Medicare is sending a Form 1095-B to people who had Medicare Part A coverage for part of <year>. The Affordable Care Act requires people to have health coverage that meets certain standards, also called qualifying health coverage or minimum essential coverage.
Part A helps cover your inpatient care in hospitals. Part A also includes coverage in critical access hospitals and skilled nursing facilities (not custodial or long-term care). It also covers hospice care and home health care.
Will I receive a 1095 from Medicare?
coverage is considered qualifying health coverage. If you have Part A, you may get IRS Form 1095-B from Medicare in the early part of the year. If you don't get Form 1095-B, don't worry. Not everyone will get this form from Medicare, and you don't need to have it to file your taxes.
Does Medicare provide a 1095?
Medicare Part A (Hospital Insurance) coverage is considered qualifying health coverage. If you have Part A, you may get IRS Form 1095-B from Medicare in the early part of the year. If you don't get Form 1095-B, don't worry. Not everyone will get this form from Medicare, and you don't need to have it to file your taxes.
Does Medicaid send out a 1095?
If that’s the case, you’ll be able to claim the additional premium tax credit on your tax return, via the normal Form 8962 process. Form 1095-B is sent out by health insurance carriers, government-sponsored plans such as Medicare, Medicaid, and CHIP, and self-insured employers who aren’t required to send out Form 1095-C instead.
How to get 1095 a form from Medicaid online?
You can also request the form by:
- Calling 877-617-9906
- Sending an email to RA-PWPA1095-B@pa.gov
- Mailing a written request to your local county assistance office
Do I need a 1095-B for Medicare?
coverage is considered to be qualifying health coverage under the Affordable Care Act. If you have Part A, you can ask Medicare to send you an IRS Form 1095-B. In general, you don't need this form to file your federal taxes.
Do you get 1095-C from Medicare?
Form 1095-B is sent out by health insurance carriers, government-sponsored plans such as Medicare, Medicaid, and CHIP, and self-insured small employers (large employers, including those that are self-insured, send out Form 1095-C instead). This form is mailed to the IRS and to the insured member.
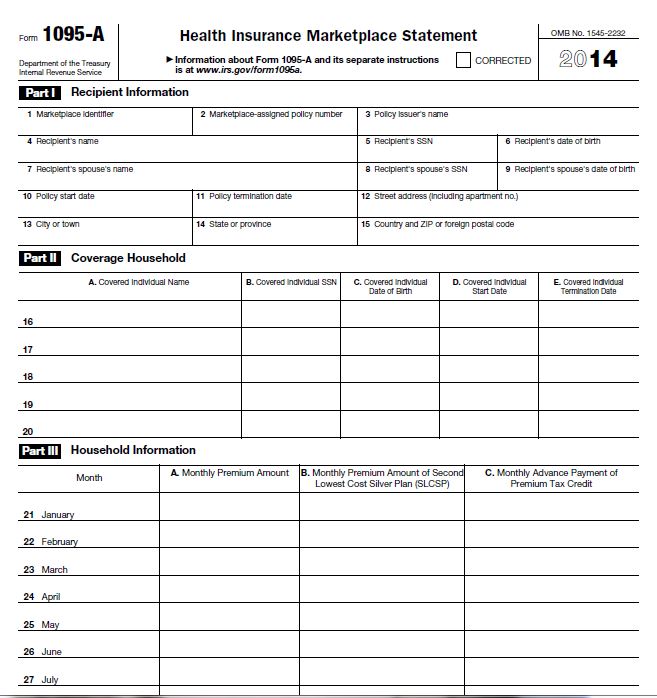
Is 1095-A and 1095-B the same?
Form 1095-A, Health Insurance Marketplace Statement, is provided by the Marketplace to individuals who enrolled or who have enrolled a family member in health coverage through the Marketplace. Form 1095-B, Health Coverage, is provided by insurance companies and other coverage providers.
Is there a difference between 1095-A and 1095-C?
The 1095-C shows that you had health insurance from a good-sized employer. The 1095-A shows that you bought health insurance from the Marketplace under the Affordable Care Act. If you have Marketplace insurance, then you must enter the 1095-A into TurboTax so it can produce a form 8962.
Do you report Medicare on taxes?
Your Medicare premiums, however, won't be taken out pretax. You'll need to deduct them when you file your taxes instead. This is the case even if you pay your premiums by having the money deducted from your Social Security retirement benefits check.
Does Medicare send 1099?
Medicare contractors send the 1099-MISC or 1099-INT (1099 Forms) to providers to report the payments made by the contractor for the calendar year. Providers who receive the 1099 Form are required to use its information as part of their tax reporting.
Do I need both 1095-A and 1095-B?
No, not all 1095 tax forms get reported. Only the 1095-A gets entered into TurboTax in the Health Insurance section. If you have a 1095-B, a form titled Health Coverage, the IRS does NOT need any details from this form.
What is 1095-B form used for?
The Form 1095-B is used as proof of Minimum Essential Coverage (MEC) when filing your state and/or federal taxes. It should be kept with your other tax information in the event the Internal Revenue Service (IRS) or Franchise Tax Board (FTB) requires you to provide it as proof of your health care coverage.
Do I need both 1095-B and 1095-C?
The 1094-C is the transmittal form that must be filed with the Form 1095-C. Form 1095-B is used to report certain information to the IRS and to taxpayers about individuals who are covered by minimum essential coverage and therefore are not liable for the individual shared responsibility payment.
What is a 1095 AB or C form?
Why do I need Form 1095-B or Form 1095-C? You'll need Form 1095-B or C to prove you had minimum essential coverage under the Affordable Care Act. The forms show the months of the year you and your dependents had insurance coverage.
What is 1095-C form used for?
Form 1095-C will indicate your name and the name of your large employer, the months during the prior calendar year when you were eligible for coverage, and the cost of the cheapest monthly premium you could have paid for coverage under your employer's health plan.
Who gets a 1095-C?
You will receive a copy of Form 1095-C from your qualifying employer if you are (or were) a full-time employee, even if you don't (didn't) participate in the employer's healthcare plan. You also will receive Form 1095-C if you were enrolled in a self-funded, employer-sponsored healthcare plan.
How to Find Your 1095-A Online
Note: Your 1095-A may be available in your HealthCare.gov account as early as mid-January, or as late as February 1. If you’re already logged in, s...
What’S on Form 1095-A and Why You Need It
1. Your 1095-A contains information about Marketplace plans any member of your household had in 2017, including: 1. Premiums paid 2. Premium tax cr...
How to Check Form 1095-A For Accuracy & What to Do If It's Wrong
1. Carefully read the instructions on the back. 2. Make sure it’s accurate. If anything about your coverage or household is wrong, contact the Mark...
Use The Information from Your 1095-A to “Reconcile”
Once you have an accurate 1095-A and second lowest cost Silver plan premium, you’re ready to fill out Form 8962, Premium Tax Credit.See a step-by-s...
Form 1095-A: Marketplace Insurance Statement
Form 1095-A is issued by state and federal marketplaces to individuals who had marketplace coverage for the year. This form is absolutely required...
Form 1095-B: Health Coverage
Form 1095-B is the catchall form that is issued for any type of coverage that is not reported on a Form 1095-A or C. This includes coverage from in...
Form 1095-C: Employer-Provided Health Insurance Offer and Coverage
Form 1095-C is issued by large employers – those that are required to offer coverage to employees or pay a penalty for failing to do so. This form...
Amended Return Relief For 1095-B and 1095-C Recipients
When filing without Form 1095-B or C, taxpayers should make a good faith effort to accurately report their insurance coverage status on their tax r...
What is a 1095-A?
Your 1095-A contains information about Marketplace plans any member of your household had in 2020, including: Premiums paid. Premium tax credits used.
What does 1095-A show?
In this case, the monthly enrollment premium on your Form 1095-A may show only the amount of your premium that applied to essential health benefits. You or a household member started or ended coverage mid-month. In this case, your Form 1095-A will show only the premium for the parts of the month coverage was provided.
Is the 1095-A premium higher than the 1095-A?
If any of these applied, the premium on your 1095-A is probably correct.
Do I need a 1095-A before filing taxes?
IMPORTANT: You must have your 1095-A before you file. Don’t file your taxes until you have an accurate 1095-A. Your 1095-A includes information about Marketplace plans anyone in your household had in 2020. It comes from the Marketplace, not the IRS.
Do I need to file Form 8962?
If you want to see if you qualify for a premium tax credit based on your final income, you can complete Form 8962 to find out. If you don't qualify for a premium tax credit, you don't have to include Form 8962 when you file your income taxes. Learn more about your taxes if you paid full price for a Marketplace plan.
What is a 1095-B?
Form 1095-B is the catchall form that is issued for any type of coverage not on a Form 1095-A or C. This includes coverage from insurance companies, the government (Medicaid, CHIP, Medicare Part A, TRICARE, VA, etc.), small self-insured employers, and more.
Who is required to file Form 1095-A?
Form 1095-A is sent by state and federal marketplaces to anyone who had marketplace coverage for the year . This form is absolutely required for taxpayers who received advance payments of the Premium Tax Credit (APTC) to help pay for health insurance coverage during the year.
What tax forms are used to report healthcare coverage?
With the passing of the Affordable Care Act, three new tax forms came into the scene: Form 1095 A, B, and C. These tax forms were used to report your healthcare coverage during a tax year. But, in 2019, the healthcare penalty went away. So many people were wondering if they need Form 1095 health insurance statements for their tax returns any longer.
What is a 1095-A?
Form 1095-A is your proof that you had health insurance coverage during the year , and it’s also used to reconcile your premium subsidy on your tax return, using Form 8962 (details below).
What does 1095-C mean?
For example, if you work for a large company and have access to coverage from your employer, but you opted to buy coverage in the exchange instead, you’d receive Forms 1095-A and 1095-C (the 1095-C would indicate that you were offered employer-sponsored coverage, even though you declined it).
What to do if 1095-A is delayed?
If delivery of your 1095-A is delayed or the information on it is incorrect, you can contact your exchange. For the 2020 plan year, however, the rules are different. People who received excess premium tax credits in 2020 do not have to repay them to the IRS, and do not even have to file Form 8962 at all.
When will the IRS issue 1095-B?
The latest extension, detailed in IRS Notice 2020-76, gives insurers and employers until March 2, 2021, to distribute Forms 1095-B and 1095-C to plan members and employees.
Do health insurance exchanges have a tax form?
The health insurance exchanges can also still provide exemptions from the individual mandate, which are necessary in order to enroll in a catastrophic health planif you’re 30 or older (note that the exchanges use their own form for this; it’s not a tax form).
Who is required to send out a 1095-C?
Form 1095-C. Form 1095-Cis sent out by large employers who are required to offer health insurance coverage as a provision of the ACA. This applies to employers with 50 or more full-time equivalent employees. Form 1095-C is sent to the IRS and to the employees.
Who sends out 1095-A?
Form 1095-A is sent out by the health insurance exchanges (HealthCare.gov or a state-based exchange, depending on the state). This form is mailed to the IRS and to the policyholder.
How to file 1095-A?
Before you file: 3 things to know about Form 1095-A 1 If you can’t find your 1095-A, check online. If your form didn’t come by mail or you can’t find it, check your online Marketplace account. When you follow these steps, be sure to choose your 2018 application, not your 2019 application. 2 Before you file, make sure your 1095-A is correct. Check basic health plan and household member information, and verify the premium for your second lowest cost Silver plan (SLCSP). If you find errors, contact the Marketplace Call Center. Don’t file your taxes until you have an accurate form. 3 You’ll use the information from your 1095-A to “reconcile” your premium tax credit. Once you have an accurate 1095-A and second lowest cost Silver plan premium, you’re ready to fill out Form 8962, Premium Tax Credit, and “reconcile.” You’ll compare the amount you used in 2018 to lower your monthly insurance payment with the actual premium tax credit you qualify for based on your final 2018 income. Get a step-by-step guide to reconciling.
What to do if 1095-A doesn't come?
If your form didn’t come by mail or you can’t find it, check your online Marketplace account. When you follow these steps, be sure to choose your 2018 application, not your 2019 application. Before you file, make sure your 1095-A is correct.
What form do I fill out to get a Silver Plan Premium Tax Credit?
Once you have an accurate 1095-A and second lowest cost Silver plan premium, you’re ready to fill out Form 8962, Premium Tax Credit, and “reconcile.”.