What is the age to begin madicare or Medicaid?
While most beneficiaries are people aged 65 or older, others receive these services at a younger age due to a qualifying disability. Medicare is the U.S. national health insurance program for those 65 and older or with qualifying disabilities.
When can you start Medicaid?
You can apply for and enroll in Medicaid or CHIP anytime during the year. Learn how to use your Medicaid or CHIP coverage. Like Medicaid and CHIP, the Basic Health Program (BHP) offers affordable, continuous coverage. It’s an optional program that your state may offer.
What month and year did Medicaid start?
This act helped to add Section 1927 to the Social Security Act of 1935 and became effective on January 1, 1991. This program was formed due to the costs that Medicaid programs were paying for discount price outpatient drugs.
What is the age limit to receive Medicaid?
There is no universal age at which to qualify for Medicaid, and age may or may not factor into your eligibility at all depending on where you live. One type of Medicaid is the Aged, Blind and Disabled (ABD) Medicaid program.
Do I Automatically Get Medicare When I Turn 65?
Some people automatically get Medicare at age 65, but those numbers have declined as the Medicare and Social Security ages have continued to drift...
What if I’m Not Automatically Enrolled at 65?
If your Medicare enrollment at 65 is not automatic, but you want to enroll, here are some more magic numbers.
Is Medicare Free at Age 65?
While Medicare Part B has a standard monthly premium, 99 out of 100 people don’t have to pay a premium for Medicare Part A. Still, no part of Medic...
How Much Does Medicare Cost at Age 65?
The standard premium for Part B modestly increases year over year. Part A costs also can increase, including the annual deductible and other coinsu...
Can You Get on Medicare at Age 62?
No, but while the standard age of eligibility remains 65, some call for lowering it. In a recent GoHealth survey, among respondents age 55 and olde...
Can a 55-Year-Old Get Medicare?
While 65 has always been Medicare’s magic number, there are a few situations where the Medicare age limit doesn’t apply, and you may be able to get...
What is the age limit for Medicare?
Most older adults are familiar with Medicare and its eligibility age of 65. Medicare Part A and Medicare Part B are available based on age or, in some cases, health conditions, including:
When do you get Medicare?
Some people automatically get Medicare at age 65, but those numbers have declined as the Medicare and Social Security ages have continued to drift apart.
Why do people not get Medicare at 65?
These days, fewer people are automatically enrolled in Medicare at age 65 because they draw Social Security benefits after 65. If you do not receive Social Security benefits, you will not auto-enroll in Medicare.
How long do you have to be on Social Security to get Medicare?
Individuals under 65 and already receiving Social Security or Railroad Retirement Board benefits for 24 months are eligible for Medicare. Still, most beneficiaries enroll at 65 when they become eligible for Medicare.
When did Medicare become law?
In the summer of ‘65, President Lyndon Johnson signed Medicare into law, establishing the age of eligibility at 65. The eligibility age for Medicare remains the same to this day.
How old do you have to be to get medicare?
While some specific circumstances can impact at what age you are eligible for Medicare, most people must wait until 65 as things currently stand.
When will Social Security be 67?
In 2000, the Social Security Amendments of 1983 began pushing back the standard age for full Social Security benefits. The progressive changes are nearing their conclusion: Beginning in 2022, the standard age for full benefits will be 67 for anyone born after 1960.
How old do you have to be to get Medicare?
Medicare eligibility at age 65. You must typically meet two requirements to receive Medicare benefits: You are at least 65 years old. You are a U.S. citizen or a legal resident for at least five years. In order to receive premium-free Part A of Medicare, you must meet both of the above requirements and qualify for full Social Security ...
How long do you have to be a resident to qualify for Medicare?
Medicare eligibility chart - by age. - Typically eligible for Medicare if you're a U.S. citizen or legal resident for at least 5 years. - If you won't be automatically enrolled when you turn 65, your Initial Enrollment Period begins 3 months before your 65th birthday.
How much is Medicare Part A 2020?
In 2020, the Medicare Part A premium can be as high as $458 per month. Let’s say Gerald’s wife, Jessica, reaches age 62 and has worked for the required number of years to qualify for premium-free Part A once she turns 65. Because Jessica is now 62 years old and has met the working requirement, Gerald may now receive premium-free Part A.
What is the Social Security retirement rate at 65?
Your Social Security retirement benefits will be reduced to 93.3% if you take them at age 65. - Not typically eligible for Medicare, unless you receive SSA or RRB disability benefits or have ALS or ESRD.
Can a 65 year old spouse get Medicare?
When one spouse in a couple turns 62 years old, the other spouse who is at least 65 years old may now qualify for premium-free Medicare Part A if they haven’t yet qualified based on their own work history. For example, Gerald is 65 years old, but he doesn’t qualify for premium-free Part A because he did not work the minimum number ...
Who can help you compare Medicare Advantage plans?
If you have further questions about Medicare eligibility, contact a licensed insurance agent today. A licensed agent can help answer your questions and help you compare Medicare Advantage plans (Medicare Part C) that are available where you live.
Is Medicaid based on income?
Yes. Medicaid qualification is based on income, not age. While Medicaid eligibility differs from one state to another, it is typically available to people of lower incomes and resources including pregnant women, the disabled, the elderly and children. Learn more about the difference between Medicare and Medicaid.
When did Medicaid become law?
Medicaid was signed into law in 1965 alongside Medicare and is offered in all 50 states, the District of Columbia and U.S. territories.
What is EPSDT in Medicaid?
Another type of Medicaid program is Early and Periodic Screening, Diagnostic, and Treatment (EPSDT). This program is available to individuals under the age of 21 who live in households that meet certain financial criteria. This type of Medicaid also has an age restriction and could therefore also be considered age-based.
Does age play a role in Medicaid eligibility?
Age may or may not play a factor in Medicaid eligibility, as there are different types of Medicaid programs, various ways to qualify and rules that differ by state. In this Medicaid eligibility guide, we’ll break down the role that age plays in Medicaid eligibility, enrollment and benefits.
Does Medicare require an age?
Each state governs its own Medicare program in adherence to federal regulations. Some states may have an age requirement in order to qualify for its Medicaid program while other states may not.
Is Medicaid available in North Dakota?
But in North Dakota, Medicaid is available to all low-income adults, regardless of age.
Is Medicaid a non-citizen?
Medicaid qualification is different in every state. You must be a resident of the state in which you are applying for benefits and must be a U.S. citizen or otherwise qualified non-citizen such as a lawful permanent resident.
Is there an age limit for medicaid?
There is no universal age at which to qualify for Medicaid, and age may or may not factor into your eligibility at all depending on where you live.
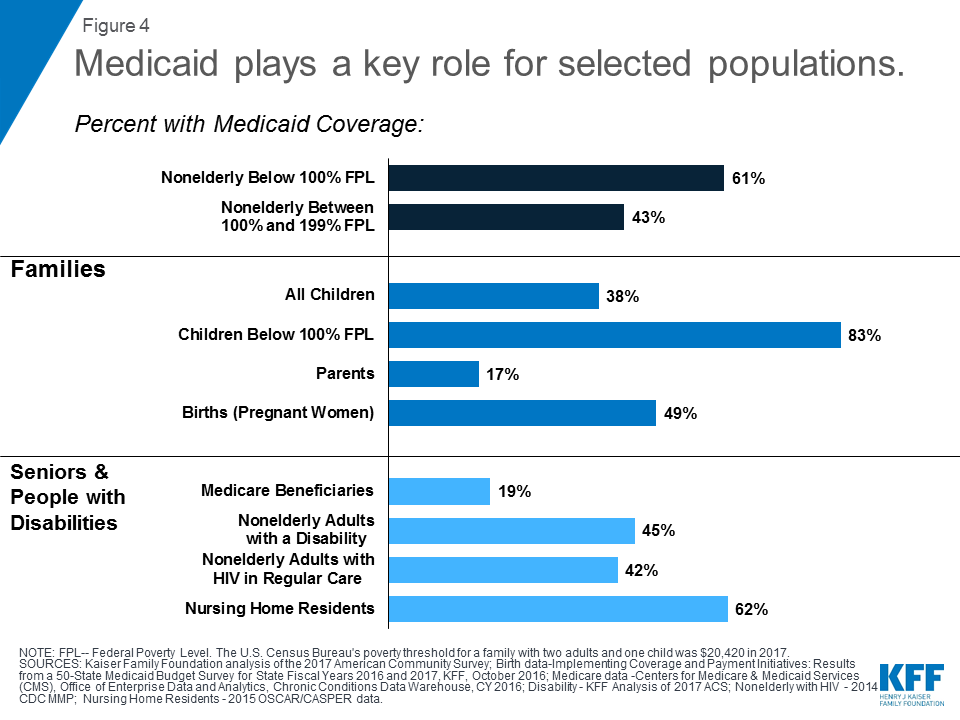
What is the Medicaid age limit?
The Affordable Care Act of 2010 created the opportunity for states to expand Medicaid to cover nearly all low-income Americans under age 65 . Eligibility for children was extended to at least 133% of the federal poverty level (FPL) in every state (most states cover children to higher income levels), and states were given the option to extend eligibility to adults with income at or below 133% of the FPL. Most states have chosen to expand coverage to adults, and those that have not yet expanded may choose to do so at any time. See if your state has expanded Medicaid coverage to low-income adults.
How long does medicaid last?
Benefits also may be covered retroactively for up to three months prior to the month of application, if the individual would have been eligible during that period had he or she applied. Coverage generally stops at the end of the month in which a person no longer meets the requirements for eligibility.
What is dual eligible for Medicare?
Eligibility for the Medicare Savings Programs, through which Medicaid pays Medicare premiums, deductibles, and/or coinsurance costs for beneficiaries eligible for both programs (often referred to as dual eligibles) is determined using SSI methodologies..
What is MAGI for Medicaid?
MAGI is the basis for determining Medicaid income eligibility for most children, pregnant women, parents, and adults. The MAGI-based methodology considers taxable income and tax filing relationships to determine financial eligibility for Medicaid. MAGI replaced the former process for calculating Medicaid eligibility, ...
What is Medicaid coverage?
Medicaid is the single largest source of health coverage in the United States. To participate in Medicaid, federal law requires states to cover certain groups of individuals. Low-income families, qualified pregnant women and children, and individuals receiving Supplemental Security Income (SSI) are examples of mandatory eligibility groups (PDF, ...
How many people are covered by medicaid?
Medicaid is a joint federal and state program that, together with the Children’s Health Insurance Program (CHIP), provides health coverage to over 72.5 million Americans, including children, pregnant women, parents, seniors, and individuals with disabilities. Medicaid is the single largest source of health coverage in the United States.
Does Medicaid require income?
Certain Medicaid eligibility groups do not require a determination of income by the Medicaid agency. This coverage may be based on enrollment in another program, such as SSI or the breast and cervical cancer treatment and prevention program.
When does Medicare start?
Medicare coverage can start as early as the first day of the month in which you turn 65, unless you were born on the first of the month. In that case, your coverage can begin on the first day of the previous month. People who are automatically enrolled will get coverage as soon as it’s available.
When is open enrollment for Medicare?
Open enrollment periods. During fall open enrollment from Oct. 15 to Dec. 7, you can make certain changes to your coverage, such as switching from Original Medicare to a Medicare Advantage Plan. You can also enroll in Part D if you didn’t do so earlier, although penalties may apply. The changes take effect Jan. 1.
How long does it take to get Medicare if you have ALS?
People who get disability benefits from Social Security automatically receive Medicare coverage after 24 months. People who have ALS, also known as Lou Gehrig’s disease, automatically receive Medicare coverage the same month that disability benefits start.
Can you qualify for special enrollment period?
Special enrollment periods. You can qualify for special enrollment period and avoid penalties in a few circumstances, such as when you’re covered by a group health insurance plan from a current employer — either your own or your spouse’s.
Does Medicare cover ALS?
People who have ALS, also known as Lou Gehrig’s disease, automatically receive Medicare coverage the same month that disability benefits start.
Does Medicare cover people under 65?
Medicare also covers certain people under 65 who have disabilities. Here’s when their Medicare coverage starts:
How long do you have to wait to receive Medicare?
To receive Medicare disability benefits, you must first receive Social Security Disability Insurance (SSDI) benefits for 24 months. 11 There is usually a five-month waiting period after a worker or widow (er) is labeled as disabled before they can receive SSDI benefits. 12 During this waiting period, the individual may be eligible for coverage under an employer’s health plan or, if they’re no longer employed, through COBRA .
What is Medicare for 65?
Medicare is the U.S. national health insurance program for those 65 and older or with qualifying disabilities.
How long does it take to get a disability if you have Lou Gehrig's disease?
If a person has end-stage renal disease (ESRD) or amyotrophic lateral sclerosis (ALS), which is more commonly known as Lou Gehrig’s disease, there is no 24-month waiting period for benefits. 13 A person diagnosed with ESRD can generally begin receiving benefits three months after a course of regular dialysis or after a kidney transplant. 14 Meanwhile, as soon as a person diagnosed with ALS begins collecting Social Security Disability benefits, they are enrolled in Part A and Part B Medicare benefits. 15
How does Medicare work?
Like Social Security, Medicare is a U.S. government program funded by tax withholding from most workers' paychecks. When they reach 65 or meet other eligibility requirements, they receive Medicare services. 2 You will probably receive Medicare Part A coverage free of charge because of your payroll deductions, but Medicare has other aspects that will likely cost you. 3
Who can talk to about Medicare?
This could be your Human Resources department or a Medicare representative.
Can a stay at home parent get Medicare?
Stay-at-home parents with no work history may still be eligible for Medicare benefits depending on their spouse's work history.
Is Medicare for people who are 65?
You might be eligible right now and not know it. Our research has found that while more than 80% of beneficiaries are people aged 65 or older, others receive services at a younger age due to a qualifying disability. 1
What is the eligibility age for Medicare?
What is the Medicare eligibility age? The eligibility age for Medicare is 65 years old for most people. This applies whether or not you’re still working at the time of your 65th birthday. The age when you retire does not factor into Medicare eligibility.
What age do you have to be to qualify for Medicare?
Medicare eligibility requirements. To qualify for Medicare under any circumstances, including reaching age 65 and those outlined above, you’ll need to meet the following eligibility requirements: U.S. citizenship. You must be a citizen, or you must have been a legal resident for a minimum of 5 years. Address. You must have a stable U.S. address.
How long do you have to be on Medicare to get Social Security?
Social Security disability. If you’re under age 65 and have been receiving Social Security disability benefits for 24 months, you qualify for Medicare. You can enroll in your 22nd month of receiving these benefits, and your coverage will begin in your 25th month of receiving them. If you’re entitled to monthly benefits based on an occupational ...
Is Medicare considered secondary insurance?
If you have insurance through your employer when you apply for Medicare, it will remain your primary insurance and Medicare will be considered secondary insurance.
Does the correctional system pay for Medicare?
If you’re imprisoned, generally the correctional facility will provide and pay for your care, not Medicare.
Can I get Medicare if I have ALS?
If you’ve been diagnosed with ALS, also known as Lou Gehrig’s Disease, you become immediately eligible for Medicare upon collecting Social Security disability insurance (SSDI) benefits.
When does Medicare start?
For most people, Medicare coverage starts the first day of the month you turn 65. Some people delay enrollment and remain on an employer plan. Others may take premium-free Part A and delay Part B. If someone is on Social Security Disability for 24 months, they qualify for Medicare. Those with End-Stage Renal Disease will be immediately eligiblee ...
How long do you have to wait to apply for medicare?
You should start looking into and applying for Medicare for up to 6 months before you become eligible.
What is a Medigap plan?
Medigap is extra insurance that fills in the gaps in Medicare. Medigap plans can pay for more extended hospital stays. Your one-time Medigap Open Enrollment Period starts on the 1st day of the month you’re 65 years old and have Part B.
What happens if you sign up for Medigap?
Signing up for Medigap during Open Enrollment means the insurance company CAN’T charge you more or deny you coverage. If you wait and sign up, you can be turned down or charged more because of your health.
How old do you have to be to collect retirement?
Some people wait until they retire to start collecting benefits. For some, that could be 66 years old; for others, waiting until 70 to get delayed retirement credits may be the most beneficial retirement plan.
When do you sign up for unemployment benefits?
It includes your birth month, and it ends three months after your birth month. If you want your benefits to start at the beginning of the month, you turn 65, be sure to sign up at least a month before your birthday. ...
Can you get Medicare if you have ALS?
Those with End-Stage Renal Disease will be immediately eligiblee for Medicare with a diagnosis. When Medicare starts is different for each beneficiary. People with disabilities, ALS, or End-Stage Renal Disease may be eligible for Medicare before they’re 65. If you qualify for Medicare because of a disability, there is no minimum age ...
What is Medicare and Medicaid?
Medicaid, a combined state and federal program, is a state-specific health insurance program for low-income individuals with limited financial means, regardless of their age.
What is Medicare Part B?
Medicare Part B is for outpatient care, durable medical equipment, and home health care. Part D is for prescription coverage. Not all persons will elect to have coverage in all three areas. In addition, some persons choose to get their Medicare benefits via Medicare Advantage plans, also called Medicare Part C.
What is spend down Medicaid?
Some depending on program / waiver. *Some states have “ spend-down ” Medicaid in which income limits are considered relative to medical bills and care costs. This is also referred to as the medically needy pathway to eligibility. **Varies dramatically by state, and not all eligibility groups have an asset limit.
Does Medicaid cover nursing home care?
Medicaid, being state run, has different benefits in each state. Generally speaking, Medicaid pays for nursing home care. Through home and community based services waiver programs it may also pay for: To avoid confusion, it is worth noting that Medicaid is referred to by different names in different states.
Does Medicare pay for long term care?
In the context of long term care for the elderly, Medicare’s benefits are very limited. Medicare does not pay for personal care (also known as custodial care or non-medical care). Medicare will pay for a very limited number of days (no more than 100 days following hospitalization for a minimum of 3 days) of skilled nursing (also referred to as nursing home care). Medicare will also pay for some home health care, provided it is medical in nature. Starting in 2019, some Medicare Advantage plans started offering long term care benefits. These services and supports are plan specific. But they may include:
Is Medicaid more comprehensive?
Medicaid is more comprehensive in its coverage, but the benefits are specific to the age group. Children have different eligibility requirements and receive different benefits from low-income adults and from elderly or disabled persons.
Is Medicare and Medicaid mutually exclusive?
Yes, Medicare and Medicaid are not mutually exclusive programs. Persons who are eligible for both are referred to as having Dual Eligibility, Dual Eligibles, or often simply “Duals”. Medicare is the first payer of covered benefits, while Medicaid is the secondary payer. Typically, Medicaid will pay for Medicare premiums and co-payments for dual eligibles. In fact, many states have special programs intended to make it easier for seniors to manage their dual eligibility status as it can be confusing to know where to turn for what services. This is generally in the form of managed care.
