Who qualifies for continuous glucose monitoring?
What is Medicare standard utilization guidelines for diabetic testing supplies?
What are the new guidelines for A1C?
Can you qualify for Medicare if you have diabetes?
What are lancets?
Why is insulin not covered by Medicare?
What should your A1C be if you are over 65?
What is the average blood sugar for an A1C of 7?
...
A1C and self-monitoring.
| A1C level | Estimated average blood sugar (glucose) level |
|---|---|
| 7% | 154 mg/dL (8.6 mmol/L) |
| 8% | 183 mg/dL (10.2 mmol/L) |
| 9% | 212 mg/dL (11.8 mmol/L) |
What is normal A1C for seniors?
Does Medicare pay for A1c test?
What brand of glucose meter does Medicare 2020 cover?
What brand of glucose meter does Medicare 2022 cover?
Does Medicare cover diabetes?
This section provides information about Medicare drug coverage (Part D) for people with Medicare who have or are at risk for diabetes. To get Medicare drug coverage, you must join a Medicare drug plan. Medicare drug plans cover these diabetes drugs and supplies:
How long can you have Medicare Part B?
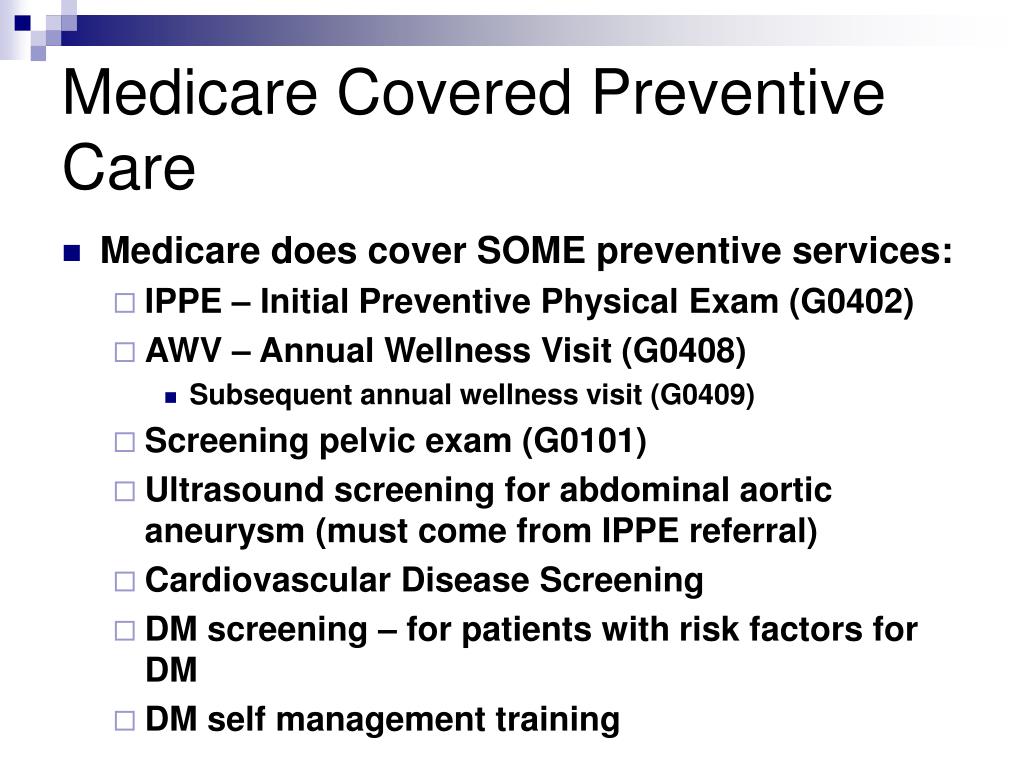
If you’ve had Medicare Part B for longer than 12 months , you can get a yearly “Wellness” visit to develop or update a personalized prevention plan based on your current health and risk factors. This includes:
What is diabetes self management training?
Diabetes self-management training helps you learn how to successfully manage your diabetes. Your doctor or other health care provider must prescribe this training for Part B to cover it.
What is Part B for diabetes?
In addition to diabetes self-management training, Part B covers medical nutrition therapy services if you have diabetes or renal disease. To be eligible for these services, your fasting blood sugar has to meet certain criteria. Also, your doctor or other health care provider must prescribe these services for you.
What is coinsurance in insurance?
Coinsurance: An amount you may be required to pay as your share of the cost for services after you pay any deductibles. Coinsurance is usually a percentage (for example, 20%).
Does Part B cover insulin pumps?
Part B may cover insulin pumps worn outside the body (external), including the insulin used with the pump for some people with Part B who have diabetes and who meet certain conditions. Certain insulin pumps are considered durable medical equipment.
What is the A1C test?
A hemoglobin A1c test is a lab test that measures how well your blood sugar has been controlled over the past 3 months. If you have diabetes, Part B covers this test if your doctor orders it.
How long is a DSMT?
Procedure Codes. The 10 initial hours of DSMT and the 2 hours of follow-up DSMT are to be furnished in increments of no less than a 0.5-hour unit of time (30 minutes, face to face), as the procedure codes are 30-minute, time-based codes. Rounding of time furnished is not allowed for 30-minute time-based codes.
Is Medicare a once in a lifetime benefit?
This is a “once-in-a-lifetime” Medicare benefit. A properly executed written or e-referral from the beneficiary’s treating diabetes provider (physician or qualified non-physician practitioner, such as a nurse practitioner, who is medically managing the beneficiary’s diabetes) is required.
What are the requirements for DME?
DME meets these criteria: 1 Durable (can withstand repeated use) 2 Used for a medical reason 3 Not usually useful to someone who isn't sick or injured 4 Used in your home 5 Generally has an expected lifetime of at least 3 years
Does Medicare cover DME equipment?
You may be able to choose whether to rent or buy the equipment. Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare.
What percentage of Medicare payment does a supplier pay for assignment?
If your supplier accepts Assignment you pay 20% of the Medicare-approved amount, and the Part B Deductible applies. Medicare pays for different kinds of DME in different ways. Depending on the type of equipment:
What is original Medicare?
Your costs in Original Medicare. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
What is Medicare assignment?
assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. you pay 20% of the. Medicare-Approved Amount.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B.
What happens if you live in an area that's been declared a disaster or emergency?
If you live in an area that's been declared a disaster or emergency, the usual rules for your medical care may change for a short time. Learn more about how to replace lost or damaged equipment in a disaster or emergency .
Does Medicare cover glucose labs?
Medicare Part B (Medical Insurance) covers glucose laboratory test screenings (with or without a carbohydrate challenge) if your doctor determines you’re at risk for developing diabetes. You may be eligible for up to 2 screenings each year. Part B covers these lab tests if you have any of these risk factors:
What is original Medicare?
Your costs in Original Medicare. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. .
What is Medicare Part B?
Medicare Part B (Medical Insurance) Part B covers certain doctor s' services, outpatient care, medical supplies, and preventive services. covers glucose laboratory test screenings (with or without a carbohydrate challenge) if your doctor determines you’re at risk for developing diabetes. You may be eligible for up to 2 screenings each year.
What is covered by Part B?
covers glucose laboratory test screenings (with or without a carbohydrate challenge) if your doctor determines you’re at risk for developing diabetes. You may be eligible for up to 2 screenings each year. Part B covers these lab tests if you have any of these risk factors: History of abnormal cholesterol and triglyceride levels (dyslipidemia) ...
What is Medicare assignment?
assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. .
What is Part B insurance?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers glucose laboratory test screenings (with or without a carbohydrate challenge) if your doctor determines you’re at risk for developing diabetes.
Does Medicare cover diabetic shoes?
Since Medicare covers diabetic shoes, Medicare Advantage plans will also cover diabetic shoes. Of course, you must still meet all eligibility requirements. And keep in mind, Advantage plans have specific networks. If your particular doctor doesn’t fall into the network, you may not have coverage for your shoes and doctor.
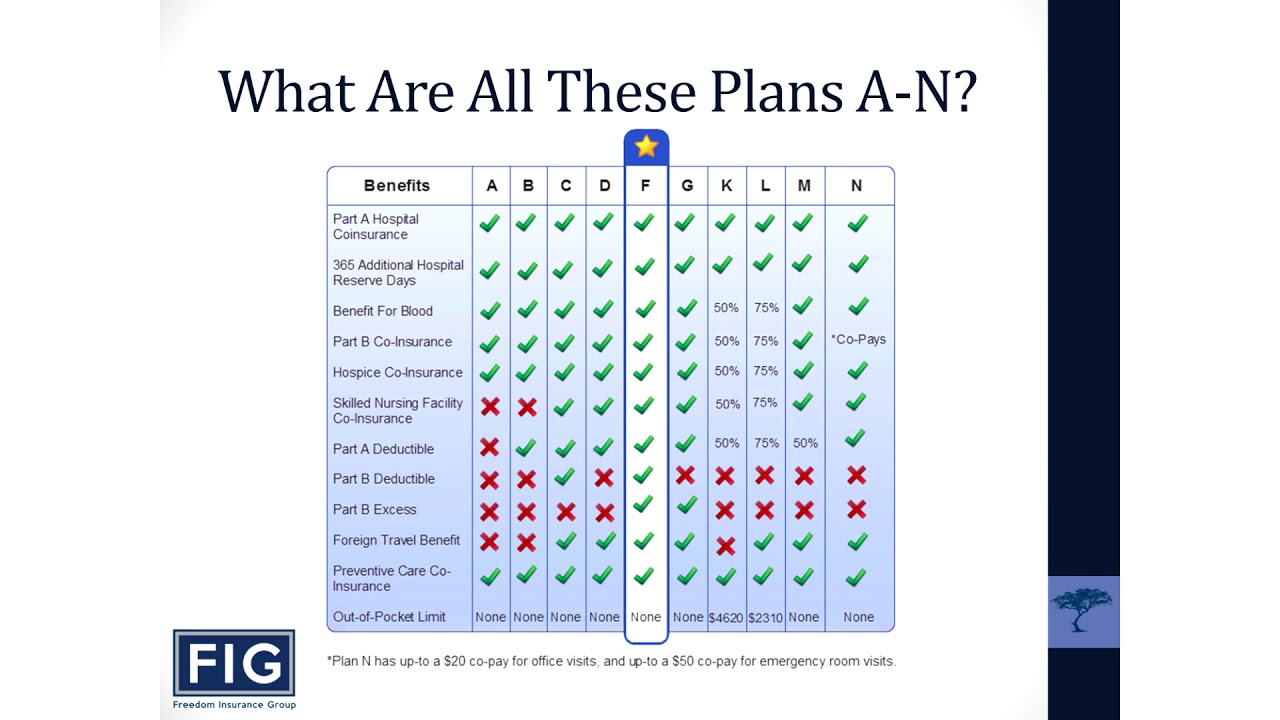
Can diabetics get therapeutic shoes?
If you have diabetes and need therapeutic shoes, your doctor can help get you started. And when you choose to buy Medigap coverage, you can take assurance that your shoes won’t cost you an arm and a leg. Your Medigap plan can help with coinsurance, copays, and your Part B deductible.
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B.
What is original Medicare?
Your costs in Original Medicare. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
What are therapeutic shoes?
Therapeutic shoes & inserts 1 One pair of custom-molded shoes and inserts 2 One pair of extra-depth shoes
Does Medicare cover shoe inserts?
Medicare also covers: 2 additional pairs of inserts each calendar year for custom-molded shoes. 3 pairs of inserts each calendar year for extra-depth shoes. Medicare will cover shoe modifications instead of inserts.
What is Medicare assignment?
assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. , you pay 20% of the. Medicare-Approved Amount.
Does Medicare cover therapeutic shoes?
Medicare will only cover your therapeutic shoes if your doctors and suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare. If your doctors or suppliers aren't enrolled, Medicare won't pay the claims submitted by them. It's also important to ask your suppliers ...
How to find out how much a test is?
To find out how much your test, item, or service will cost, talk to your doctor or health care provider. The specific amount you’ll owe may depend on several things, like: 1 Other insurance you may have 2 How much your doctor charges 3 Whether your doctor accepts assignment 4 The type of facility 5 Where you get your test, item, or service