
The Medicare Secondary Payer (MSP) provisions protect the Medicare Trust Fund from making payments when another entity has the responsibility of paying first. Any entity providing items and services to Medicare patients must determine if Medicare is the primary payer.
Full Answer
How to bill Medicare as secondary payer?
What it means to pay primary/secondary
- The insurance that pays first (primary payer) pays up to the limits of its coverage.
- The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover.
- The secondary payer (which may be Medicare) may not pay all the uncovered costs.
What does it mean when Medicare is a secondary payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility; that is, when another entity has the responsibility for paying beforeMedicare. Over the years, Congress has made an effort to shift costs from Medicare to the appropriate private sources of payment, which has resulted in significant savings to the Medicare Trust Fund.
How does Medicare work as a secondary payer?
“Medicare pays secondary to other insurance (including paying in the deductible) in situations where the other insurance is primary to Medicare. Primary Medicare benefits may not be paid if the plan denies payment because the plan does not cover the service for primary payment when provided to Medicare beneficiaries.
How does Medicare calculate secondary payment?
How does Medicare calculate secondary payment? Medicare's secondary payment will be based on the full payment amount (before the reduction for failure to file a proper claim) unless the provider, physician, or other supplier demonstrates that the failure to file a proper claim is attributable to a physical or mental incapacity of the ...
What is Medicare Secondary Payer Rule?
Generally the Medicare Secondary Payer rules prohibit employers with 20 or more employees from in any way incentivizing an active employee age 65 or older to elect Medicare instead of the group health plan, which includes offering a financial incentive.
How does Medicare process secondary claims?
If, after processing the claim, the primary insurer does not pay in full for the services, submit a claim via paper or electronically, to Medicare for consideration of secondary benefits. It is the provider's responsibility to obtain primary insurance information from the beneficiary and bill Medicare appropriately.
Does Medicare submit claims to secondary insurance?
Provider Central If a Medicare member has secondary insurance coverage through one of our plans (such as the Federal Employee Program, Medex, a group policy, or coverage through a vendor), Medicare generally forwards claims to us for processing.
Will secondary pay if primary denies?
If your primary insurance denies coverage, secondary insurance may or may not pay some part of the cost, depending on the insurance. If you do not have primary insurance, your secondary insurance may make little or no payment for your health care costs.
When would a biller most likely submit a claim to secondary insurance?
If a claim has a remaining balance after the primary insurance has paid, you will want to submit the claim to the secondary insurance, if one applies. This article assumes that the primary insurance did not cross over the claim to the secondary insurance on your behalf.
What is the timely filing limit for Medicare secondary claims?
12 monthsQuestion: What is the filing limit for Medicare Secondary Payer (MSP) claims? Answer: The timely filing requirement for primary or secondary claims is one calendar year (12 months) from the date of service.
When submitting a secondary claim what fields will the secondary insurance be in?
Secondary insurance of the patient is chosen as primary insurance for this secondary claim; primary insurance in the primary claim is chosen as secondary insurance in the secondary claim. Payment received from primary payer should be put in 'Amount Paid (Copay)(29)' field in Step-2 of Secondary claim wizard.
What determines if Medicare is primary or secondary?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
Is Medicare Secondary Payer questionnaire required?
Providers are required to complete a Medicare Secondary Payer Questionnaire (MSPQ) upon admission of each Medicare patient. A sample of the MSPQ can be found in the Centers for Medicare & Medicaid Services' (CMS) Internet-Only Manual (IOM), Publication 100-05, Medicare Secondary Payer Manual, Chapter 3, Section 20.2.
How does billing work with 2 insurances?
If you have multiple health insurance policies, you'll have to pay any applicable premiums and deductibles for both plans. Your secondary insurance won't pay toward your primary's deductible. You may also owe other cost sharing or out-of-pocket costs, such as copayments or coinsurance.
What is the Medicare Secondary Payer questionnaire?
CMS developed an MSP questionnaire for providers to use as a guide to help identify other payers that may be primary to Medicare. This questionnaire is a model of the type of questions you should ask to help identify MSP situations.
How do you fill out CMS 1500 when Medicare is secondary?
0:239:21Medicare Secondary Payer (MSP) CMS-1500 Submission - YouTubeYouTubeStart of suggested clipEnd of suggested clipHere when the insured. And the patient are the same the biller enters the word. Same if medicare isMoreHere when the insured. And the patient are the same the biller enters the word. Same if medicare is primary this item is left blank.
What is Medicare Secondary Payer?
The Medicare Secondary Payer (MSP) provisions protect the Medicare Trust Fund from making payments when another entity has the responsibility of paying first. Any entity providing items and services to Medicare patients must determine if Medicare is the primary payer. This booklet gives an overview of the MSP provisions and explains your responsibilities in detail.
What happens if you don't file a claim with the primary payer?
File proper and timely claims with the primary payer. Not filing proper and timely claims with the primary payer may result in claim denial. Policies vary depending on the payer; check with the payer to learn its specific policies.
What is MSP in Medicare?
MSP provisions prevent Medicare paying items and services when patients have other primary health insurance coverage. In these cases, the MSP Program contributes:
Why does Medicare make a conditional payment?
Medicare may make pending case conditional payments to avoid imposing a financial hardship on you and the patient while awaiting a contested case decision.
How long does it take to pay a no fault claim?
For no-fault insurance and WC claims, “paid promptly” means payment within 120 days after the no-fault insurance or WC carrier got the claim for specific items and services. Without contradicting information, you must treat the service date for specific items and services as the claim date when determining the paid promptly period; for inpatient services, you must treat the discharge date as the service date.
Does Medicare pay first when there is no fault?
no-fault pays first when there’s Ongoing Responsibility for Medicals (ORM) reported. Medicare doesn’t make a payment.
Can Medicare make a payment?
Medicare can’t make payment when payment “has been made or can reasonably be expected to be made” under liability insurance (including self-insurance), no-fault insurance, or a WC law or plan of the United States, called a primary plan.
When a provider receives a reduced no fault payment because of failure to file a proper claim, what is?
When a provider receives a reduced no-fault payment because of failure to file a proper claim, (see Chapter 1, §20 for definition), the Medicare secondary payment may not exceed the amount that would have been payable if the no-fault insurer had paid on the basis of a proper claim.
How often do you need to collect MSP information?
Following the initial collection, the MSP information should be verified once every 90 days. If the MSP information collected by the hospital, from the beneficiary or his/her representative and used for billing, is no older than 90 calendar days from the date the service was rendered, then that information may be used to bill Medicare for recurring outpatient services furnished by hospitals. This policy, however, will not be a valid defense to Medicare’s right to recover when a mistaken payment situation is later found to exist.
Is GHP primary to Medicare?
Do you have employer group health plan (GHP) coverage through yourself, a spouse, or family member if dually entitled based on Disability and ESRD? If yes, the employer GHP may be primary to Medicare. Continue below.
Can a beneficiary recall his/her retirement date?
During the intake process, when a beneficiary cannot recall his/her precise retirement date as it relates to coverage under a group health plan as a policyholder or cannot recall the same information as it relates to his/her spouse, as applicable, hospitals must follow the policy below.
Does Medicare require independent labs to collect MSP?
The Centers for Medicare & Medicaid Services (CMS) will not require independent reference laboratories to collect MSP information in order to bill Medicare for reference laboratory services as described in subsection (b) above. Therefore, pursuant to section 943 of The Medicare Prescription Drug, Improvement & Modernization Act of 2003, CMS will not require hospitals to collect MSP information in order to bill Medicare for reference laboratory services as described in subsection (b) above. This policy, however, will not be a valid defense to Medicare’s right to recover when a mistaken payment situation is later found to exist.
Can you send a claim to Medicare with multiple primary payers?
Claims with multiple primary payers cannot be sent electronically to Medicare.
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare. When Medicare began in 1966, it was the primary payer for all claims except for those covered by Workers' Compensation, ...
What age is Medicare?
Retiree Health Plans. Individual is age 65 or older and has an employer retirement plan: Medicare pays Primary, Retiree coverage pays secondary. 6. No-fault Insurance and Liability Insurance. Individual is entitled to Medicare and was in an accident or other situation where no-fault or liability insurance is involved.
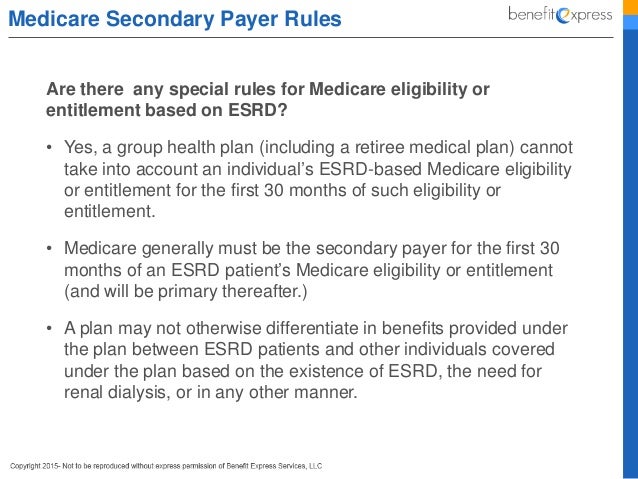
How long does ESRD last on Medicare?
Individual has ESRD, is covered by a GHP and is in the first 30 months of eligibility or entitlement to Medicare. GHP pays Primary, Medicare pays secondary during 30-month coordination period for ESRD.
What are the responsibilities of an employer under MSP?
As an employer, you must: Ensure that your plans identify those individuals to whom the MSP requirement applies; Ensure that your plans provide for proper primary payments whereby law Medicare is the secondary payer; and.
Why is Medicare conditional?
Medicare makes this conditional payment so that the beneficiary won’t have to use his own money to pay the bill. The payment is “conditional” because it must be repaid to Medicare when a settlement, judgment, award or other payment is made. Federal law takes precedence over state laws and private contracts.
When did Medicare start?
When Medicare began in 1966 , it was the primary payer for all claims except for those covered by Workers' Compensation, Federal Black Lung benefits, and Veteran’s Administration (VA) benefits.
Is Medicare the primary payer?
Medicare remains the primary payer for beneficiaries who are not covered by other types of health insurance or coverage. Medicare is also the primary payer in certain instances, provided several conditions are met.
When will Medicare not pay a contractor?
The contractor will not make any Medicare payment if the beneficiary has not filed a claim or cooperated fully with the provider, physician or other supplier or the GHP. Also, the contractor will not make any Medicare payments until the beneficiary has exhausted the entire claims process. Conditional benefits are not payable if payment cannot be made under the GHP because the beneficiary failed to file a proper claim (See §20 for definition of proper claim) unless the failure to file a proper claim is due to mental or physical incapacity of the beneficiary. A beneficiary need not file any appeal if not inclined to do so.
What is the prohibition on Medicare?
An employer or other entity is prohibited from offering Medicare beneficiaries financial or other benefits as incentives not to enroll in or to terminate enrollment in a GHP or LGHP that is or would be primary to Medicare. This prohibition precludes the offering of benefits to Medicare beneficiaries that are alternatives to the employer's primary plan (e.g., prescription drugs) unless the beneficiary has primary coverage other than Medicare. An example would be primary plan coverage through his/her own or a spouse's employer. This rule applies even if the payments or benefits are offered to all other individuals who are eligible for coverage under the plan. It is a violation of the Medicare law every time a prohibited offer is made regardless of whether it is oral or in writing. Any entity that violates the prohibition is subject to a civil money penalty of up to $5,000 for each violation.
What is a senior federal judge?
Senior Federal judges are retired judges of the U.S. court system and the Tax Court. They may continue to adjudicate cases, but they are entitled to full salary as a retirement benefit whether or not they perform judicial services for the Government. By law, the remuneration they receive as senior judges is not considered wages for Social Security retirement offset purposes. Since they are considered retired for Social Security purposes, they are not considered to have current employment status for purposes of the working aged and disability provisions.
How long does a CMS hearing take?
Employer and employee organizations have 65 days from the date of their notice to request a hearing.
What is the right to collect double damages?
Section 1862(b)(3)(A) of the Act provides that any claimant (including a beneficiary, provider, physician, or supplier) has the right to take legal action against, and to collect double damages from a GHP, that fails to pay primary benefits for services covered by the GHP. Any claimant, also, has the right to take legal action against, and to collect double damages from, a no-fault or liability insurer that fails to pay primary benefits for services covered by the no-fault or liability insurer where required to do so under §1862(b) of the Act.
What age do you have to be to get Medicare?
Section 1862(b)(1)(A)(i)(II) of the Act provides that GHPs of employers of 20 or more employees must provide to any employee or spouse age 65 or older the same benefits under the same conditions that they provide to employees and spouses under 65 if those 65 or older are covered under the plan on the basis of the individual's current employment status or the current employment status of a spouse of any age. The requirement applies regardless of whether the individual or spouse 65 or older is entitled to Medicare.
Does GHP take into account Medicare?
GHP may not take into account that an individual is eligible for or entitled to Medicare benefits on the basis of ESRD during a coordination period described in Chapter 2,
Who is responsible for making sure their primary payer reimburses Medicare?
Medicare recipients may be responsible for making sure their primary payer reimburses Medicare for that payment. Medicare recipients are also responsible for responding to any claims communications from Medicare in order to ensure their coordination of benefits proceeds seamlessly.
What does a primary payer do?
In the simplest of terms, a primary payer will cover the cost of a health care bill according to its policy rules and up to the limit established therein.
How does Medicare work with insurance carriers?
Generally, a Medicare recipient’s health care providers and health insurance carriers work together to coordinate benefits and coverage rules with Medicare. However, it’s important to understand when Medicare acts as the secondary payer if there are choices made on your part that can change how this coordination happens.
What is ESRD covered by?
Diagnosed with End-Stage Renal Disease (ESRD) and covered by a group health plan or COBRA plan; Medicare becomes the primary payer after a 30-day coordination period.
How old do you have to be to be covered by a group health plan?
Over the age of 65 and covered by an employment-related group health plan as a current employee or the spouse of a current employee in an organization that shares a plan with other employers with more than 20 employees between them.
Is Medicare a secondary payer?
Medicare is the secondary payer if the recipient is: Over the age of 65 and covered by an employment-related group health plan as a current employee or the spouse of a current employee in an organization with more than 20 employees.
Who is covered by an employment-related group health plan?
Disabled and covered by an employment-related group health plan as a current employee or the spouse of a current employee in an organization that shares a plan with other employers with more than 100 employees between them.
