall report condition code 45 (Ambiguous Gender Category) on any outpatient claim related to transgender or hermaphrodite issues.
How much is top surgery Australia?
Top surgery can cost between $4,000 - $18,000 out of pocket, depending on the technique and surgeon.
Does the government cover gender reassignment surgery?
Medicare covers necessary gender reassignment surgery. It also pays for doctor visits and lab work as you go through the transition process. Also, prescription plans usually cover hormone treatments for transgender people.
What does Black FOLX mean?
Definition of folx : folks —used especially to explicitly signal the inclusion of groups commonly marginalized Having women teach other women matters. Women of color. Transgender women. Disabled women.
How much does a gender switch cost?
Gender reassignment surgeries are expensive. Bottom surgeries can cost about $25,000 and top (breast surgeries) from $7,800 to $10,000. Facial and body contouring are also costly. More employer insurance policies, and those sold under the Affordable Care Act, now cover at least some gender reassignment surgeries.
Description Information
Please Note: This may not be an exhaustive list of all applicable Medicare benefit categories for this item or service.
National Coverage Analyses (NCAs)
This NCD has been or is currently being reviewed under the National Coverage Determination process. The following are existing associations with NCAs, from the National Coverage Analyses database.
Do you need to get preauthorization for a transition surgery?
The National Center for Transgender Equality recommends that you get pre-authorization from your Advantage plan before you get healthcare related to your transition. Also, unlike Medicare, Advantage plans rely on networks.
Does Medicare pay for breast removal surgery?
Medicare Part B covers outpatient services. If you’re hospitalized for your surgery, Part A pays for it. With Medicare, you can see any doctor that accepts Medicare.
Does Medicare pay for gender dysphoria surgery?
For Medicare to pay for your surgery, your doctor must diagnose you with gender dysphoria or gender identity disorder. Also, your doctor must confirm that the operation is necessary. You may have to show counseling and hormone therapy before coverage approval.
Does Medicare cover gender reassignment surgery?
Medicare covers necessary gender reassignment surgery. It also pays for doctor visits and lab work as you go through the transition process. Also, prescription plans usually cover hormone treatments for transgender people. Yet, Medicare won’t pay for surgery to make your physical features more masculine or feminine.
Can you have gender reassignment surgery with Medicare?
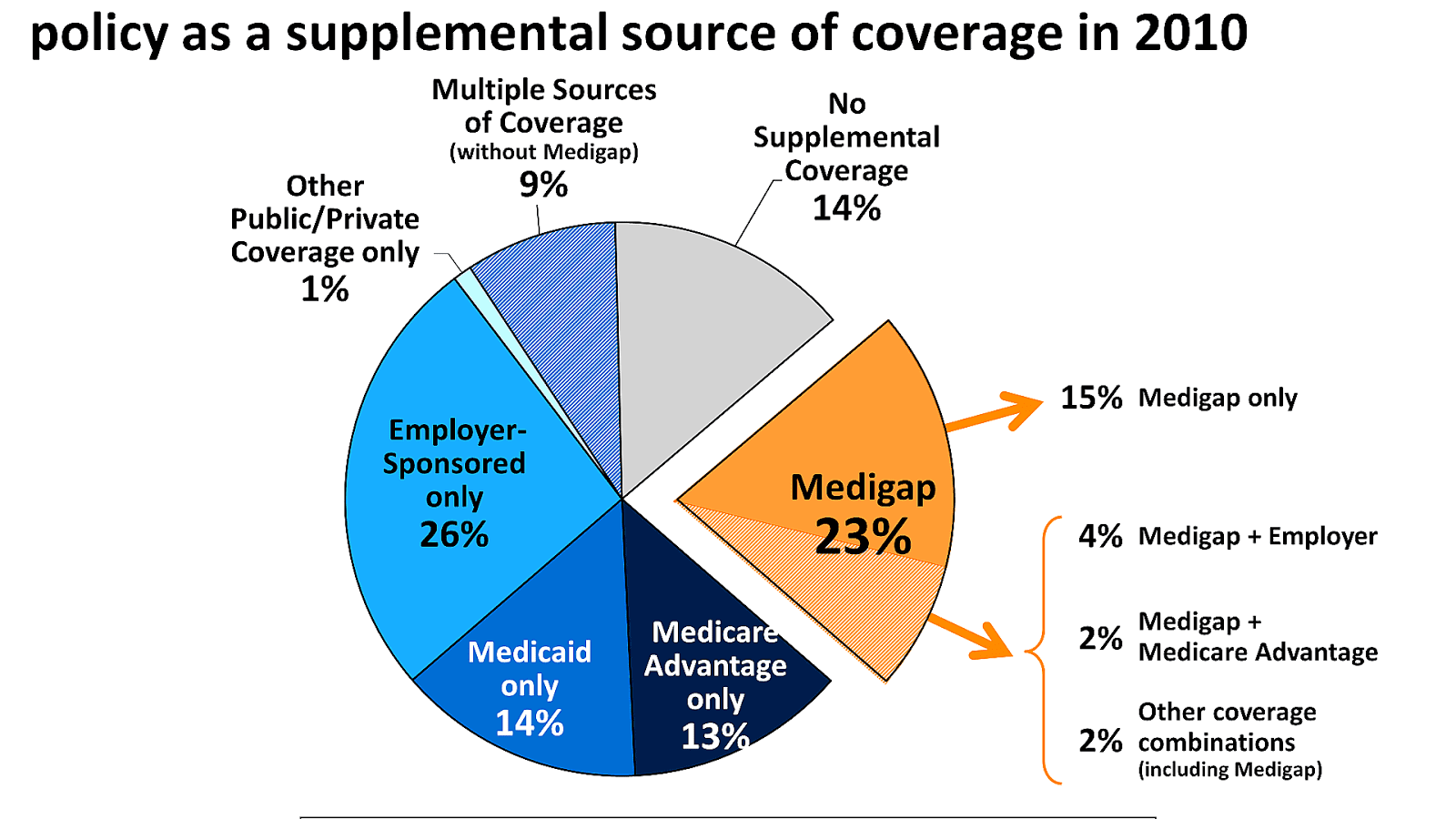
Gender reassignment surgery is a special procedure, and you’ll want to choose an expert healthcare team. But if you only have Medicare, your costs can be high. A Medigap plan can make gender reassignment surgery more affordable. Let the experts at MedicareFAQ help you find the right Medigap plan for your needs.
Does Medicare cover facial feminization?
But, Medicare won’t pay to change a person’s appearance because Medicare considers it cosmetic and not considered medically necessary. So, this means Medicare won’t cover facial feminization, breast augmentation, hair removal, face or body contouring, or vocal cord surgeries.
Does Medicare cover Part B deductible?
If Medicare covers, then your plan will too. But, if Medicare denies your claim, Medigap won’t pay it either. For example, if you have Plan G, you pay your premium and the Part B deductible. Then, the plan covers the charges Medicare would’ve sent you.
Does Medicare cover hormone therapy?
Hormone Therapy. In preparation for gender reassignment surgery, Medicare will cover hormone therapy through Part D prescription drug coverage. If you have Original Medicare, you will need to be enrolled in a stand-alone Prescription Drug Plan (PDP). Many Medicare Advantage plans include prescription drug coverage.
Does Medicare cover transgender people?
Routine preventive care and transition-related services are vitally important to prepare for gender reassignment surgery, but there can be some confusion about Medicare coverage for transgender individuals. Medicare is a federal program that provides health insurance for individuals 65 years of age or older, and some people under the age ...
Does Medicare Advantage cover prescriptions?
Many Medicare Advantage plans include prescription drug coverage. If coverage is initially denied due to inconsistency with Social Security gender records, an appeal can be made to provide a Medicare recipient with access to medications they require to meet their specific needs.
Does Medicare cover gender reassignment surgery?
The Centers for Medicare & Medicaid Services has not issued a national coverage determination on gender reassignment surgery, and therefore, leaves coverage determination up to local Medicare Administrative Contractors (MACs). According to CMS, coverage will be based on whether the surgery is considered “reasonable and necessary for the individual beneficiary after considering the individual’s specific circumstances. For Medicare beneficiaries enrolled in Medicare Advantage (MA) plans, the initial determination of whether or not surgery is reasonable and necessary will be made by the MA plans.”
What are the exclusions for transgender people?
Plans with transgender exclusions. Many health plans are still using exclusions such as “services related to sex change” or “sex reassignment surgery” to deny coverage to transgender people for certain health care services. Coverage varies by state. Before you enroll in a plan, you should always look at the complete terms ...
Is transgender health insurance discriminatory?
These transgender health insurance exclusions may be unlawful sex discrimination . The health care law prohibits discrimination on the basis of sex, among other bases, in certain health programs and activities.
Can insurance companies limit sex-specific preventive services?
Your health insurance company can’t limit sex-specific recommended preventive services based on your sex assigned at birth, gender identity, or recorded gender — for example, a transgender man who has residual breast tissue or an intact cervix getting a mammogram or pap smear.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
Gender Dysphoria (GD) is defined by the Diagnostic and Statistical Manual of Mental Disorders - Fifth Edition, DSM-5™ as a condition characterized by the "distress that may accompany the incongruence between one’s experienced or expressed gender and one’s assigned gender" also known as “natal gender”, which is the individual’s sex determined at birth.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
Which states exclude transition services?
Twelve states also specifically exclude transition-related services from health benefits for state employees. On the other hand, Maine announced last month that it would begin covering transition services under Medicaid, and judges in Wisconsin, Minnesota and California recently ruled that health-care providers in those states can’t discriminate ...
Is being transgender a biological imperative?
Sprigg said being transgender is a lifestyle choice, not a biological imperative — a view at odds with that of medical professional organizations, such as the AMA, the American Psychiatric Association and the American Psychological Association.
Is gender reassignment surgery cosmetic?
Lesbian, gay, bisexual, transgender and queer and/or questioning groups strongly dispute the notion that gender reassignment surgery is cosmetic, akin to elective plastic surgery.