Normally, Medicare does not cover routine vision correction, but Medicare does cover eyeglasses, contact lenses, and intraocular lenses following surgery to treat cataracts. If you require eyeglasses, Medicare Part B only provides coverage for standard frames.
Does Medicare pay for new frames for eyeglasses?
The eyeglasses must have standard frames and come from a Medicare-enrolled supplier, as Medicare will not pay for designer frames. A person can upgrade their frames if they are willing to pay the additional costs over the medically approved amount.
Does Medicare pay for corrective lenses?
Medicare doesn’t usually cover eyeglasses or contact lenses. helps pay for corrective lenses if you have cataract surgery to implant an intraocular lens. Corrective lenses include one pair of eyeglasses with standard frames or one set of contact lenses. You pay 100% for non-covered services, including most eyeglasses or contact lenses.
What is Medicare and how does it work?
Medicare is a public and federal health insurance program for Americans over the age of 65 and for certain other individuals who qualify for coverage. Medicare is funded entirely by the federal government through the Social Security Administration. The funding comes from taxes that workers in the U.S. pay into Social Security.
How much does Medicare pay for eye exams?
You’ll pay 20 percent of the Medicare-approved amount, including the deductible or any copayments in a hospital outpatient setting. Under Medicare Part B, you can receive up to 80 percent coverage for glaucoma eye exams if you’re at high risk for glaucoma, an eye disease that can cause blindness.
Do Medicare pay for glasses?
Generally, Original Medicare (Parts A & B) will not help pay for prescription sunglasses, contact lenses or eyeglasses. However, eyeglasses or other corrective lenses may be covered in cases where they are deemed “medically necessary,” such as after cataract surgery.
Does Medicare cover dry eye treatment?
If you are having a medical eye problem such as blepharitis or dry eye syndrome, Medicare will pay for any and all necessary medical visits to treat the problem.
Which IOL is covered by Medicare?
monofocal lensNote: The conventional intraocular lens (IOL) covered by Medicare is typically a monofocal lens. Other advanced lens types, such as a toric lens for astigmatism, Lifestyle Lens (multifocal or accommodating lens, or enVista™ lens may have out-of-pocket expenses.
What things will Medicare pay for?
What Part A covers. Medicare Part A hospital insurance covers inpatient hospital care, skilled nursing facility, hospice, lab tests, surgery, home health care.
How do people afford Xiidra on Medicare?
Here are some ways that may lower the cost of your Xiidra prescription.Instead of Medicare, Use a Coupon. If your Medicare co-pay is higher than $637.01, you can save money by using a GoodRx coupon instead. ... Manufacturer Coupon. Pay as little as $0 per prescription with insurance. ... Patient Assistance Program from Novartis.
Does Medicare pay for Restasis?
It is covered by most Medicare and insurance plans, but some pharmacy coupons or cash prices may be lower. Restasis (Cyclosporine) is used to increase tear production in patients who have dry eye due to eye inflammation.
What is the Medicare approved amount for eyeglasses after cataract surgery?
Since surgeons generally perform cataract surgery on an outpatient basis, it falls under Medicare Part B. This covers certain post-surgical costs. Usually, Medicare pays 80% of the total surgical cost, consisting of the procedure itself and the facility charges. Medicare does not normally cover prescription glasses.
Does Medicare pay for lens implants?
Medicare covers cataract surgery that involves intraocular lens implants, which are small clear disks that help your eyes focus. Although Medicare covers basic lens implants, it does not cover more advanced implants. If your provider recommends more advanced lens implants, you may have to pay some or all of the cost.
Are PanOptix lens covered by Medicare?
Medicare will pay for what it considers medically necessary cataract surgery. This means that Medicare will pay for the medical part of cataract surgery and a monofocal IOL. The cost of a specialized multifocal or trifocal lens (such as PanOptix) isn't covered.
Does Medicare pay for everything?
Original Medicare (Parts A & B) covers many medical and hospital services. But it doesn't cover everything.
Does Medicare pay 100 percent of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
Which type of care is not covered by Medicare?
Non-medical services, including a private hospital room, hospital television and telephone, canceled or missed appointments, and copies of x-rays. Most non-emergency transportation, including ambulette services. Certain preventive services, including routine foot care.
What percentage of corrective lenses are paid for by Medicare?
Any other insurance you may have in addition to Medicare. Whether the doctor and facility accept Medicare. You will pay 20 percent of the cost of your corrective lenses based on the Medicare-approved amount.
How often do eyeglasses need to be paid for?
Many Medicaid programs will pay for a new pair of prescription eyeglasses every five years. Contact your local program to determine eligibility and to apply.
Does Medicare pay for glasses?
Medicare does not pay for prescription eyeglasses or contact lenses. ( Learn More) Medicare Part B can provide coverage for one pair of prescription eyeglasses after you have cataract surgery, however. ( Learn More) If you have a supplemental Medicare Advantage plan, this can help you pay for glasses and provide some vision insurance coverage.
Does Medicare cover vision?
Medicare & Vision Coverage. Original Medicare, which includes Medicare Part A and Medicare Part B, does not offer coverage for vision services. The following are not covered: Prescription eyewear, including eyeglasses, are not paid for by original Medicare. Medicare can offer coverage for vision screenings for people at risk for glaucoma ...
Does Medicare pay for corrective lenses?
Medicare will only pay for corrective lenses from a supplier that is currently enrolled in Medicare. You can receive one pair of standard frames, and upgraded frames will cost extra.
Does Medicare cover cataract surgery?
Medicare can offer coverage for vision screenings for people at risk for glaucoma or diabetic retinopathy. Medicare also covers the cost of cataract surgery. Medigap, which is supplemental insurance to help cover costs that original Medicare does not cover, also does not provide any vision benefit coverage, including coverage for eyeglasses.
Why is Medicare important?
Medicare reaches many people in the U.S., but it is only useful if those enrollees get good health care and have good access to physicians, treatments, procedures, hospitals, and other services.
What percentage of Medicare patients accept new patients?
While most physicians, 91 percent , accept new Medicare patients, there is a big gap in mental health.
Why is Medicare so confusing?
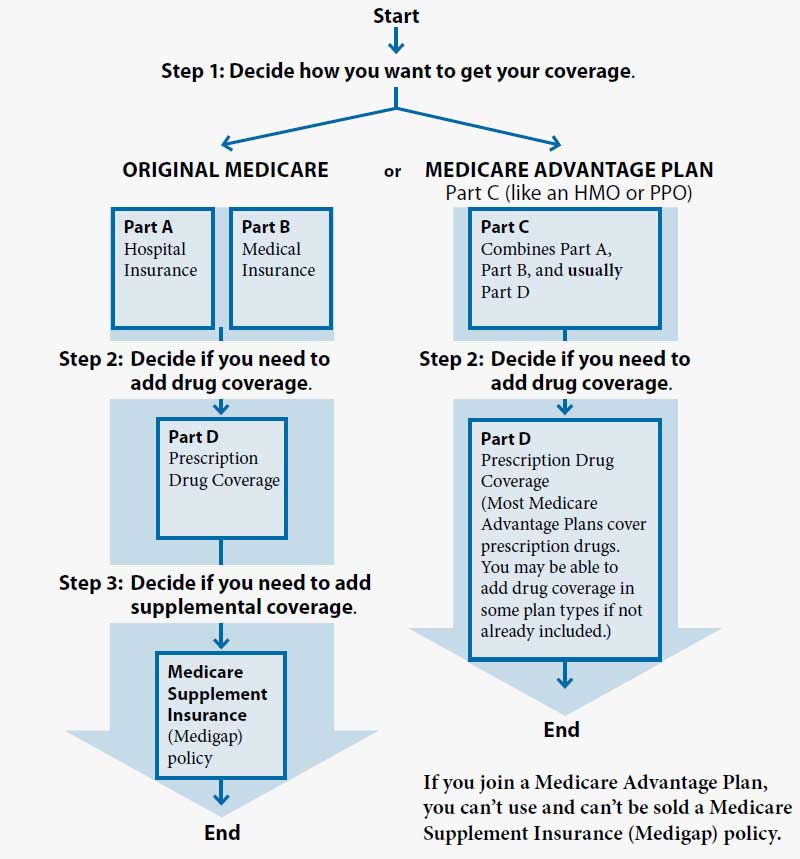
Medicare can be very confusing because of a complicated set of rules and coverage benefits and also because the program includes several different parts as well as the option to choose a private health care plan.
What is Medicare insurance?
What is Medicare? Medicare is a public and federal health insurance program for Americans over the age of 65 and for certain other individuals who qualify for coverage. Medicare is funded entirely by the federal government through the Social Security Administration.
What to know before enrolling in Medicare?
Before you enroll in a Medicare program, make sure you understand what all your options are and have taken the time to weigh the benefits of each against your needs. It is also important to ensure you choose plans and parts that will provide you with good access and care from the professionals you want to see.
What is the first choice for Medicare?
The first choice is between going with the original program, Parts A and B, or to choose a private plan through Part C.
How many people are on Medicare in 2017?
Most of these alternatives are HMOs, or health maintenance organizations. In 2017 there were more than 57 million Americans enrolled in Medicare. About one-third of those chose a private insurance plan, a number that has been growing since 2004.
How often can I get glasses on Medicaid?
There are limitations on how frequently an individual can obtain glasses, such as one pair a year, two pairs over 5 years or one pair over a lifetime. Every state Medicaid program offers a unique coverage program for eyeglasses, some require co-payments, while others pay the entire cost of the glasses with standard frames.
Do you have to replace glasses if they are stolen?
Some states offer a replacement plan for eyeglasses that are lost, stolen or broken, while others do not . Some states require that glasses be purchased from a vendor that agrees to a lowered cost through a volume contract.
Does Medicaid pay for glasses?
In some states, Medicaid only pays for a pair of glasses or contact lenses after cataract surgery. Depending on the state in which the participant is a member of Medicaid, the amount of glasses and the basis for need may vary, as documented by the Kaiser Family Foundation.
Which Eye Exams Does Medicare Cover?
In general, Original Medicare doesn’t cover routine eye exams for eyeglasses or contact lenses; however, there are some exceptions to this rule because Medicare can provide coverage for eye exams and vision care if an individual has diabetes, glaucoma, macular degeneration, or has undergone cataract surgery.
What Parts of Medicare Cover Eye Exams?
Although Original Medicare doesn’t cover eye exams, other parts of Medicare may be able to help pick up the cost for medically necessary services for vision conditions related to diabetes, glaucoma or macular degeneration.
What Do Eye Exams Cost With Medicare?
As mentioned, Medicare generally doesn’t cover routine eye exams, but there are exceptions for high-risk patients.
Does Medicare Cover Vision?
In a nutshell, Original Medicare doesn’t cover routine eye exams. However, under certain circumstances and conditions, Medicare can cover certain types of vision care. For example, Medicare Part B covers medically necessary screenings and eye exams for high-risk individuals with glaucoma, diabetes, or macular degeneration conditions.
Does Medicare Cover Glasses?
Medicare doesn’t usually cover eyeglasses or contacts, so you’d have to pay 100 percent of the cost — with the exception of certain eye conditions. In some cases, Medicare Part B can help you pay for corrective lenses if you’ve undergone cataract surgery to implant an intraocular lens.
Does Medicare Cover Eye Surgery?
Although Medicare doesn’t cover vision, hearing, or dental procedures, there are certain exceptions. For instance, if you require eye surgery or have a chronic eye condition that puts you at high risk, Medicare can cover cataract surgery or exams for high-risk patients with diabetes.
Eye Doctors That Accept Medicare
If you’re looking for an eye doctor that accepts Medicare, visit Medicare’s official website and click on the “Find Care Providers” link and use the lookup tool to search for keywords, providers, specialty, and location.
Does Medicare cover glasses after second eye surgery?
What actually happens is that Medicare covers just one pair of glasses or contacts after the second surgery, says Tracy Holt, MHR, COPC, transformational services account manager for Eye Care Leaders.
Does Medicare cover eyeglasses?
Medicare will rarely cover tint, oversize lenses, A/R coating, polycarbonate, or high index, she adds. So does Medicare also pay for the eye exam? No. Medicare does not cover routine eye exams/refractions for eyeglasses or contact lenses.
Does Medicare cover cataract surgery?
Medicare Coverage of Post-Cataract Eyeglasses, Explained. You may already know this, but it’s worth emphasizing: Medicare does not cover refractions, eyeglasses, or contact lenses for beneficiaries. The exception is for post-cataract surgery or in cases when surgery results in the removal of the eye’s natural lens.
Can you collect from a patient for cataract eyewear?
You can collect directly from the patient for these items. To do that compliantly and to collect your full reimbursement, you’ll need to provide and have the patient sign an advance beneficiary notice of non-coverage (ABN) before you deliver the post-cataract eyewear. The ABN is CMS-required form, mandated by HIPAA.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B.
What percentage of Medicare payment does a supplier pay for assignment?
If your supplier accepts Assignment you pay 20% of the Medicare-approved amount, and the Part B Deductible applies. Medicare pays for different kinds of DME in different ways. Depending on the type of equipment:
What is Medicare assignment?
assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. you pay 20% of the. Medicare-Approved Amount.
Does Medicare cover DME equipment?
You may be able to choose whether to rent or buy the equipment. Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare.
What is the Medicare Part B copayment?
For Medicare Part B, this comes to 20%. Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
How much is Medicare Part B deductible in 2021?
Original Medicare. If a person gets coverage through Medicare Part B, they will need to meet the Medicare Part B annual deductible of $203 (in 2021), plus 20% of the Medicare-approved amount. They will also pay the Part B monthly premium, which is $148.50 in 2021.
Does Medicare cover eyeglasses?
Generally, Medicare does not cover the cost of eyeglasses or contact lenses, although coverage for some items may be available after certain types of cataract surgery. Some Medicare Advantage plans also offer vision care. Coverage for vision care may have associated costs, such as premiums, deductibles, copays, and coinsurance.
Does Medicare pay for designer frames?
The eyeglasses must have standard frames and come from a Medicare-enrolled supplier, as Medicare will not pay for designer frames. A person can upgrade their frames if they are willing to pay the additional costs over the medically approved amount. Learn more about original Medicare (parts A and B) here.
Does Medicare Advantage cover eye exams?
While Medicare Advantage plans must offer the same coverage as original Medicare, they often include additional benefits, such as hearing, dental, and vision care. The latter coverage may include eye exams and eyeglasses, although there may be out-of-pocket costs. Depending on the Advantage plan, a person may need to use in-network providers ...
Is Healthline Media a licensed insurance company?
Healthline Media does not transact the business of insurance in any manner and is not licensed as an insurance company or producer in any U.S . jurisdiction. Healthline Media does not recommend or endorse any third parties that may transact the business of insurance. Last medically reviewed on February 1, 2021.
Does Medicare Advantage have out-of-network costs?
However, they may include a monthly premium, deductibles, copays, and coinsurance. In addition, plans generally have out-of-pocket costs — both in-network and out-of-network.