Medicare claim address, phone numbers, payor id – revised list
| State | State | IVR # | Claim mailing address | Appeal address |
| Florida | FL | 1-877-847-4992 | Medicare Part B Participating Providers ... | Medicare Part B Redetermination P.O. Box ... |
| Virgin Islands | VI | 1-877-847-4992 | Medicare Part B Participating Providers ... | Medicare Part B Redetermination P.O. Box ... |
| Arizona | AZ | 1-877-908-8431 | Medicare Part B P.O. Box 6704 Fargo, ND ... | Medicare Part B PO Box 6704 Fargo, ND 58 ... |
| Montana | MT | 1-877-908-8431 | Medicare Part B P.O. Box 6735 Fargo, ND ... | Medicare Part B PO Box 6735 Fargo, ND 58 ... |
Full Answer
How to file a Medicare appeal?
To increase your chance of success, you may want to try the following tips:
- Read denial letters carefully. ...
- Ask your healthcare providers for help preparing your appeal. ...
- If you need help, consider appointing a representative. ...
- Know that you can hire legal representation. ...
- If you are mailing documents, send them via certified mail. ...
- Never send Medicare your only copy of a document. ...
- Keep a record of all interactions. ...
How to get help when you have problems with Medicare?
What To Do If There Is A Medicare Billing Error, Or You Suspect One Occurred
- It could be an accident. Accidents happen—even with billion-dollar government programs. ...
- Make sure you’re not being scammed. On the other hand, an “accident” could disguise itself as fraud. ...
- Check with Social Security. ...
- Fill out the right form. ...
- Know who is billing you. ...
Where to file Medicare claims?
- Before filing claims electronically to Railroad Medicare, you must have an EDI enrollment packet on file with Palmetto GBA. ...
- View the Electronic Filing Instructions
- Palmetto GBA Interactive CMS-1500 Claim Form Instructions — This resource can also be helpful to providers who submit electronic claims. ...
How to appeal a Medicare claim denial decision?
Questioning a Medicare Claim
- The first level of appeal, described above, is called a “redetermination.”
- If your concerns aren’t resolved to your satisfaction at this level, you can file an appeal form with Medicare to advance your request to the second “reconsideration” level in which ...
- The third level of appeal is before an administrative law judge (ALJ). ...
What address do you send Medicare claims to?
Medicare All state claim address and phone number list, if any modification please comment it....Medicare claim address, phone numbers, payor id – revised list.StateArizonaIVR #1-877-908-8431Claim mailing addressMedicare Part B P.O. Box 6704 Fargo, ND 58108-6704Appeal addressMedicare Part B PO Box 6704 Fargo, ND 58108-6704Online resourcewww.noridianmedicare.com22 more columns
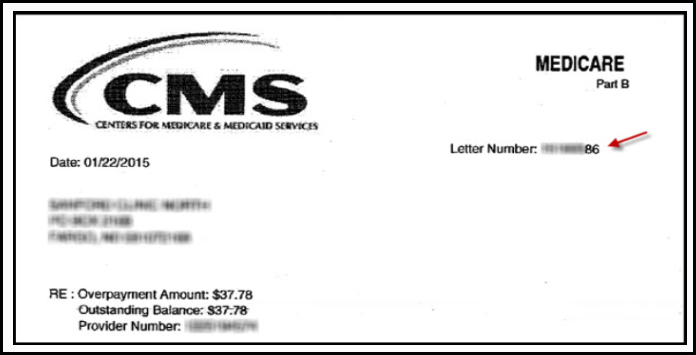
How do I dispute a Medicare charge?
Fill out a "Redetermination Request Form [PDF, 100 KB]" and send it to the company that handles claims for Medicare. Their address is listed in the "Appeals Information" section of the MSN. Or, send a written request to company that handles claims for Medicare to the address on the MSN.
How do I write a Medicare appeal letter?
The Medicare appeal letter format should include the beneficiary's name, their Medicare health insurance number, the claim number and specific item or service that is associated with the appeal, dates of service, name and location of the facility where the service was performed and the patient's signature.
Where do I mail Medicare Part B claims?
Medicare Claims Mailing Addressed for Mental Health Part B ClaimsNoridian Healthcare Solutions.P.O. Box 6703 Fargo, ND 58108-6703.
Can I appeal a Medicare decision?
The plan must tell you, in writing, how to appeal. After you file an appeal, the plan will review its decision. Then, if your plan doesn't decide in your favor, the appeal is reviewed by an independent organization that works for Medicare, not for the plan.
Who has the right to appeal denied Medicare claims?
You have the right to appeal any decision regarding your Medicare services. If Medicare does not pay for an item or service, or you do not receive an item or service you think you should, you can appeal. Ask your doctor or provider for a letter of support or related medical records that might help strengthen your case.
How do I write a letter of appeal for a denied claim?
Things to Include in Your Appeal LetterPatient name, policy number, and policy holder name.Accurate contact information for patient and policy holder.Date of denial letter, specifics on what was denied, and cited reason for denial.Doctor or medical provider's name and contact information.
How long does Medicare have to respond to an appeal?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days. Payment request—60 days.
How do I appeal insurance denial?
You or your doctor contact your insurance company and request that they reconsider the denial. Your doctor may also request to speak with the medical reviewer of the insurance plan as part of a “peer-to-peer insurance review” in order to challenge the decision.
Can you mail claims to Medicare?
4. Mail completed form and supporting documents to Medicare Submit your completed Patient's Request for Medical Payment form, itemized medical bill or bills, and any supporting documents to your state's Medicare contractor. All claims must be submitted by mail; you can't file a Medicare claim online.
What form is used to send claims to Medicare?
Form CMS-1500Providers sending professional and supplier claims to Medicare on paper must use Form CMS-1500 in a valid version. This form is maintained by the National Uniform Claim Committee (NUCC), an industry organization in which CMS participates.
How do I submit Medicare secondary claims?
Medicare Secondary Payer (MSP) claims can be submitted electronically to Novitas Solutions via your billing service/clearinghouse, directly through a Secure File Transfer Protocol (SFTP) connection, or via Novitasphere portal's batch claim submission.
How to contact Novitas for Medicare appeal?
If you have questions related to the first level of appeal / redetermination requests, please contact our Customer Service Center at 1-855-252-8782. Please use the following address and post office boxes to submit requests for claim redeterminations (first level appeals) to Novitas Solutions. Medicare Appeals.
What is the appeals process in Novitas?
The appeals process starts with Novitas Solutions at the first level of appeal / redetermination. If the appeals process continues to progress from one level to the next, questions regarding appeal status, other than a redetermination , should be directed to the party that is reviewing the documentation (depending on the level of appeal .)
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
What to do if you are not satisfied with the IRE decision?
If you’re not satisfied with the IRE’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or, in certain circumstances, a review of the appeal record by an ALJ or an attorney adjudicator.
What is a home health change of care notice?
The “Home Health Change of Care Notice” is a written notice that your home health agency should give you when your home health plan of care is changing because of one of these:
What is the ABN for Medicare?
If you have Original Medicare and your doctor, other health care provider, or supplier thinks that Medicare probably (or certainly) won’t pay for items or services, he or she may give you a written notice called an ABN (Form CMS-R-131).
How long does it take for an IRE to review a case?
They must get this information within 10 days after the date you get the notice telling you your case file has been sent to the IRE. The IRE’s address is on the notice.
Do doctors have to give advance notice of non-coverage?
Doctors, other health care providers, and suppliers don’t have to (but still may) give you an “Advance Beneficiary Notice of Noncoverage” for services that Medicare generally doesn’t cover, like:
How long does it take to appeal a Medicare payment?
The MSN contains information about your appeal rights. You'll get a MSN in the mail every 3 months, and you must file your appeal within 120 days of the date you get the MSN.
How long does it take for Medicare to make a decision?
You can submit additional information or evidence after the filing redetermination request, but, it may take longer than 60 days for the Medicare Administrator Contractor (MAC) that processes claims for Medicare to make a decision. If you submit additional information or evidence after filing, the MAC will get an extra 14 calendar days ...
How long does it take for Medicare to be reconsidered?
You'll generally get a decision from the MAC (either in a letter or an MSN) called a "Medicare Redetermination Notice" within 60 days after they get your request. If you disagree with this decision, you have 180 days after you get the notice to request a reconsideration by a Qualified Independent Contractor (QIC).
What to call if you don't file a Medicare claim?
If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227) . TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got. If it's close to the end of the time limit and your doctor or supplier still hasn't filed the claim, you should file the claim.
How to file a medical claim?
Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1 The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2 The itemized bill from your doctor, supplier, or other health care provider 3 A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare 4 Any supporting documents related to your claim
How long does it take for Medicare to pay?
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020.
When do you have to file Medicare claim for 2020?
For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020. Check the "Medicare Summary Notice" (MSN) you get in the mail every 3 months, or log into your secure Medicare account to make sure claims are being filed in a timely way.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. , these plans don’t have to file claims because Medicare pays these private insurance companies a set amount each month.
Do you have to file a claim with Medicare Advantage?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. , these plans don’t have to file claims because Medicare pays these private insurance companies a set amount each month.