In 2022, the federal government is projected to spend $316 billion on support for employment-based coverage for people under age 65 and $462 billion for Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
How much does the federal government spend on Medicaid each year?
The Federal share of all Medicaid expenditures is estimated to have been 63 percent in 2018. State Medicaid expenditures are estimated to have decreased 0.1 percent to $229.6 billion. From 2018 to 2027, expenditures are projected to increase at an average annual rate of 5.3 percent and to reach $1,007.9 billion by 2027.
How has the enhanced FMAP impacted Medicaid spending growth?
While the enhanced FMAP shifts some state spending on this increased enrollment to the federal government, the sustained federal outlay growth in the quarters after the FMAP increase first took effect likely reflects overall Medicaid spending growth that is experienced at the state-level as well as the federal level.
What is a Medicare-Medicaid plan?
Medicare-Medicaid Plans. Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
How many people are enrolled in Medicaid in the US?
64,699,741 individuals were enrolled in Medicaid. 6,695,724 individuals were enrolled in CHIP. Medicaid expenditures are estimated to have increased 2.7 percent to $616.1 billion in 2018, with Federal expenditures having grown an estimated 4.4 percent to $386.5 billion.

What is the federal budget for Medicare?
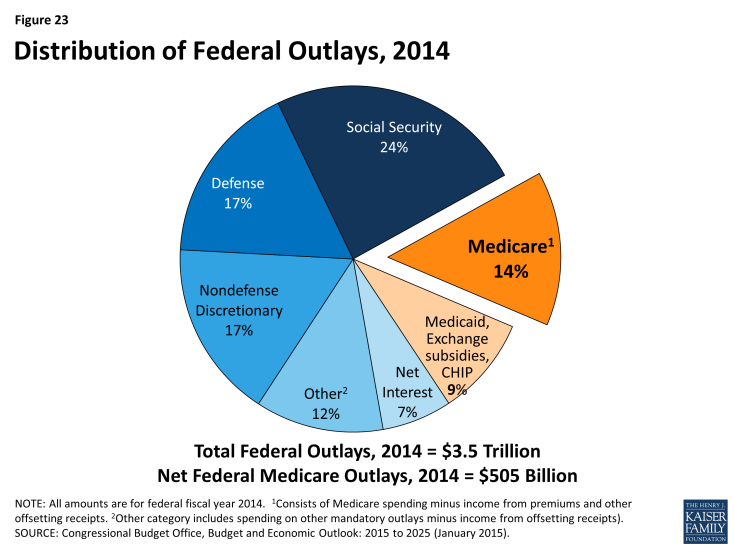
Medicare accounts for a significant portion of federal spending. In fiscal year 2020, the Medicare program cost $776 billion — about 12 percent of total federal government spending. Medicare was the second largest program in the federal budget last year, after Social Security.
Does the federal government provide 56 cents for every Medicaid dollar spent?
individual states design and administer the medicaid programs (typically through the states department of public welfare) under broad guidelines established by the federal government. the federal government provides about 56 cents for every medicaid dollar spent, and the states provide the balance.
What are the major sources of funding for Medicare?
Funding for Medicare, which totaled $888 billion in 2021, comes primarily from general revenues, payroll tax revenues, and premiums paid by beneficiaries (Figure 1). Other sources include taxes on Social Security benefits, payments from states, and interest.
What is the role of the federal government in Medicare?
In the Medicare program, the federal government has taken some steps consistent with its purchaser role by facilitating disclosure of comparative quality data in the public domain. In 1998, the National Medicare Education Program—an initiative to educate beneficiaries about Medicare health care options—was launched.
What impact did the creation of the federal Medicaid program have on federal grants in aid?
Medicaid spending increases are the main driver of this upward trend. Spending for health care has driven the increase in federal grants to states over the past decade. Health grants grew by 73 percent from 2008 to 2019, while nonhealth grants decreased by 5 percent over that span. (See Figure 2.)
Which is considered a mandatory medical service that states must offer to receive federal matching funds?
Federal rules require state Medicaid programs to cover certain “mandatory” services, such as hospital and physician care, laboratory and X-ray services, home health services, and nursing facility services for adults.
Is Medicare subsidized by the federal government?
As a federal program, Medicare relies on the federal government for nearly all of its funding. Medicaid is a joint state and federal program that provides health care coverage to beneficiaries with very low incomes.
Who pays for Medicaid?
The Medicaid program is jointly funded by the federal government and states. The federal government pays states for a specified percentage of program expenditures, called the Federal Medical Assistance Percentage (FMAP).
How is Medicare funded now?
Medicare is funded by the Social Security Administration. Which means it's funded by taxpayers: We all pay 1.45% of our earnings into FICA - Federal Insurance Contributions Act, if you're into deciphering acronyms - which go toward Medicare. Employers pay another 1.45%, bringing the total to 2.9%.
How does federalism work in healthcare?
The federal government provides: Protections for people with preexisting health conditions. Uniform financial assistance for people with incomes below 400 percent of the federal poverty level. Individual and employer mandates to ensure people gain and keep coverage.
What is the function of the Center for Medicare and Medicaid services?
The Centers for Medicare and Medicaid Services (CMS) provides health coverage to more than 100 million people through Medicare, Medicaid, the Children's Health Insurance Program, and the Health Insurance Marketplace.
What is the federal Medicaid share?
The Federal share of all Medicaid expenditures is estimated to have been 63 percent in 2018. State Medicaid expenditures are estimated to have decreased 0.1 percent to $229.6 billion. From 2018 to 2027, expenditures are projected to increase at an average annual rate of 5.3 percent and to reach $1,007.9 billion by 2027.
What percentage of births were covered by Medicaid in 2018?
Other key facts. Medicaid Covered Births: Medicaid was the source of payment for 42.3% of all 2018 births.[12] Long term support services: Medicaid is the primary payer for long-term services and supports.
What percentage of Medicaid beneficiaries are obese?
38% of Medicaid and CHIP beneficiaries were obese (BMI 30 or higher), compared with 48% on Medicare, 29% on private insurance and 32% who were uninsured. 28% of Medicaid and CHIP beneficiaries were current smokers compared with 30% on Medicare, 11% on private insurance and 25% who were uninsured.
Which states have Medicaid expansion?
Two states (Maine and Virginia) implemented Medicaid expansion under the ACA in January 2019 and two others states (Idaho and Utah) implemented the expansion in January 2020. These expansions may contribute to higher federal Medicaid outlays in the quarter that expansion was implemented.
What does the enhanced FMAP shifts state spending on?
While the enhanced FMAP shifts some state spending on this increased enrollment to the federal government, the sustained federal outlay growth in the quarters after the FMAP increase first took effect likely reflects overall Medicaid spending growth that is experienced at the state-level as well as the federal level.
How much was the FFY 2020?
After the onset of the COVID-10 pandemic and the passage of the FFCRA in March 2020, quarterly outlays in Quarter 3 of FFY 2020 (April through June 2020) were $127.4 billion, an increase of 22.5% over Quarter 3 outlays in the prior year.
When will the FMAP increase end?
States could draw down the increased federal matching funds beginning at the end of March for claims paid in the first quarter of 2020 and in early April for the second quarter of 2020. 3 The FMAP increase will expire at the end of the quarter in which the public health emergency (PHE). In the one year since the onset of the coronavirus pandemic, ...
What is the Bureau of Fiscal Service?
The Bureau of the Fiscal Service (part of the U.S. Department of the Treasury) publishes these Monthly Treasury Statements, which summarize the financial activities of the U.S. federal government including receipts and outlays of funds. Specifically, this data note analyzes the Treasury data on outlays of the federal government classified as ...
Does the FMAP affect Medicaid?
The duration of federal fiscal relief to state Medicaid programs during the pandemic, which will affect both state and federal Medicaid spending in the future. The enhanced FMAP provides federal fiscal relief that helps replace state spending, so federal Medicaid spending growth may continue to outpace state spending growth while ...
Is Medicaid a countercyclical program?
The pandemic has generated both a public health crisis and an economic crisis, with major implications for Medicaid, a countercyclical program.
Which pays first, Medicare or Medicaid?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second.
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. . If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare.
Can you get medicaid if you have too much income?
Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid. The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid. In this case, you're eligible for Medicaid because you're considered "medically needy."
Can you spend down on medicaid?
Medicaid spenddown. Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid . The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid.
Does Medicare cover prescription drugs?
. Medicaid may still cover some drugs and other care that Medicare doesn’t cover.
What is the IFC for Medicare?
This interim final rule with comment period (IFC) gives individuals and entities that provide services to Medicare beneficiaries needed flexibilities to respond effectively to the serious public health threats posed by the spread of the 2019 Novel Coronavirus (COVID-19). Recognizing the urgency of this situation, and understanding that some pre-existing Medicare payment rules may inhibit innovative uses of technology and capacity that might otherwise be effective in the efforts to mitigate the impact of the pandemic on Medicare beneficiaries and the American public, we are changing Medicare payment rules during the Public Health Emergency (PHE) for the COVID-19 pandemic so that physicians and other practitioners, home health and hospice providers, inpatient rehabilitation facilities, rural health clinics (RHCs), and federally qualified health centers (FQHCs) are allowed broad flexibilities to furnish services using remote communications technology to avoid exposure risks to health care providers, patients, and the community. We are also altering the applicable payment policies to provide specimen collection fees for independent laboratories collecting specimens from beneficiaries who are homebound or inpatients (not in a hospital) for COVID-19 testing. We are also expanding, on an interim basis, the list of destinations for which Medicare covers ambulance transports under Medicare Part B. In addition, we are making programmatic changes to the Medicare Diabetes Prevention Program (MDPP) and the Comprehensive Care for Joint Replacement (CJR) Model in light of the PHE, and program-specific requirements for the Quality Payment Program to avoid inadvertently creating incentives to place cost considerations above patient safety. This IFC will modify the calculation of the 2021 and 2022 Part C and D Star Ratings to address the expected disruption to data collection and measure scores posed by the COVID-19 pandemic and also to avoid inadvertently creating incentives to place cost considerations above patient safety. This rule also amends the Medicaid home health regulations to allow other licensed practitioners to order home health services, for the period of this PHE for the COVID-19 pandemic in accordance with state scope of practice laws. We are also modifying our under arrangements policy during the PHE for the COVID-19 pandemic so that hospitals are allowed broader flexibilities to furnish inpatient services, including routine services outside the hospital.
How does telemedicine help Medicare?
Telemedicine, in particular has the potential to play a large role in enhancing the delivery of healthcare in the home, including the provision of information, education , and services provided via telecommunications systems. One of the benefits of telemedicine is its potential to minimize risk to clinicians and patients during an outbreak of an infectious disease, such as the PHE for the COVID-19 pandemic. Recently, we have been asked by stakeholders to provide more clarity on how hospices can leverage technology to keep clinicians and patients safe during the PHE for the COVID-19 pandemic.
What is the PFS 2020?
In the CY 2020 PFS final rule ( 84 FR 62645 and 62646), we finalized allowing the use of interactive two-way audio/video communication technology to furnish the counseling and therapy portions of the weekly bundle of services furnished by OTPs. In light of the PHE for the COVID-19 pandemic, during which the public has been instructed to practice self-isolation or social distancing, and because interactive audio-video communication technology may not be available to all beneficiaries, we are revising § 410.67 (b) (3) and (4) to allow the therapy and counseling portions of the weekly bundles, as well as the add-on code for additional counseling or therapy, to be furnished using audio-only telephone calls rather than via two-way interactive audio-video communication technology during the PHE for the COVID-19 pandemic if beneficiaries do not have access to two-way audio/video communications technology, provided all other applicable requirements are met. We believe this change is necessary to ensure that beneficiaries with opioid use disorders are able to continue to receive these important services during the current PHE.
Is the IFC retroactive?
March 1, 2020 precedes the date of publication of this IFC in the Federal Register, which means this rule has a retroactive effect. However, section 1872 (e) (1) (A) (ii) of the Act permits the Secretary to issue a rule with retroactive effect if the failure to do so would be contrary to the public interest.
Does Medicare pay for telehealth?
[ 15] Starting on March 1, 2020, Medicare can pay for telehealth services, including office, hospital, and other visits furnished by physicians and other practitioners to patients located anywhere across the country including in a patient's place of residence. We have been asked by stakeholders to clarify whether this expansion applies to teaching physician services, including those furnished under the primary care exception. We believe that allowing Medicare payment for services billed by the teaching physician when the resident is furnishing services, including office/outpatient E/M services provided in primary care centers, via telehealth under direct supervision by interactive telecommunications technology would allow residents to furnish services remotely to patients who may need to be isolated for purposes of exposure risk based on presumed or confirmed COVID-19 infection, and as a result, would increase access to services for patients. To increase the capacity of teaching settings to respond to the PHE for the COVID-19 pandemic as more practitioners are increasingly being asked to assist with the COVID-19 response, we believe that, for telehealth services involving residents, the requirement that a teaching physician be present for key portions of the service can be met through virtual means. We also believe same is true for telehealth services furnished by the resident in primary care centers. The use of real-time, audio and video telecommunications technology allows for the teaching physician to interact with the resident through virtual means while the resident is furnishing services via telecommunications technology, and thus, in the circumstances of the PHE, would meet the requirement for teaching physician presence for office/outpatient E/M services furnished in primary care centers. Consequently, on an interim basis for the duration of the PHE for the COVID-19 pandemic, we are revising our regulations to specify that Medicare may make payment under the PFS for teaching physician services when a resident furnishes telehealth services to beneficiaries under direct supervision of the teaching physician which is provided by interactive telecommunications technology. Additionally, on an interim basis, for the duration of the PHE for the COVID-19 pandemic, Medicare may make payment under the PFS for services billed under the primary care exception by the teaching physician when a resident furnishes telehealth services to beneficiaries under the direct supervision of the teaching physician by interactive telecommunications technology. We also seek comment on our belief that direct supervision by interactive telecommunications technology is appropriate in the context of this PHE, as well as whether and how it balances risks that might be introduced for beneficiaries with reducing exposure risk and the increased spread of the disease, in the context of this PHE.