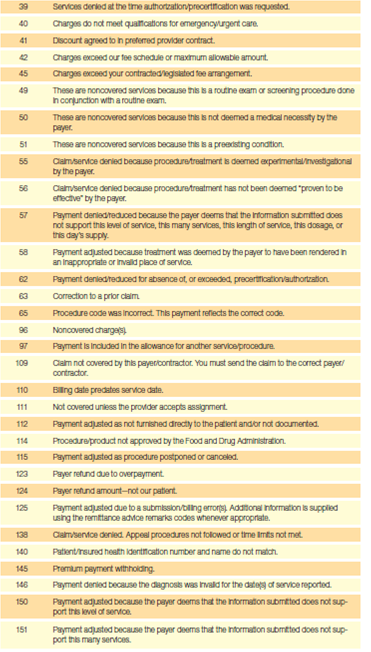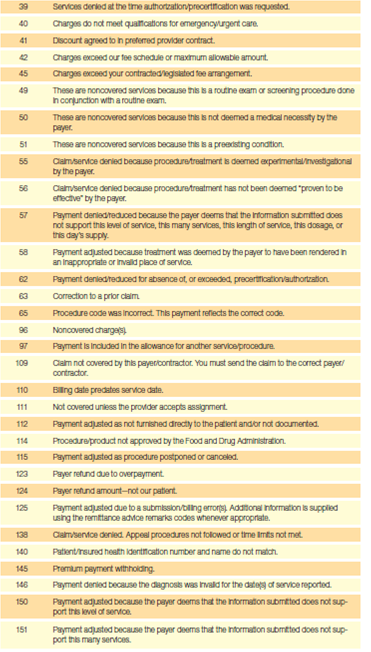
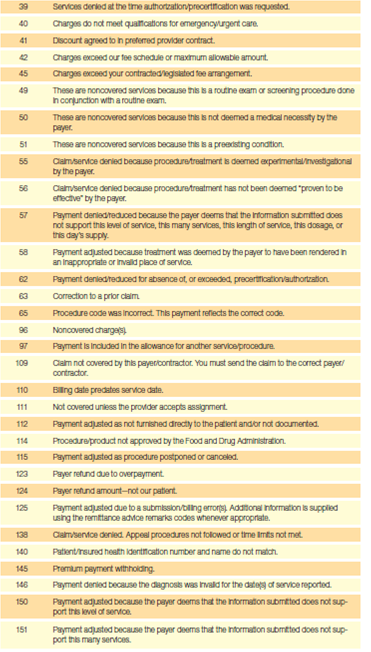
The KX modifier is a signal on a claim that though the patient services have met the capped amount allowed, the provider deems continued care medically necessary. As the description in the below table indicates, medical record documentation must be maintained to support the medical necessity of the continued services.
When to use the KX modifier?
- When the original NOE was submitted;
- When the NOE was returned to the hospice (RTPs) for correction or was accepted and available for correction; and
- When the hospice resubmitted the NOE.
What does modifier Kx mean?
What you need to know
- Appropriate Use: When additional documentation supports the medical requirements of the service under a valid medical policy.
- Inappropriate Use: When the claim provides all information on the service billed and medical documentation does not provide further explanation.
- Physical/Speech/Occupational Therapy. ...
How to add Kx modifier?
- Qualified for the cap exception;
- Are reasonable and necessary services that require the skills of a therapist; and
- Are justified by appropriate documentation in the medical record.”
What is Kx modifier used for?
The KX modifier is used by DME suppliers to ensure that the records exist and are available to support that the claim has followed Medical Policy and the LCD for that item.
What is modifier code KX?
The KX modifier is a signal on a claim that though the patient services have met the capped amount allowed, the provider deems continued care medically necessary. As the description in the below table indicates, medical record documentation must be maintained to support the medical necessity of the continued services.
What does the KX modifier mean for DME?
The KX modifier represents the presence of required documentation is on file to support the medical necessity of the item.
Where do you put the KX modifier?
The KX modifier is appended on claims at or very close to the $1920 cap, and should not applied from the first visit, even if the therapist knows that the cap will likely be exceeded.
What is the KX modifier threshold?
The KX modifier threshold process applies an annual Medical Record (MR) threshold amount when a beneficiary's incurred expenses reach a threshold of $3,000. This amount will remain until calendar year 2028.
What is a KX?
The KX modifier is a Medicare-specific modifier that indicates a beneficiary has gone above their therapy threshold amount. To my knowledge, there are no other insurance payers that use this modifier. I hope that helps!
Does modifier KX affect payment?
When the KX modifier is appended to a therapy HCPCS code, the contractor will override the CWF system reject for services that exceed the caps and pay the claim if it is otherwise payable.
How long can you use KX modifier?
Nope, there is no upper limit—as long as the services you are providing are medically necessary. However, there are additional steps you must take if you believe treatment beyond the manual medical review threshold of $3,700 is medically necessary.
Does Aetna require KX modifier?
Effective June 1, 2020, we'll allow hemodialysis services billed with modifier KX. You can use this modifier to report services required in excess of the three times per seven-day period. Be sure to include the KX modifier on your bill to us, if necessary.
Does Medicare require modifiers for physical therapy?
**One last quick tip, for therapy businesses who have PTAs or OTAs, Medicare now requires that you use an assistant modifier, CQ for PTAs and CO for OTAs, for services performed.
What is the KX modifier threshold for 2020?
For CY 2020, the KX modifier threshold amounts are: (a) $2,080 for Physical Therapy (PT) and Speech-Language Pathology (SLP) services combined, and (b) $2,080 for Occupational Therapy (OT) services. Make sure your billing staffs are aware of these updates.
What are the Medicare therapy Threshold limits for 2021?
For CY 2021 (and each calendar year until 2028 at which time it is indexed annually by the MEI), the MR threshold is $3,000 for PT and SLP services and $3,000 for OT services. The targeted MR process means that not all claims exceeding the MR threshold amount are subject to review as they once were.
How many PT sessions will Medicare pay for?
There's no limit on how much Medicare pays for your medically necessary outpatient therapy services in one calendar year.
Modifier KX
Use of the KX modifier indicates that the supplier has ensured coverage criteria for the DMEPOS billed is met and that documentation does exist to support the medical necessity of item. Documentation must be available upon request.
Incorrect Use
Append KX modifier to claim without verifying coverage criteria and existence of documentation
Appeal Option
Denied claims requiring a change specific to KX modifier, whether it be adding or removing it, must be requested via Written Redetermination only
What is KX modifier?
The KX modifier has differing requirements for usage depending on the specific Local Coverage Determination (LCD); suppliers should review the LCD/Article’s carefully to understand the documentation requirements and the proper use of the KX modifier for each policy.
What is Medicare Advantage Policy Guideline?
The Medicare Advantage Policy Guideline documents are generally used to support UnitedHealthcare Medicare Advantage claims processing activities and facilitate providers’ submission of accurate claims for the specified services. The document can be used as a guide to help determine applicable:
When do you need to submit KX modifier?
Providers of outpatient therapy services are required to submit the KX modifier on their therapy claims, when an exception to the cap is requested for medically necessary services.
When did the KX modifier expire?
Section 202 of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) extended the therapy cap exceptions process through December 31, 2017. As a reminder, excessive use of the KX modifier including routine use of the modifier prior to reaching the cap limits may indicate abusive billing.
What is the KX modifier?
A: The KX modifier is added to claim lines to indicate that the clinician attests that services are medically necessary and justification is documented in the medical record. Even though no special documentation is submitted to the contractor for automatic process exceptions, the clinician is responsible for consulting guidance in the Medicare manuals and in the professional literature to determine if the beneficiary qualifies for the automatic process exception. In addition, the clinician’s opinion is not binding on the Medicare contractor; the Medicare contractor makes the final determination concerning whether the claim is payable.#N#Q: When are exceptions to the therapy caps for services provided in a SNF setting considered?#N#Revised 09/2015
When exceptions are in effect and the beneficiary qualifies for a therapy cap exception, the provider shall add
When exceptions are in effect and the beneficiary qualifies for a therapy cap exception, the provider shall add a KX modifier to the therapy HCPCS code subject to the cap limits. The KX modifier shall not be added to any line of service that is not a medically necessary service; this applies to services that, according to a local coverage determination by the contractor, are not medically necessary services.
What is documentation justifying services?
A: Documentation justifying the services shall be submitted in response to any Additional Documentation Request (ADR) for claims that are selected for medical review. If medical records are requested for review, clinicians may include, at their discretion, a summary that specifically addresses the justification for therapy cap exception and they should follow the documentation requirements listed
When can a beneficiary use the cap exceptions process?
The beneficiary may qualify for use of the cap exceptions process at any time during the episode when documented medically necessary services exceed caps. All covered and medically necessary services qualify for exceptions to caps. All requests for exception are in the form of a KX modifier added to claim lines.
Can you use KX modifier on PT lines?
o Use the KX modifier on either all or none of the SLP lines on the claim, as appropriate. In contrast, if all the OT lines on the claim are below the cap, do not use the KX modifier on any of the OT lines, even when the KX modifier is appropriately used on all of the PT lines.
When to use KX modifier?
Apply the KX modifier when you provide medically necessary services above the soft cap. Therapists should continue to affix the KX modifier to all medically necessary services above the designated limit ($2,010 in 2018), thus signaling Medicare to pay the claim. That means you must continue to track your patients’ progress toward ...
Can you still submit a claim to Medicare with a GA modifier?
Once you have a signed ABN on file, you should still submit claims to Medicare—with a GA modifier, which will trigger Medicare to reject those claims. Then, after you receive the denial from Medicare, you can collect payment for those services directly from your patients.
What is Medicare Administrative Contractor?
The Medicare Administrative Contractor is hereby advised that this constitutes technical direction as defined in your contract. CMS does not construe this as a change to the MAC Statement of Work. The contractor is not obligated to incur costs in excess of the amounts allotted in your contract unless and until specifically authorized by the Contracting Officer. If the contractor considers anything provided, as described above, to be outside the current scope of work, the contractor shall withhold performance on the part(s) in question and immediately notify the Contracting Officer, in writing or by e-mail, and request formal directions regarding continued performance requirements.
Does the revision date apply to red italicized material?
Disclaimer for manual changes only: The revision date and transmittal number apply only to red italicized material. Any other material was previously published and remains unchanged. However, if this revision contains a table of contents, you will receive the new/revised information only, and not the entire table of contents.