What is a Medicare rug rate? The base rate for nontherapy RUGs is $16, and it covers, for example, the costs incurred by skilled nursing facilities in determining whether beneficiaries require therapy. What does Medicare cover for extended care facility costs?
What is a rug level in pharmacy?
The American Society of Consultant Pharmacists advises that a patient’s RUG level is calculated based on information found on the patient’s Minimum Data Set, also know as an MDS. The RUG level then determines the per diem rate that the facility receives.
What is the rug rate reduction for SNFS that did not submit data?
SNFs that did not submit quality data are subject to a 2% reduction to their RUG rate. Please note, this is NOT related to sequestration. Effective with claims discharged on October 1, 2018, the SNF Value-Based Program (VBP) became effective. Medicare will adjust RUG rates as needed based on the VBP factor published by CMS.
What is a rug group in long-term care?
A RUG, or resource utilization group, is used to classify patients in long-term care facilities based on the care the patient requires, according to the Texas Department of Aging and Disability Services. As of 2014, there are 34 RUG groups.
Are evaluation minutes included in the calculation of rug rates?
Time spent on evaluation was included in the calculation of the RUG rates; therefore, evaluation minutes are already accounted for and are not to be reported.
What does rug level mean?
The RUG score shows the type and quantity of care required for each individual resident. RUG scores consist primarily of the levels of occupational, physical and speech therapy a patient receives along with the intensity of nursing services the patient requires.
What does rug mean in MDS?
Resource Utilization GroupsResource Utilization Groups, or RUGs, flow from the Minimum Data Set (MDS) and drive Medicare reimbursement to nursing homes under the Prospective Payment System (PPS). A resident is initially assigned to one of the seven major categories of RUGs based on their clinical characteristics and functional abilities.
What are Medicare rug rates?
The base rate for nontherapy RUGs is $16 and covers, for example, SNFs' costs for evaluating beneficiaries to determine whether they need therapy.
Does Medicare still use RUGs?
New Medicare Payment Model, PDPM, Proposes to Replace RUGs System for SNFs. On April 27, 2018, the Centers for Medicare and Medicaid Services (CMS) announced a proposal to replace the Resource Utilization Groups (RUGs) payment system with a new model for Medicare payment of skilled nursing care.
What is RUGS IV?
RUG-IV is a patient classification system for skilled nursing patients used by the federal government to determine reimbursement levels. This method is stemming from the SNF PPS FY2012 Final Rule and was previously RUG-III.
What is a rug in medical term?
A retrograde urethrogram (RUG) is a diagnostic procedure performed most commonly in male patients to diagnose urethral pathology such as trauma to the urethra or urethral stricture. [1, 2]
How is PDPM score calculated?
The PDPM Function Score for PT Payment ranges from 0 through 24. Using the responses from Steps 1 and 2 above, determine the resident's PT group using the table below. 1 Calculate the sum of the Function Scores for Sit to Lying and Lying to Sitting on Side of Bed. Divide this sum by 2.
How does the SNF PPS system determine payment?
Case Mix Adjustment: Payments under the SNF PPS are case-mix adjusted in order to reflect the relative resource intensity that would typically be associated with a given patient's clinical condition, as identified through the resident assessment process.
What is NF B SNF?
Skilled Nursing Facilities All Freestanding Skilled Nursing Facilities, Level-B, (FS/NF-B), and Freestanding Skilled Adult Subacute Nursing Facilities, Level-B, (FSSA/NF-B), except those that are exempt under Health and Safety Code, section 1324.20(c), are required to pay the QAF.
What are RUG categories?
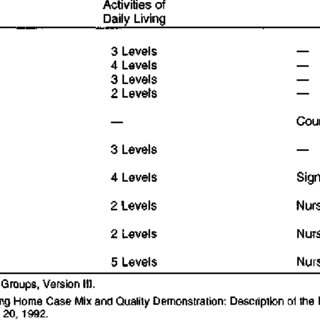
There are seven major RUG categories: Rehabilitation, Extensive Services, Special Care, Clinically Complex, Impaired Cognition, Behavior Problems, and Reduced Physical Function.
What are DRGs and rugs?
Based on a patient classification case-mix system, the Resource Utilization Group (RUG) relies on specific nursing documentation of patient care delivered, that is, resource used. Implemented at the same time as diagnostic-related groups (DRGs), the RUGs system is not based on length of stay, diagnosis, or age.
What does rug mean in therapy?
What is meant by “RUG IV”, “Concurrent Therapy” and “Look Back”? RUG stands for “Resource Utilization Group”. RUGs are significant because they are the core of the SNF payment system under Medicare Part A since July 1, 1998, and have been modified several times.
Final Report
This is the final report from the Urban Institute (March 2007) that describes data sources and methodological approaches used in the research of the RUG-III refinements.
Data
Updated RUG-53 Unadjusted Case Mix Indices --The updated nursing and therapy case mix index chart shows the distributional impact of adding 9 new groups to the RUG-III hierarchy. The addition of the new groups requires a recalibration of the case mix indices for all the RUG-III groups.
How many days per week is skilled care?
If rehabilitation is the primary reason for a skilled level of care, the facility has to ensure therapy is clinically indicated at least 5 days per week in order for the patient to meet Medicare skilled coverage criteria.
Is SNF coverage daily basis?
As detailed in Chapter 8 of the Medicare Benefit Policy Manual, “Unless there is a legitimate medical need for scheduling a therapy session each day, the “daily basis” requirement for SNF coverage would not be met.”.
How long does a patient have to stay in an acute care hospital to qualify for SNF?
To qualify for admission to the SNF under the Part A benefit, the patient must have had a prior stay of at least three days in an acute care hospital.
When did Medicare change the payment system for audiologists?
The SNF payment system changed significantly on October 1, 2019. See the Medicare Patient-Driven Payment Model (PDPM) for more information.
What happens if a SNF does not have an SLP?
For example, if the SNF does not have an SLP on staff, they must contract with an SLP to provide the necessary services. In this scenario, the agency would bill Medicare for the SLP’s services and pay the SLP a negotiated rate. CMS does not dictate the amount a contract employee is paid.
What is consolidated billing in Medicare?
Consolidated billing is a mechanism established by CMS to prevent double billing for services. For example, if the SNF does not have an SLP on staff, they must contract with an SLP to provide the necessary services. In this scenario, the agency would bill Medicare for the SLP’s services and pay the SLP a negotiated rate. CMS does not dictate the amount a contract employee is paid. Additional information on consolidated billing is found in Chapter 6 of the Medicare Claims Processing Manual [PDF].
What is reasonable and necessary for the treatment of the resident's condition?
the services must be reasonable and necessary for the treatment of the resident's condition; this includes the requirement that the amount, frequency, and duration of the services must be reasonable and they must be furnished by qualified personnel.
Does Medicare cover student supervision?
Under Medicare, student supervision requirements vary by practice setting and whether the services are covered under Part A or Part B of the Medicare benefit. For example, Medicare is explicit that student services under Part B require 100% direct supervision of the licensed SLP.
Does MDS score count toward therapy minutes?
Time spent on MDS assessment does not count toward therapy minutes. A full description of how to score the MDS 3.0 is on CMS' website. The MDS places a patient into a diagnostic category and the SNF receives a lump sum payment based on that category for all of the services the patient requires.