Does Medicare require a copay?
A Medicare copayment is a fixed, out-of-pocket expense that you have to pay for each medical service or item — such as a prescription you receive if you have a Medicare Advantage plan or a Medicare prescription drug plan. Your Medicare plan pays the rest of the cost for the service. Copayments are different from coinsurance. If you have Original Medicare, you typically don’t …
How do Medicare copays and deductibles work?
Jan 20, 2022 · A copay is your share of a medical bill after the insurance provider has contributed its financial portion. Medicare copays (also called copayments) most often come in the form of a flat-fee and typically kick in after a deductible is met.
Does Medicare have copayments?
Nov 17, 2021 · A Medicare copay is the amount of money you're required to pay for a covered Medicare service or good. A copayment is typically a flat fee. Learn More About Medicare Join our email series to receive your free Medicare guide and the latest information about Medicare and Medicare Advantage. Sign me up!
What is copay or copayment for health insurance?
Jul 07, 2021 · Most copayment amounts are in the $10 to $45+ range, but the cost depends entirely on your plan. Certain parts of Medicare, such as Part C and Part D, charge copays for covered services and...

What happens if you don't buy Medicare?
If you don't buy it when you're first eligible, your monthly premium may go up 10%. (You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.) Part A costs if you have Original Medicare. Note.
How much does Medicare pay for outpatient therapy?
After your deductible is met, you typically pay 20% of the Medicare-approved amount for most doctor services (including most doctor services while you're a hospital inpatient), outpatient therapy, and Durable Medical Equipment (DME) Part C premium. The Part C monthly Premium varies by plan.
Does Medicare cover room and board?
Medicare doesn't cover room and board when you get hospice care in your home or another facility where you live (like a nursing home). $1,484 Deductible for each Benefit period . Days 1–60: $0 Coinsurance for each benefit period. Days 61–90: $371 coinsurance per day of each benefit period.
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
What is a copay in Medicare?
A copay is your share of a medical bill after the insurance provider has contributed its financial portion. Medicare copays (also called copayments) most often come in the form of a flat-fee and typically kick in after a deductible is met. A deductible is the amount you must pay out of pocket before the benefits of the health insurance policy begin ...
How much is Medicare Part A 2021?
The Medicare Part A deductible in 2021 is $1,484 per benefit period. You must meet this deductible before Medicare pays for any Part A services in each benefit period. Medicare Part A benefit periods are based on how long you've been discharged from the hospital.
Does Medicare cover out of pocket costs?
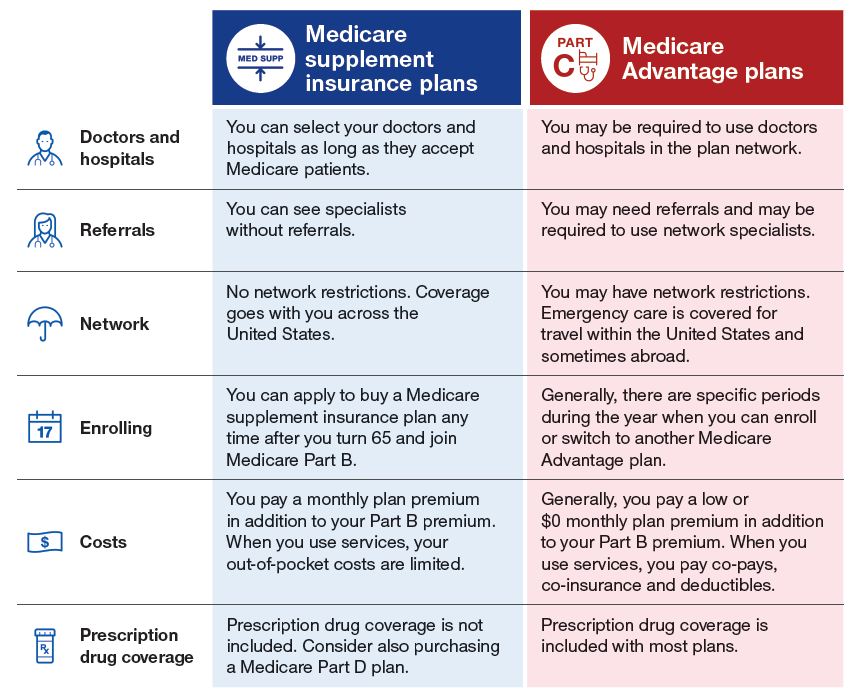
There is one way that many Medicare enrollees get help covering their Medicare out-of-pocket costs. Medigap insurance plans are a form of private health insurance that help supplement your Original Medicare coverage. You pay a premium to a private insurance company for enrollment in a Medigap plan, and the Medigap insurance helps pay ...
What is Medicare approved amount?
The Medicare-approved amount is the maximum amount that a doctor or other health care provider can be paid by Medicare. Some screenings and other preventive services covered by Part B do not require any Medicare copays or coinsurance.
How much is Medicare Part B deductible for 2021?
The Medicare Part B deductible in 2021 is $203 per year. You must meet this deductible before Medicare pays for any Part B services. Unlike the Part A deductible, Part B only requires you to pay one deductible per year, no matter how often you see the doctor. After your Part B deductible is met, you typically pay 20 percent ...
What percentage of Medicare deductible is paid?
After your Part B deductible is met, you typically pay 20 percent of the Medicare-approved amount for most doctor services. This 20 percent is known as your Medicare Part B coinsurance (mentioned in the section above).
How much is the deductible for Medicare 2021?
If you became eligible for Medicare. + Read more. 1 Plans F and G offer high-deductible plans that each have an annual deductible of $2,370 in 2021. Once the annual deductible is met, the plan pays 100% of covered services for the rest of the year.
What are the benefits of Medicare Advantage?
Many are likely drawn to the unique benefits of Medicare Advantage, as compared with Original Medicare: 1 Medicare Advantage plans may often include additional benefits for prescription drugs, dental care, and vision care. 2 The average premium for a Medicare Advantage plan that offers prescription drug coverage is $33.57 per month in 2021. 2 Some plans may not have a monthly premium, and some may even help pay you back for your Medicare Part B premium. 3 Medicare Advantage, unlike Original Medicare, comes with an out-of-pocket limit, which means your out-of-pocket spending will be capped. 4 While plans are offered by private insurers, you are still guaranteed the benefits of Original Medicare.
Who is Christian Worstell?
Christian Worstell is a licensed insurance agent and a Senior Staff Writer for MedicareAdvantage.com. He is passionate about helping people navigate the complexities of Medicare and understand their coverage options. .. Read full bio
What is Medicare for 65?
Cost. Eligibility. Enrollment. Takeaway. Medicare is a government-funded health insurance option for Americans age 65 and older and individuals with certain qualifying disabilities or health conditions. Medicare beneficiaries are responsible for out-of-pocket costs such as copayments, or copays for certain services and prescription drugs.
How much is Medicare Part A 2021?
You’ll have the following costs for your Part A services in 2021: monthly premium, which varies from $0 up to $471. per benefits period deductible, which is $1,484. coinsurance for inpatient visits, which starts at $0 and increases with the length of the stay.
When is Medicare enrollment period?
If you miss your initial enrollment period or want to change or enroll in a different Medicare plan, here are the additional enrollment periods: General and Medicare Advantage enrollment: from January 1 to March 31.
Does Medicare Part A have coinsurance?
coinsurance for inpatient visits, which starts at $0 and increases with the length of the stay. These are the only costs associated with Medicare Part A, meaning that you will not owe a copay for Part A services.
What is a copay in Medicare?
A copayment, or copay, is a fixed amount of money that you pay out-of-pocket for a specific service. Copays generally apply to doctor visits, specialist visits, and prescription drug refills. Most copayment amounts are in ...
How much is coinsurance for Medicare?
These coinsurance amounts generally take the place of copays you might otherwise owe for services under original Medicare and include: $0 to $742+ daily coinsurance for Part A, depending on the length of your hospital stay. 20 percent coinsurance of the Medicare-approved amount for services for Part B.
When is Medicare open enrollment?
General and Medicare Advantage enrollment: from January 1 to March 31. Open enrollment: from October 15 to December 7. Special enrollment: a number of months depending on your circumstances. The initial enrollment period is the time in which you can enroll into Medicare parts A and B.
Does Medicare Advantage cover physicals?
All of our Medicare Advantage plans cover an annual routine physical examination with no cost share. The exam includes a comprehensive physical exam and evaluates the status of chronic diseases.
Does Medicare cover syphilis?
Medicare covers STI screening for chlamydia, gonorrhea, syphilis or Hepatitis B when tests are ordered by a primary care provider for members who are pregnant or have an increased risk for an STI. These tests are covered once every year or at certain times during pregnancy.
Copay vs. Coinsurance
Copays and coinsurance fees are often discussed when you hear about your medical insurance plan. Most of the time, a copay or copayment refers to a single fee that you will have to pay when you receive health care.
Does Medicare Use Copays?
Yes and no. Importantly, Part B of Medicare never uses copays. Part B has a deductible of $203per benefit period, and after this, you will pay 20 percent of your costs, which is your coinsurance.
Mental Health Services -- The Exception
Mental health services are the one regular exception to this rule. There may be some instances in which you don't have to pay a copay for these services, but most of the time that is the arrangement that Medicare will use. Make sure to check the details with the office you are dealing with and with Medicare.
What About Part A?
Medicare Part A does not technically use a copayment, but the fees are very similar to what most people associate with copays. Part A hospital insurance uses a so-called coinsurance fee, but this fee is not percentage-based and is pre-set with a few tiers depending on the length of your skilled nursing facility or hospital stay.
Copays with Medicare Advantage
When it comes to copays, Medicare Advantage is a whole other story. Medicare Advantage, or Part C, refers to a way of receiving your Medicare coverage through a private health insurance company. If you have a Medicare Advantage plan, many of the associated fees will be set by that insurance company, rather than Medicare.
How do Part D Prescription Drug Plans Fit In?
Although Part D plans usually won't apply to your actual doctor visit, they are still very relevant to the process. If your doctor prescribes you medication during your visit, it will usually be covered by a Part D plan.
Can Medigap Plans Help?
Medigap plans, or Medicare Supplement Plans, are plans that cover some of your Medicare out-of-pocket costs. With these plans, you will only pay a monthly premium, with no other out-of-pocket costs. As an example, these plans can cover your Part B coinsurance, and cover many other out-of-pocket fee categories.
What is the PACE program?
PACE. PACE (Program of All-inclusive Care for the Elderly) is a Medicare/Medicaid program that helps people meet health care needs in the community.
What is SSI benefits?
A monthly benefit paid by Social Security. SSI is for people with limited income and resources who are disabled, blind, or age 65 or older. SSI benefits aren't the same as Social Security retirement or disability benefits.
What is an inpatient hospital?
Inpatient hospital care. You’re admitted to the hospital as an inpatient after an official doctor’s order, which says you need inpatient hospital care to treat your illness or injury. The hospital accepts Medicare.
What is general nursing?
General nursing. Drugs as part of your inpatient treatment (including methadone to treat an opioid use disorder) Other hospital services and supplies as part of your inpatient treatment.
What is a critical access hospital?
Critical access hospitals. Inpatient rehabilitation facilities. Inpatient psychiatric facilities. Long-term care hospitals. Inpatient care as part of a qualifying clinical research study. If you also have Part B, it generally covers 80% of the Medicare-approved amount for doctor’s services you get while you’re in a hospital.
Do you have to pay copay for extended care?
Geriatric and extended care copay rates. You won't need to pay a copay for geriatric care (also called elder care) or extended care ( also called long-term care) for the first 21 days of care in a 12-month period. Starting on the 22nd day of care, we'll base your copays on 2 factors:
What is the service connected rating for free medications?
If you have a service-connected rating of 40% or less and your income falls at or below the national income limits for receiving free medications, you may want to provide your income information to us to determine if you qualify for free medications.
How many times can you use urgent care?
There's no limit to how many times you can use urgent care. To be eligible for urgent care benefits, including through our network of approved community providers, you must: Be enrolled in the VA health care system, and. Have received care from us within the past 24 months (2 years)
What is VA claim exam?
VA claim exams (also called compensation and pension, or C&P, exams) Care related to a VA-rated service-connected disability. Care for cancer of head or neck caused by nose or throat radium treatments received while in the military. Individual or group programs to help you quit smoking or lose weight.
How to find out if you qualify for a reduced inpatient copay?
To find out if you qualify for a reduced inpatient copay rate, call us toll-free at 877-222-8387.