Does Medicare cover the cost of in home health care?
The only way Medicare will cover your home health costs is if you receive your care from a Medicare-approved home health agency. Your doctor may have recommendations for agencies that are Medicare-approved that he or she trusts with their patients.
How much does Medicare pay for in home care?
Medicare will cover 100% of the costs for medically necessary home health care provided for less than eight hours a day and a total of 28 hours per week. The average cost of home health care as of 2019 was $21 per hour. Many seniors opt for home health care if they require some support but do not want to move into an assisted living community.
Does Medicare or Medicaid pay for home care?
Does Medicare pay for any home care? It is very rare for Medicare to pay for any home-based services, particularly personal or “custodial” care. The general exception to this rule is if such care falls under the description of doctor-prescribed medically necessary treatment for illness, injury, or condition, including:
What are the Medicare requirements for home health care?
cover eligible home health services like these:
- Part-Time Or "Intermittent" Skilled Nursing Care Part-time or intermittent nursing care is skilled nursing care you need or get less than 7 days each week or less than 8 hours ...
- Physical therapy
- Occupational therapy
- Speech-language pathology services
- Medical social services
- Part-time or intermittent home health aide services (personal hands-on care)

How many days will Medicare pay 100% of the covered costs of care in a skilled nursing care facility?
100 daysMedicare covers care in a SNF up to 100 days in a benefit period if you continue to meet Medicare's requirements.
Does Medicare pay for home assistant?
Home health aide: Medicare pays in full for an aide if you require skilled care (skilled nursing or therapy services). A home health aide provides personal care services, including help with bathing, toileting, and dressing.
How Much Does Medicare pay for home health care per hour?
Medicare will cover 100% of the costs for medically necessary home health care provided for less than eight hours a day and a total of 28 hours per week. The average cost of home health care as of 2019 was $21 per hour.
What will Medicare not pay for?
Generally, Original Medicare does not cover dental work and routine vision or hearing care. Original Medicare won't pay for routine dental care, visits, cleanings, fillings dentures or most tooth extractions. The same holds true for routine vision checks. Eyeglasses and contact lenses aren't generally covered.
Medicare Covers Medically Necessary Home Health Services
Medicare does not usually cover the cost of non-medical home care aides if that is the only type of assistance that a senior needs.
Medicare Advantage May Offer More Comprehensive Coverage
Private insurance companies run Medicare Advantage. Those companies are regulated by Medicare and must provide the same basic level of coverage as Original Medicare. However, they also offer additional coverage known as “supplemental health care benefits.”
What is home health care?
Home health care covers a wide range of treatment options that are performed by medical professionals at home. Care may include injections, tube feedings, condition observation, catheter changing, and wound care. Skilled therapy services are also included in home health care, and these include occupational, speech, ...
What percentage of Medicare Part B is DME?
Medicare Part B will cover 80 percent of the Medicare-approved amount for DME as long as the equipment is ordered by your physician and you rent or purchase the devices through a supplier that is participating in Medicare and accepts assignment.
How often do you need to be a skilled nursing nurse?
Treatments must be needed part time, at least once every 60 days, but not more than once daily for up to three weeks. You must be under the care of a physician.
Does Medicare cover speech therapy?
Medical social services may also be covered under your Medicare benefits.
Is home health care a good idea?
Home health care can be a good solution for those patients who need care for recovery after an injury, monitoring after a serious illness or health complication, or medical care for other acute health issues. Medicare recipients may get help paying for home health care if you meet specific criteria.
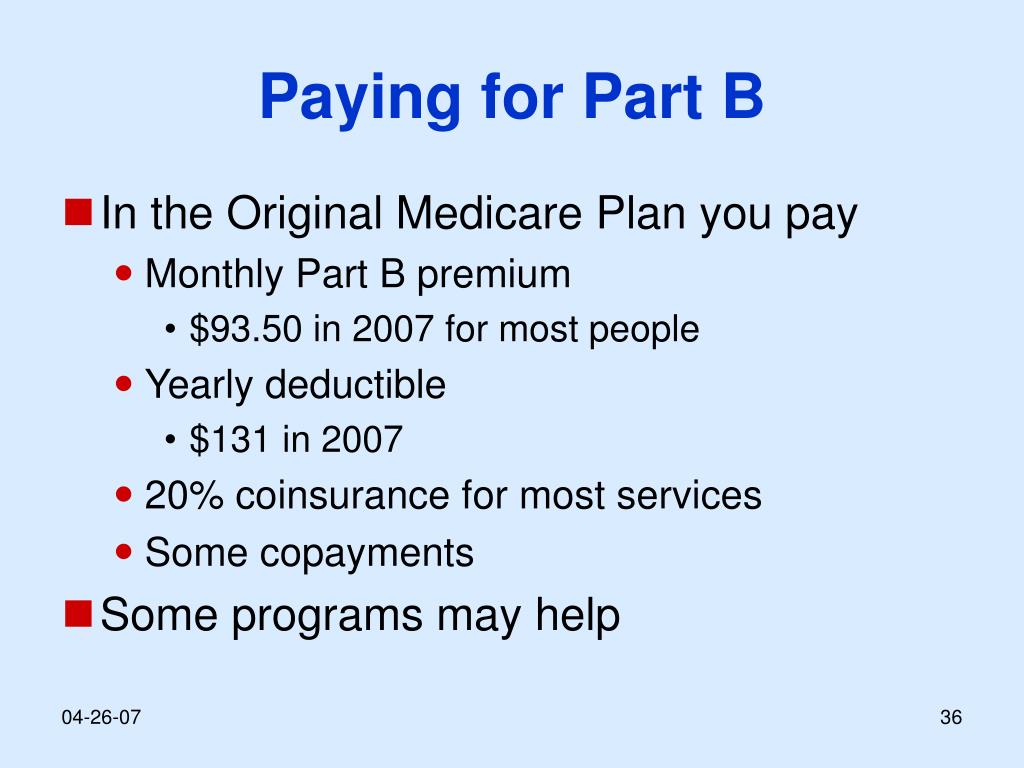
Do you have to pay 20 percent of Medicare deductible?
You will be required to pay 20 percent out of pocket, and the part B deductible may apply. If you are enrolled in a Medicare Advantage (MA) plan, you will have the same benefits as Original Medicare Part A and Part B, but many MA plans offer additional coverage. Related articles:
Does Medicare pay for home health?
If you do qualify for home health care, Medicare Part A and Part B may help cover the costs associated with your care. You will pay $0 for home health care services. If you require durable medical equipment, or DME, Medicare benefits will help pay for equipment you may need, including items that are designed for medical use in ...
Will Medicare Pay for Home Health Care Costs?
Medicare will pay for home health care costs if you meet all criteria for participation. Original Medicare allows you to go to any home health care agency that is a Medicare contracted provider. The agency should also tell you if Medicare doesn’t cover any items or services and how much you'll have to pay.
What Home Health Care Services Will Medicare Cover?
Medicare will cover a wide range of healthcare services under the home health care benefit, but you may not need all of them depending on the condition that qualified you to begin with. However, you have to have some need for professional services to be eligible for home health care services.
What Home Health Care Services Will Medicare NOT Cover?
There are services Medicare will not pay for, which may come as a surprise to some families. If your loved one needs some of the care that Medicare will not cover, you will need to consider family caregiving or private-pay caregivers. Medicare will not cover the following under the home health care benefit:
How Do You Qualify for Home Health Care Coverage?
For Medicare to qualify you for home health coverage, you must meet specific criteria. If you’re in doubt about qualifying, contact your physician first to tell you whether they are willing to write an order for services.
How Do You Get Medicare to Pay for These Costs?
As the recipient of home health services with a Medicare provider, you would not typically need to get Medicare to pay for costs. Medicare pays your Medicare-certified home health agency for the covered services you get during a 30-day period of care.
Medicare Payment for Home Health Care Costs
Although it’s a beneficial healthcare program, Medicare can be complicated to understand. Benefits through medicare are numerous but require an understanding of the criteria for participation. This is especially true of Medicare Advantage plans. Home healthcare costs are covered under Medicare if you follow the rules for participation.
How do I contact Medicare for home health?
If you have questions about your Medicare home health care benefits or coverage and you have Original Medicare, visit Medicare.gov, or call 1-800-MEDICARE (1-800-633-4227) . TTY users can call 1-877-486-2048. If you get your Medicare benefits through a Medicare Advantage Plan (Part C) or other
What happens when home health services end?
When all of your covered home health services are ending, you may have the right to a fast appeal if you think these services are ending too soon. During a fast appeal, an independent reviewer called a Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) looks at your case and decides if you need your home health services to continue.
What is an appeal in Medicare?
Appeal—An appeal is the action you can take if you disagree with a coverage or payment decision made by Medicare, your Medicare health plan, or your Medicare Prescription Drug Plan. You can appeal if Medicare or your plan denies one of these:
Why is home health important?
In general, the goal of home health care is to provide treatment for an illness or injury. Where possible, home health care helps you get better, regain your independence, and become as self-sucient as possible. Home health care may also help you maintain your current condition or level of function, or to slow decline.
Can Medicare take home health?
In general, most Medicare-certified home health agencies will accept all people with Medicare . An agency isn’t required to accept you if it can’t meet your medical needs. An agency shouldn’t refuse to take you because of your condition, unless the agency would also refuse to take other people with the same condition.
Who can get home health care with Medicare?
Lorraine Roberte is an insurance writer for The Balance. As a personal finance writer, her expertise includes money management and insurance-related topics. She has written hundreds of reviews of insurance products.
Who Qualifies for Home Health Care With Medicare?
Medicare has several conditions in place for home health care. Anyone with Part A or Part B coverage who meets all of these qualifying factors is eligible:
What Home Health Services Does Medicare Cover?
Medicare covers specific types of home health care services, including:
Expanded Home Health Care Coverage
If you’re looking for additional coverage for home health care beyond what Medicare includes, you do have some options. These can help you save money on home health care.
The Bottom Line
Medicare does cover some home health care. However, there are strict conditions you must meet to qualify. In addition, the services are often limited in scope and duration.
How long does Medicare pay for home health care services?
Medicare typically pays for home health care services considered “intermittent” for up to 21 days. However, extensions are sometimes granted if the doctor has an estimated time when you’d no longer need the care. 3
How many hours of home health care does Medicare cover?
Medicare covers intermittent home health care. This is defined as care that’s needed fewer than seven days a week for fewer than eight hours a day. Additionally, intermittent home health care is not meant to exceed 21 days. 3
How to qualify for home health care?
Ideally, home health can enhance your care and prevent re-admission to a hospital. There are several steps and conditions to qualify for home health care: 1 You must be under the care of a doctor who has created a plan for you that involves home health care. Your doctor must review the plan at regular intervals to make sure it is still helping you. 2 Your doctor must certify that you need skilled nursing care and therapy services. To need this care, your doctor must decide that your condition will improve or maintain through home health services. 3 Your doctor must certify that you are homebound. This means it is very difficult or medically challenging for you to leave your home.
What is home health aide?
Home health aides are health professionals who help people in their home when they have disabilities, chronic illnesses, or need extra help. Aides may help with activities of daily living, such as bathing, dressing, going to the bathroom, or other around-the-home activities. For those who need assistance at home, home health aides can be invaluable.
What is the difference between home health and skilled nursing?
The difference is that, for reimbursement, you must be getting skilled nursing services as well.
What is Medicare Part A?
Medicare Part A is the portion that provides hospital coverage. Medicare Part A is free to most individuals when they or their spouse worked for at least 40 quarters paying Medicare taxes.
What education do you need to be a home health aide?
According to the U.S. Bureau of Labor Statistics, the typical educational level for a home health aide is a high school diploma or equivalent. Some people may use the term “home health aide” to describe all occupations that provide care at home, but a home health aide is technically different from a home health nurse or therapist.
Who must review home health care plans?
You must be under the care of a doctor who has created a plan for you that involves home health care. Your doctor must review the plan at regular intervals to make sure it is still helping you. Your doctor must certify that you need skilled nursing care and therapy services.
Is long term care insurance part of Medicare?
Some people choose to purchase separate long-term care insurance, which isn’t a part of Medicare . These policies may help to cover more home health care services and for longer time periods than Medicare. However, the policies vary and do represent an extra cost to seniors.
When will HHAs get paid?
30-Day Periods of Care under the PDGM. Beginning on January 1 2020, HHAs are paid a national, standardized 30-day period payment rate if a period of care meets a certain threshold of home health visits. This payment rate is adjusted for case-mix and geographic differences in wages. 30-day periods of care that do not meet ...
What is PPS in home health?
The Balanced Budget Act (BBA) of 1997, as amended by the Omnibus Consolidated and Emergency Supplemental Appropriations Act (OCESAA) of 1999, called for the development and implementation of a prospective payment system (PPS) for Medicare home health services.
When did the Home Health PPS rule become effective?
Effective October 1, 2000, the home health PPS (HH PPS) replaced the IPS for all home health agencies (HHAs). The PPS proposed rule was published on October 28, 1999, with a 60-day public comment period, and the final rule was published on July 3, 2000. Beginning in October 2000, HHAs were paid under the HH PPS for 60-day episodes ...
Is telecommunications technology included in a home health plan?
In response CMS amended § 409.43 (a), allowing the use of telecommunications technology to be included as part of the home health plan of care, as long as the use of such technology does not substitute for an in-person visit ordered on the plan of care.