Entities Responsible for Medicare Appeals by Level and Medicare Part
| Level of the Appeals Process | Medicare Parts A and B | Medicare Part C | Medicare Part D |
| Level 2 | QIC | Independent Review Entity | Independent Review Entity |
| Level 3 | Office of Medicare Hearings and Appeals | Office of Medicare Hearings and Appeals | Office of Medicare Hearings and Appeals |
| Level 4 | Medicare Appeals Council | Medicare Appeals Council | Medicare Appeals Council |
| Level 5 | Federal Court | Federal Court | Federal Court |
Where to get help in making a Medicare appeal?
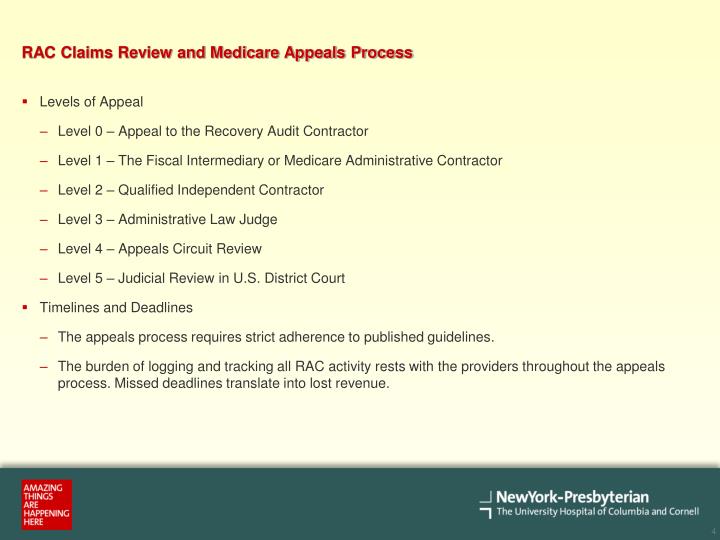
Original Medicare? The appeals process has 5 levels: Level 1: Redetermination by the Medicare Administrative Contractor (MAC) Level 2: Reconsideration by a Qualified Independent Contractor (QIC) Level 3: Decision by the Office of Medicare Hearings and Appeals (OMHA) Level 4: Review by the Medicare Appeals Council (Appeals Council)
Who can assist with a Medicare appeal?
Oct 10, 2012 · The five levels of Medicare Appeals are: Level 1: Redetermination (no minimum monetary limit) – You must appeal and request a redetermination in writing within 120 days of notification. If you do not request a redetermination within 30 days, Medicare will begin withholding moneys from your current accounts receivable (A/R), and could begin notifying the …
When can I file an appeal to a Medicare claim?
5 rows · There are five levels in the Medicare claims appeal process: Level 1: Your Health Plan. If ...
How to appeal a higher Medicare Part B premium?
Appealing Medicare Decisions Medicare FFS has 5 appeal process levels: Level 1 - MAC Redetermination Level 2 - Qualified Independent Contractor (QIC) Reconsideration Level 3 - Office of Medicare Hearings and Appeals (OMHA) Disposition Level 4 - Medicare Appeals Council (Council) Review Level 5 - U.S. District Court Judicial Review
What is the correct order of the levels of the Medicare appeal?
The levels are: First Level of Appeal: Redetermination by a Medicare Administrative Contractor (MAC) Second Level of Appeal: Reconsideration by a Qualified Independent Contractor (QIC) Third Level of Appeal: Decision by the Office of Medicare Hearings and Appeals (OMHA)
What is the first level of the Medicare appeals process?
redeterminationAppeal the claims decision. The first level of an appeal for Original Medicare is called a redetermination. A redetermination is performed by the same contractor that processed your Medicare claim.
How many levels are in the appeals process for a member?
The 5 Levels of the Appeals Process.
How many steps are there in the Medicare appeal process?
The appeals process has 5 levels. If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you'll get instructions in the decision letter on how to move to the next level of appeal.
What is the highest level of a Medicare Redetermination?
Medicare FFS has 5 appeal process levels:Level 1 - MAC Redetermination.Level 2 - Qualified Independent Contractor (QIC) Reconsideration.Level 3 - Office of Medicare Hearings and Appeals (OMHA) Disposition.Level 4 - Medicare Appeals Council (Council) Review.
How many levels of Medicare appeals are there?
five levelsThe Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
How do you win a Medicare appeal?
To increase your chance of success, you may want to try the following tips: Read denial letters carefully. Every denial letter should explain the reasons Medicare or an appeals board has denied your claim. If you don't understand the letter or the reasons, call 800-MEDICARE (800-633-4227) and ask for an explanation.Nov 12, 2020
How long does Medicare have to respond to an appeal?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 days. Payment request—60 days.
What are the four levels of appeals?
There are four stages to the appeal process — reconsideration, hearing, council, and court.
What to do if Medicare denies a claim?
If Medicare denies payment of the claim, it must be in writing and state the reason for the denial. This notice is called the Medicare Summary Notice (MSN) and is usually issued quarterly. Look for the reason for denial. coverage rule), it must be stated on the notice.
What is a second level appeal?
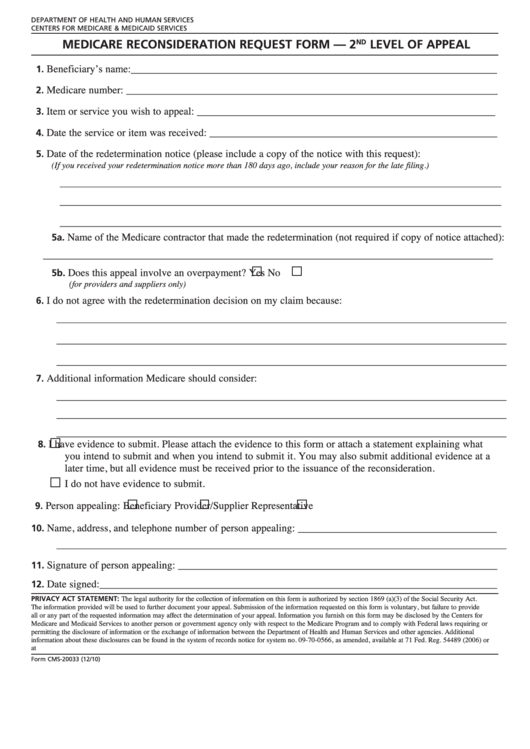
Second Level of Appeal: Reconsideration by a Qualified Independent Contractor. Any party to the redetermination that is dissatisfied with the decision may request a reconsideration.Apr 4, 2022
How do I appeal Part B Irmaa?
Even if you haven't experienced a life-changing event, you can still appeal an IRMAA. Request an appeal in writing by completing a request for reconsideration form. To get an appeal form, you can go into a nearby Social Security office, call 800-772-1213, or check the Social Security website.
What is level 3 in Medicare?
Level 3 is filing an appeal with the Administrative Law Judge (ALJ). ALJs hold hearings and issue decisions related to Medicare coverage determination that reach Level 3 of the Medicare claims appeal process. Level 4 is the Department Appeals Board (DAB) Review.
What is a redetermination?
A Redetermination is a completely new, critical re-examination of a disputed claim or charge. You should not request a Redetermination if you have identified a minor error or omission when you first filed your claim. In that case, you should request a "Reopening".
What happens if you reach level 5?
If you reach level 5, you can request a judicial review, and a decision will be made by the U.S. District Court, but only if a specific dollar amount remains in controversy following the council decision.
How long does it take to appeal a contractor's decision?
If you would like to request an appeal from the contractor, you must do so within 120 days from the date indicated on the initial determination receipt. Be sure to include any documentation that supports the overturn of the determination. You can expect a notice within 60 days; however, you may advance your appeal to the next level within 180 days if you disagree with their decision.
What is Medicare Recovery Audit Contractors?
Fraud, waste, and improper payments are a serious problem within the Medicare network. As a response, the U.S. Congress passed a resolution in 2003, creating the Medicare Recovery Audit Contractors (RAC) Program, designed to identify and reduce fraud. The results have been controversial: While billions of taxpayer dollars have been recovered, the program has also been the subject of industry criticism, litigation and even federal government hearings.
What is RAC in Medicare?
RACs use proprietary software and data mining to review Medicare billing records in search of coding and billing errors.
How long does it take to get an ALJ decision?
Within 60 days of the ALJ's decision or 90 days of no decision, you can request in writing a determination by the Appeals Council. Similar to level 3, there is a minimum amount requirement, determined annually.
What is the ABN for Medicare?
If you have Original Medicare and your doctor, other health care provider, or supplier thinks that Medicare probably (or certainly) won’t pay for items or services, he or she may give you a written notice called an ABN (Form CMS-R-131).
What to do if you are not satisfied with the IRE decision?
If you’re not satisfied with the IRE’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or, in certain circumstances, a review of the appeal record by an ALJ or an attorney adjudicator.
Does CMS exclude or deny benefits?
The Centers for Medicare & Medicaid Services (CMS) doesn’t exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, disability, sex, or age in admission to, participation in, or receipt of the services and benefits under any of its programs and activities, whether carried out by CMS directly or through a contractor or any other entity with which CMS arranges to carry out its programs and activities.
What is a QIC?
QIC is an independent contractor that didn’t take part in the level 1 decision. The QIC will review your request for a reconsideration and will make a decision.
How long does it take for an IRE to review a case?
They must get this information within 10 days after the date you get the notice telling you your case file has been sent to the IRE. The IRE’s address is on the notice.
Can you request a fast reconsideration?
If you disagree with the plan’s redetermination, you, your representative, or your doctor or other prescriber can request a standard or expedited (fast) reconsideration by an IRE. You can’t request a fast reconsideration if it’s an appeal about payment for a drug you already got.
What to do if you are not satisfied with QIC?
If you’re not satisfied with the QIC’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or , in certain circumstances, a review of the appeal record by an ALJ or attorney adjudicator.
What are the levels of Medicare appeal?
There are five levels in the Medicare claims appeal process: Level 1: Your Health Plan. If you disagree with a Medicare coverage decision, you may request your health plan to redetermine your claim. Level 2: An Independent Organization . If you disagree with the decision in Level 1 , you may request a reconsideration by an independent organization.
What is the OMHA level 3?
OMHA is responsible for Level 3 claims appeals. The entry point of the appeals process depends on the part of the Medicare program that covers the disputed benefit or whether the beneficiary is enrolled in a Medicare Advantage plan.
What does "I" mean in CMS?
In a 2019 Final Rule, CMS ended the requirement that appellants sign their appeal requests.In this booklet, “I” or “you” refers to patients, parties, and appellants active in an appeal.
What happens if you disagree with an ALJ?
If you disagree with the ALJ or attorney adjudicator decision, or you wish to escalate your appeal because the OMHA adjudication time frame passed, you may request a Council review. The Council is part of the HHS Departmental Appeals Board (DAB).
Can a patient transfer their appeal rights?
Patients may transfer their appeal rights to non-participating providers or suppliers who provide the items or services and don’t otherwise have appeal rights. To transfer appeal rights, the patient and non-participating provider or supplier must complete and sign the