Those include:
- Medicare Shared Savings Program (MSSP)
- Pioneer ACOs
- Next Generation ACOs
- Comprehensive End Stage Renal Disease (ESRD) Care Model
- Comprehensive Primary Care Model
- Multi-Payer Advanced Primary Care Practice
- End Stage Renal Disease Prospective Payment System
- Maryland All-Payer Model
- Medicare Care Choices Model
- Bundled Payment Care Improvement
What are alternative payment models?
Types of APMs
- APMs. Meet the statutory definition of an APM. ...
- MIPS APMs. MIPS APMs have MIPS eligible clinicians participating in the APM on their CMS-approved participation list.
- Advanced APMs. ...
- Advanced & MIPS APMs. ...
- All-Payer/Other-Payer Option. ...
What is Medicare alternative payment model?
- Comprehensive ESRD Care Model (all tracks)
- Comprehensive Primary Care Plus Model (all tracks)
- Next Generation ACO Model
- Oncology Care Model (all tracks)
- Medicare Shared Savings Program (all tracks)
- Medicare ACO Track 1+ Model
- Bundled Payments for Care Improvement Advanced
- Maryland Total Cost of Care Model
- Vermont All-Payer ACO Model
How does Medicare calculate secondary payment?
How does Medicare calculate secondary payment? Medicare's secondary payment will be based on the full payment amount (before the reduction for failure to file a proper claim) unless the provider, physician, or other supplier demonstrates that the failure to file a proper claim is attributable to a physical or mental incapacity of the ...
What does Medicare pay as the secondary payer?
The Medicare secondary payment is $100. When Medicare is the secondary payer, the combined payment made by the primary payer and Medicare on behalf of the beneficiary is $3,000. The beneficiary has no liability for Medicare-covered services since the primary payment satisfied the $520 deductible.

What are Medicare alternative payment models?
An Alternative Payment Model (APM) is a payment approach that gives added incentive payments to provide high-quality and cost-efficient care. APMs can apply to a specific clinical condition, a care episode, or a population.
What are payment models in healthcare?
Healthcare reimbursement models are billing systems by which healthcare organizations get paid for the services they provide to patients, whether by insurance payers or patients themselves.
What are the models of payment?
We consider how three broad payment models stack up against these criteria: fee-for-service (FFS), episode-based payment (EBP), and population-based payment (PBP).
What are the four main methods of reimbursement?
Here are the five most common methods in which hospitals are reimbursed:Discount from Billed Charges. ... Fee-for-Service. ... Value-Based Reimbursement. ... Bundled Payments. ... Shared Savings.
What are two types of payment models?
There are two basic types of bundled payment models: retrospective payment systems and prospective payment systems. In a retrospective payment system, payers retain a fee-for-service (FFS) arrangement and continue to compensate providers directly. But they also track total costs against the predetermined target price.
How many types of payment models are there in healthcare?
There are eight basic health care payment methods available in the world, these methods are more specific [11].
What are advanced payment models?
Advanced Alternative Payment Models (APMs) is a track of the Quality Payment Program that offers incentives for meeting participation thresholds based on your levels of payments or patients through Advanced APMs. If you achieve these thresholds, you become a qualifying APM participant (QP).
What is the difference between MIPS and APM?
MIPS stands for Merit-Based Incentive Payment System, while APM stands for Alternative Payment Model. Health care providers need to begin the verification process this year, and the first payments under these systems will be made in 2019. Both MIPS and APMs are processes that use value-based payment models.
What is risk based payment model?
Risk-based payment models aim to hold providers accountable for better, more efficient care. This model is also called risk-based payer contracts. Providers are paid a fee per patient and are then responsible for treating the patient within this budget.
What are value based payment models?
Value Based Payment (VBP) is a concept by which purchasers of health care (government, employers, and consumers) and payers (public and private) hold the health care delivery system at large (physicians and other providers, hospitals, etc.) accountable for both quality and cost of care.
What is an IPA model HMO?
HMO: IPA Model--An independent practice association is a partnership or association of physicians who offer their services collectively to large provider groups and HMOs. Patients may choose from a list of doctors who contract with the larger provider group of HMO.
What are the four types of HMO models?
Health Maintenance Organization: An organization that provides or arranges for coverage of designated health services needed by plan members for a fixed prepaid premium. There are four basic models of HMOs: group model, individual practice association (IPA), network model, and staff model.
What is an APM in healthcare?
APMs require healthcare organizations (often a hospital and affiliated physician practices) to align themselves with the goal of taking better care of a population of patients, often defined by a geographic region. A common example of an APM is a Medicare Shared Savings Plan (MSSP) also known as an Accountable Care Organization (ACO).
What is an advanced APM?
An Advanced APM is similar to an APM, with some additional criteria. The APM requires participants to use certified EHR technology. The APM bases payment on quality measures comparable to those in the MIPS quality performance category.
What is the final rule for CMS 2021?
In the 2021 Final Rule, CMS announced 2021 would be the final year for web interface and APMs will need to begin participating in the APM Performance Pathway (APP). In addition, CMS announced reporting can happen at the APM entity, individual, and group/TIN level.
Do CMS APMs have unique reporting requirements?
Most CMS APMs have unique reporting requirements. APMs that are considered MIPS APMs may participate in MIPS at the APM entity level. In the past, many APMs have reported via the web interface mechanism, a sampling methodology for reporting on a specific set of attributed patients.
How does Medicare help ACO?
Medicare payments to the ACO are directly tied to cost of care and quality. The money that is saved through the ACO’s efforts is shared with the organization in the form of a bonus as long as it also provides high quality care. The goal is to keep healthcare costs low by creating a payment system based on the quality of care, not the quantity.
What does MIPS stand for in Medicare?
MIPS stands for Merit Based Incentive Payments System. The system includes a number of ACO quality programs and consolidates the Physician Quality Reporting System, Value-Based Payment Modifier, and Meaningful Use of EHRs. It’s the default program for Medicare physicians who aren’t a part of an advanced alternative payment model.
What is the next generation ACO?
The Next Generation ACO Final Rule. The final rule is a set of proposed changes for the Shared Savings Program that were announced in December 2018. One of the most notable parts of the final rule is that it sets the shared savings for ACOs at 40 or 50 percent.
What is an APM?
An advanced alternative payment model (APM) is a program that awards bonuses to ACOs. Physicians who participate in an APM are exempt from Merit Based Incentive Payments System (MIPS) regulations. Participation in an APM makes an ACO eligible for a 5 percent bonus annually from 2019 through 2024.
What is Medicare Shared Savings Program?
The program is designed for higher performing ACOs and similar organizations that have experience offering coordinated care.
What is MACRA in Medicare?
MACRA stands for the Medicare Access and CHIP Reauthorization Act of 2015. The act established the Quality Payment Program that awards the bonuses to ACOs that participate in an alternative payment model (APM). MACRA also outlines the requirements that ACOs must meet to receive financial bonuses from Medicare.
Does Medicare still use fee for service?
Medicare still uses fee-for-service payments with ACOs, but they also offer bonus programs as a way to encourage healthcare groups to focus on quality not quantity when it comes to treatment, illness prevention and managing chronic diseases. The bonus programs also aim to keep costs from rising.
What is Medicare 5%?
In the Medicare Access and CHIP Reauthorization Act (MACRA), it authorized paying a 5% annual lump sum payment to physicians who participate in qualified APMs at certain threshold levels, and it also exempted those physicians from the Merit-Based Incentive Payment System (MIPS).
What is the purpose of the Physician-Focused Payment Model Technical Advisory Committee (PTAC)?
Congress created an independent committee called the Physician-Focused Payment Model Technical Advisory Committee (PTAC) to review APMs developed by physicians and to recommend which proposals should be implemented in the Medicare program. How the AMA helps physicians design patient-centered APMs.
What is APM in hospice?
An APM developed by the American Academy of Hospice and Palliative Medicine, supported by the AMA, and recommended by PTAC would enable physician-led teams to provide home-based palliative care services to patients with serious, potentially life-limiting illnesses, not just patients on hospice.
What is APM in emergency medicine?
Emergency care. An APM developed by the American College of Emergency Physicians and recommended by PTAC would provide the resources emergency physicians need to increase the number of patients who can be sent home after an emergency department visit rather than being admitted to the hospital.
What is an APM in cancer?
An APM developed by an oncologist and recommended by PTAC is designed to support enhanced services for cancer patients that can reduce the frequency of emergency department visits and hospital admissions for complications of chemotherapy. A similar grant-funded project successfully reduced spending while improving the quality of life for cancer patients, and the AMA has supported implementation of this APM so that all oncologists can replicate this success.
Why is it important for physicians to be involved in the design of APMs?
However, it is essential for physicians to be involved in the design of APMs to ensure that the APMs successfully remove the barriers physicians currently face in delivering high-quality care to their patients, and that the APMs do not require physicians to be accountable for spending or outcomes they cannot control.
What is APM in healthcare?
An APM is a different way of compensating physicians for patient care. Physicians face barriers in the standard payment systems used by Medicare and other payers that prevent them from delivering all of the services their patients need and delivering services in ways that will work best for individual patients.
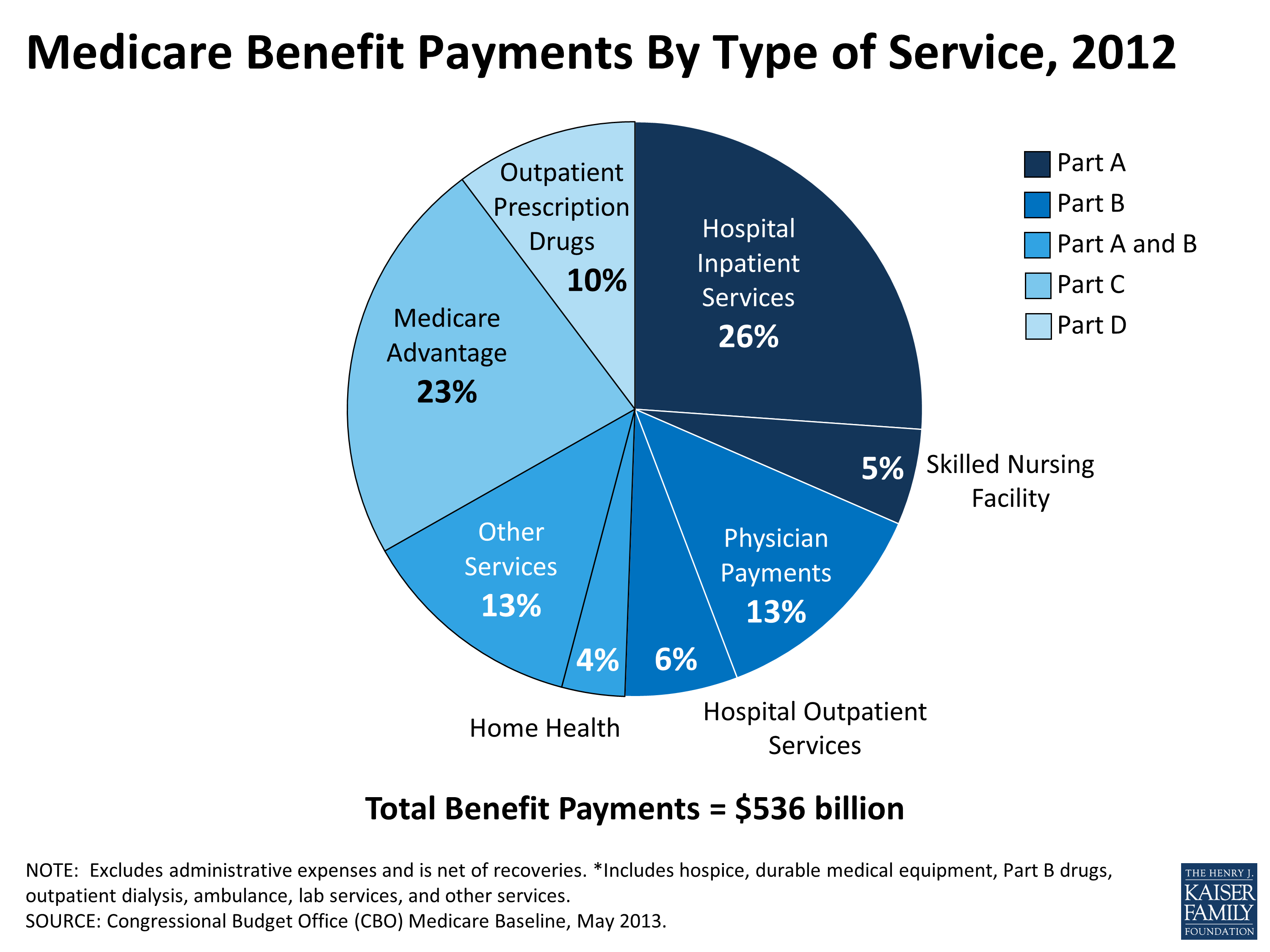
How much money is spent on Medicare inpatients?
Inpatient PPS. One in every five Medicare beneficiaries is hospitalized one or more times each year. Of the approximately $300 billion dollars spent on the Medicare program each year, almost $100 billion is spent on inpatient services. More than three-quarters of the nation's inpatient acute-care ...
What is a patient centered medical home?
According to the Agency for Healthcare Research and Quality, the patient-centered medical home encompasses: 1. Comprehensive care that meets the large majority of each patient’s physical and mental health care needs, including prevention and wellness, acute care, and chronic care. 2.
What is value based purchasing?
The Hospital Value-Based Purchasing Program seeks to improve patient safety and experience by basing Medicare payments on the quality of care provided, rather than on the quantity of services performed. Hospital VBP affects payment for inpatient stays in more than 3,000 hospitals across...
Is health care based on value?
Health care is currently in the middle of a transition from a system of payment based on the volume of services provided (fee-for-service) to payment based on the value of those services (value-based care and alternative payment models).
Does Medicare have a bundle payment?
Traditionally, Medicare has made separate payments to providers for each of the individual services they furnish to beneficiaries for a certain illness or course of treatment. However, policymakers and providers have become increasingly concerned that this approach may result in fragmen...
Does Medicare pay for psychiatric PPS?
Psychiatric PPS. Medicare pays for these services through the IPF prospective payment system, which uses pre-determined rates based primarily on the patient’s condition (age, diagnosis, comorbidities) and length of stay, and the location of the IPF. Medicare also provides additional payment for IPFs tha...
What is the Maryland All Payer Model?
Maryland All-Payer Model: The state of Maryland adopted a hospital global budget payment program in which all payers pay hospitals a fixed annual amount for inpatient and outpatient services, irrespective of hospital utilization (in other words, one annual budget unrelated to the number of patients admitted).
When did Medicare start care choices?
Medicare Care Choices Model: Launched in July 2015, this model provides new options for hospice patients by allowing Medicare beneficiaries who qualify for hospice to receive palliative care services and curative care at the same time, and many of these services are available 24/7.
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS) has deployed multiple alternative payment models that increasingly tie Medicare payments to value, meaning the quality and efficiency of the care delivered.
How much did Maryland save in Medicare?
In year 1, the composite quality measure of preventable conditions improved by over 26 percent, and Maryland decreased absolute overall per capita Medicare hospital costs by 1.08 percent, saving Medicare $116 million.
