
Does Medicare cover Pap smears and pelvic exams?
Screening Pap Tests & Pelvic Exams MLN Booklet Page 5 of 12 ICN MLN909032 December 2020 Medicare Part B covers HPV screening for all female patients ages 30–65 once every 5 years with a Pap test. Coverage Frequency Table 1 describes how often Medicare Part B covers screening Pap tests, pelvic exams, and . HPV screening. Table 1.
Does Medicare cover well woman exams?
Coding and Billing a Medicare AWV. G0438: Annual wellness visit, includes a personalized prevention plan of service (PPS), initial visit. G0439: Annual wellness visit, includes a personalized prevention plan of service (PPS), subsequent visit. G0468: Federally qualified health center (FQHC) visit, IPPE, or AWV; a FQHC visit that includes an initial preventive physical examination …
What is the code to Bill a pelvic exam?
Sep 28, 2015 · How to bill out for an annual Well Woman Exam for a patient covered by Medicare? Unless you specifically evaluate a patient for both the AWV and a Well Woman Exam, do not bill out the AWV. A primary care physician providing the annual exam will also include the pelvic and breast exam and a pap smear collection.
What are screening Pap tests and pelvic examinations?
Aug 12, 2011 · Covered Services. Medicare covers the following screening exams in conjunction with a Well Woman Exam: 1. G0101 Cervical or Vaginal Cancer Screening; Pelvic and Clinic Breast Examination. a. G0101 is reimbursed by Medicare every two years unless the patient is considered high risk, and then it is allowed on an annual basis.
Does G0101 and Q0091 need a modifier?
As of February 21, 2011, the screening services of Q0091 and/or G0101 are considered for separate reimbursement when reported in addition to a significant and separately identifiable E/M service. Modifier 25 must be appended to the E/M service for the screening services to be separately reimbursed.
How do I bill a Pap smear to Medicare?
Bottom line: Use Q0091 when obtaining a screening Pap smear for a Medicare patient.Feb 27, 2019
Does Medicare cover pap and pelvic?
Medicare covers Pap tests and pelvic exams to check for cervical and vaginal cancers at no cost to you. Clinical breast exams are also covered. You can receive these preventive screenings once every 24 months, or more frequently if you have certain risk factors.
How do I code a Medicare Well Woman Exam?
If a Medicare beneficiary requests a well-woman exam in conjunction with a “Welcome to Medicare” visit or an AWV, codes G0101 and Q0091 are billable and paid in addition to the “Welcome to Medicare” exam or AWV. To ensure payment, verify the date of the patient's last claim to Medicare for these services.
What is the CPT code for pelvic exam?
Preventive E/M or Gynecological Exam & Pap Smear Collection The appropriate medical E/M office visit code (99202-99215) may be reported with modifier 25 in addition to Q0091.
What is the CPT code for gynecological exam?
Z01. 419: Encounter for gynecological examination (general) (routine) without abnormal findings.
Are pelvic exams covered by Medicare?
Medicare Part B covers a Pap smear, pelvic exam, and breast/chest exam once every 24 months. You may be eligible for these screenings every 12 months if: You are at high risk for cervical or vaginal cancer. Or, you are of childbearing age and have had an abnormal Pap smear in the past 36 months.
Does Medicare pay for Pap smears after 65?
Since most Medicare beneficiaries are above the age of 65, Medicare does continue to cover Pap smears after this age. Medicare Part B will continue to pay for these Pap smears after the age of 65 for as long as your doctor recommends them.
Is cervical screening covered by Medicare?
Medicare covers most of the cost of a Cervical Screening Test, so if your chosen cervical screening doctor offers 'bulk billing', there should be no cost to you for the test.
How do I bill a Well Woman Exam?
A gynecologic or annual women's exam should be reported using the age-appropriate preventive medicine visit procedure code and a gynecological diagnosis code (e.g. Z01. 419).May 23, 2007
Can G0101 and 99213 be billed together?
Can you please clarify this? Medicare will allow you to submit G0101 in addition to an evaluation and management (E/M) service (e.g., 99213) if the E/M service is significant and separately identifiable from the G0101 service.
What is the ICD 10 code for routine annual gynecological visit and exam with Pap smear?
411 and Z01. 419 (routine gynecological exam with or without abnormal findings) indicate that the codes include a cervical Pap screening and instruct us to add additional codes for HPV screening and/or a vaginal Pap test.Oct 12, 2017
What is included in a well woman exam?
If a patient is seen by her primary care physician (PCP) for an annual, the provider will also include the pelvic and breast exam and a pap smear collection.
What determines whether a patient has the G0101 or Q0091?
High-Risk Factors determine whether or not a patient may have the G0101 and Q0091 on an annual basis. If a patient is considered high risk, then these screening tests may be done annually.
What is an advance beneficiary notice?
Advance Beneficiary Notices (ABNs) An Advance Beneficiary Notice is a Medicare Waiver of Liability that providers are required to give a Medicare patient for services provided that may not be covered or considered medically necessary.
What is an ABN for Medicare?
It also notifies Medicare that the patient acknowledges that certain procedures were provided and that the patient will be personally responsible for full payment if Medicare denies payment for a specific procedure or treatment.
Does Medicare change billing policies?
Medicare billing policies are constantly changing at CMS and with your local carrier, so before you do anything, check with them and your coding specialist to make sure you are billing correctly.
What are Medicare modifiers?
Appropriate Medicare Modifiers. Certain Medicare modifiers are required when billing with an ABN. 1. GA Modifier: Waiver of Liability Statement Issued as Required by Payer Policy. This modifier indicates that an ABN is on file, and allows the provider to bill the patient if not covered by Medicare. 2.
What is the purpose of annual exam?
The purpose of the annual exam includes screening for disease, assessing risk of future medical problems, promoting a healthy lifestyle, and updating vaccinations. Aspects of the annual exam may include all or some of the following: 1. Review of History. 2.
Who can use CPT code for pap smear?
The only CPT ® codes specifically for pap smears are for use by a pathologist, for the interpretation of the cytology specimen. CPT® codes in the lab section, 88000 series, should not be reported by the office physician who collects the pap smear. Those codes are used by the pathologist who provides the interpretation of the pap smear.
What is a Pap smear?
Pap smear during a preventive medicine services for a commercial patient. If the patient presents for a preventive medicine service , the pelvic exam is part of the age and gender appropriate physical exam, as described by CPT ® codes in the 99381—99397 series of codes.
What is the CPT code for a physical exam?
CPT codes 99381–99397 include an age and gender appropriate history and physical exam. Billing G0101 would be double billing for that portion of the exam. G0101 Cervical or vaginal cancer screening; pelvic and clinical breast examination (Ca screen; pelvic/breast exam )
Does Medicare pay for Pap smears?
Pap smear during a Medicare wellness visit. Medicare doesn’t pay for routine services, but does pay for a cervical/vaginal cancer screening with a breast exam. (Medicare pays for wellness visits, not discussed here.
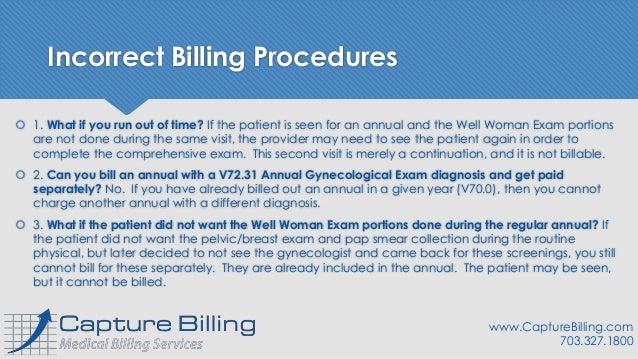
What if you run out of time for a well woman exam?
What if you run out of time? If the patient is seen for an annual and the Well Woman Exam portions are not done during the same visit, the provider may need to see the patient again in order to complete the comprehensive exam. This second visit is merely a continuation, and it is not billable.
What determines whether a patient has the G0101 or Q0091?
High Risk Factors determine whether or not a patient may have the G0101 and Q0091 on an annual basis. If a patient is considered high risk, then these screening tests may be done annually.
What is an advanced beneficiary notice?
An Advanced Beneficiary Notice is a Medicare Waiver of Liability that providers are required to give a Medicare patient for services provided that may not be covered or considered medically necessary . ABNs do not apply to services that are specifically excluded from Medicare coverage, such as an annual.
Who is Manny Oliverez?
Manny Oliverez, CPC, is a 20-year healthcare veteran and the CEO and co-founder of Capture Billing, a medical billing services company located outside of Washington, D.C. He teaches the nation’s physicians, administrators, and medical practices how to maximize billing and revenue cycle management processes. Manny also frequently posts articles and videos on his award-winning healthcare blog. For more information on Manny and his company, please visit his website, or call (703)327-1800. And if you’re on LinkedIn, please look for him there too.READ MORE
Is well woman screening covered by Medicare?
Because specific well woman screening components of the routine annual exam are covered by Medicare, these are billed out separately. These screenings are carved out from the provider’s usual fee for preventive service, because they are allowable and reimbursable by Medicare. The remainder balance is the patient’s financial responsibility. The total fee does not change, only how it is billed and who pays.
What is an AWV in Medicare?
KEY POINTS. The Medicare annual wellness visit (AWV) and the initial preventive physical examination (IPPE) provide a number of benefits to patients and physicians, but many physicians still do not provide them. Medicare wellness visits can help physicians address care gaps and report quality measures important in pay-for-performance systems.
What are pay for performance measures?
Many pay-for-performance measures can be addressed during Medicare wellness visits, including these, which are associated with the following programs: Core Quality Measures Collaborative (Collaborative), the Integrated Healthcare Association’s California Value Based P4P Program (IHA ), and the National Committee for Quality Assurance’s Healthcare Effectiveness Data and Information Set (HEDIS). Measures used by the Medicare Shared Savings Program (MSSP) 2018 and 2019 reporting years are also listed.
Why are wellness visits important?
Medicare wellness visits can help physicians address care gaps and report quality measures important in pay-for-performance systems. When billed correctly and delivered efficiently along with other covered Medicare preventive services, AWVs can boost practice revenue.
Who is Dr. Cuenca?
Dr. Cuenca is a board-certified family medicine and sports medicine physician with MemorialCare Medical Group in Mission Viejo, Calif. He is also a member of FPM ’s Editorial Advisory Board. ...
What is the benefit of AWV?
The main benefit of the AWV to patients is the creation of a personalized prevention plan, a written plan that can help guide their preventive care decisions for the next five to 10 years. This plan includes age-appropriate preventive services, recommendations offered by both the U.S. Preventive Services Task Force and the Advisory Committee on Immunization Practices, and personalized health advice that identifies risk factors and suggests referrals or programs to address them. 3
Do physicians have to provide AWVs?
Physicians and other health care providers do not offer AWVs to their Medicare patients for numerous reasons. Providing and documenting all of the required AWV elements efficiently can be challenging, and some practices may feel their staffing or electronic health record resources are too limited.
What is the code for a pelvic exam?
For a screening clinical breast and pelvic exam, Medicare patients can be billed using code G0101, “Cervical or vaginal cancer screening; pelvic and clinical breast examination.”. Knowing the codes as well as Medicare and private payer rules is crucial to get reimbursed for administering Pap smears.
What is a Pap test?
A Pap test is a simple and quick screening test conducted to obtain a smear of vaginal or cervical cells for cytological study. The human papillomavirus (HPV) test and the Pap test examine cells from a woman’s cervix. The Pap test looks at the cells to see if they are cancerous.
What is the code for papanicolaou smear?
Q0091 Screening papanicolaou smear; obtaining, preparing and conveyance of cervical or vaginal smear to laboratory. Using HCPCS code Q0091: Q0091 should be used when obtaining a screening Pap smear for a Medicare patient, though private payers may allow it along with a preventive medicine service (AAFP).
What is an IPPE in Medicare?
Initial Preventive Physical Examination (IPPE) The IPPE, known as the “Welcome to Medicare” preventive visit, promotes good health through disease prevention and detection. Medicare pays for 1 patient IPPE per lifetime not later than the first 12 months after the patient’s Medicare Part B benefits eligibility date.
How many times can you report ACP?
There are no limits on the number of times you can report ACP for a certain patient in a certain time period. When billing this patient service multiple times, document the change in the patient’s health status and/or wishes regarding their end-of-life care. Preparing Eligible Medicare Patients for the AWV.
What is routine physical exam?
Routine Physical Exam. Exam performed without relationship to treatment or diagnosis for a specific illness, symptom, complaint, or injury. ✘ Not covered by Medicare; prohibited by statute, however, the IPPE, AWV, or other Medicare benefits cover some elements of a routine physical. ✘ Patient pays 100% out-of-pocket.
What is advance directive?
“Advance directive” is a general term referring to various documents such as a living will, instruction directive, health care proxy, psychiatric advance directive, or health care power of attorney.
What is advance care planning?
Advance care planning including the explanation and discussion of advance directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified health care professional; each additional 30 minutes (List separately in addition to code for primary procedure) Diagnosis.
Does the AWV include HRA?
The AWV includes a HRA. See summary below of the minimum elements in the HRA. Get more information in the CDC’s A Framework for Patient-Centered Health Risk Assessments booklet, including: