Medicare Guidelines: Eligibility, Costs, and Services
- You can qualify for Medicare by turning 65 years old or if you have a disability or diagnosis of end stage renal disease (ESRD) or amyotrophic lateral sclerosis (ALS).
- Your costs for Medicare depend on your income, work history, and other factors.
- You can get help paying for Part B and Part D if you have a limited income; on the other hand, you’ll pay more if you have a higher income.
- Each service that Medicare covers has guidelines to follow to get coverage.
- Age. You'll become eligible for Medicare when you turn 65 years old. ...
- Disability. You'll be automatically enrolled in Medicare once you've received 24 months of SSDI at any age. ...
- ESRD or ALS.
What insurances follow Medicare guidelines?
People representing Medicare plans aren't allowed to:
- Come to your home uninvited to sell or endorse anything.
- Call you unless you’re already a member of the plan. ...
- Require you to speak to a sales agent to get information about the plan.
- Offer you cash (or gifts worth more than $15) to join their plan or give you free meals during a sales pitch for a Medicare health or drug plan.
What are the criteria to meet eligibility for Medicare?
- You have been receiving Social Security disability benefits for at least 24 months in a row
- You have Lou Gehrig’s disease (amyotrophic lateral sclerosis)
- You have permanent kidney failure requiring regular dialysis or a kidney transplant. This condition is called end-stage renal disease (ESRD).
What are the best options for Medicare?
Ranking the best medicare supplement plans of 2021
- Humana. Humana is one of the largest providers of healthcare and healthcare insurance in the country. ...
- Mutual of Omaha Medicare Supplement. Mutual of Omaha offers eight Medicare supplement plans that cover most out of pocket expenses most people will incur.
- United Medicare Advisors. ...
- Aetna Medicare Supplement. ...
- Cigna. ...
What are the rules for Medicare?
- Private practices
- Skilled nursing facilities
- Rehabilitation facilities
- Home health agencies providing therapy covered under Part B in the home of the beneficiary
- Hospital outpatient departments (including emergency)
What are the 3 requirements for Medicare?
Be age 65 or older; Be a U.S. resident; AND. Be either a U.S. citizen, OR. Be an alien who has been lawfully admitted for permanent residence and has been residing in the United States for 5 continuous years prior to the month of filing an application for Medicare.
At what income do you have to pay for Medicare?
Monthly Medicare Premiums for 2022Modified Adjusted Gross Income (MAGI)Part B monthly premium amountIndividuals with a MAGI above $170,000 and less than $500,000 Married couples with a MAGI above $340,000 and less than $750,000Standard premium + $374.205 more rows
What is the 60 day rule for Medicare?
A benefit period begins the day you are admitted to a hospital as an inpatient, or to a SNF, and ends the day you have been out of the hospital or SNF for 60 days in a row. After you meet your deductible, Original Medicare pays in full for days 1 to 60 that you are in a hospital.
What are the 3 types of Medicare and what do they provide?
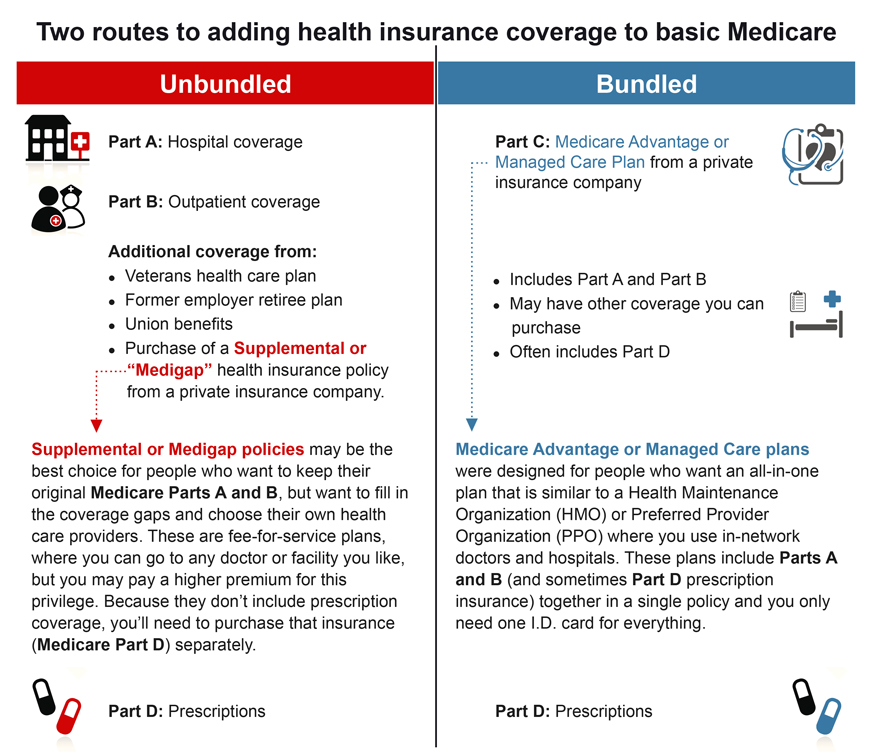
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
Does Social Security count as income for Medicare?
All types of Social Security income, whether taxable or not, received by a tax filer counts toward household income for eligibility purposes for both Medicaid and Marketplace financial assistance.
What are the income limits for Medicare 2021?
In 2021, the adjustments will kick in for individuals with modified adjusted gross income above $88,000; for married couples who file a joint tax return, that amount is $176,000. For Part D prescription drug coverage, the additional amounts range from $12.30 to $77.10 with the same income thresholds applied.
How do you count Medicare days?
A part of a day, including the day of admission and day on which a patient returns from leave of absence, counts as a full day. However, the day of discharge, death, or a day on which a patient begins a leave of absence is not counted as a day unless discharge or death occur on the day of admission.
What happens when you run out of Medicare days?
For days 21–100, Medicare pays all but a daily coinsurance for covered services. You pay a daily coinsurance. For days beyond 100, Medicare pays nothing. You pay the full cost for covered services.
Is there a lifetime limit on Medicare?
In general, there's no upper dollar limit on Medicare benefits. As long as you're using medical services that Medicare covers—and provided that they're medically necessary—you can continue to use as many as you need, regardless of how much they cost, in any given year or over the rest of your lifetime.
Whats the difference between Medicare Part A and B?
If you're wondering what Medicare Part A covers and what Part B covers: Medicare Part A generally helps pay your costs as a hospital inpatient. Medicare Part B may help pay for doctor visits, preventive services, lab tests, medical equipment and supplies, and more.
What will Medicare not pay for?
Generally, Original Medicare does not cover dental work and routine vision or hearing care. Original Medicare won't pay for routine dental care, visits, cleanings, fillings dentures or most tooth extractions. The same holds true for routine vision checks. Eyeglasses and contact lenses aren't generally covered.
What part of Medicare is free?
Part APart A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. coverage if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A." Most people get premium-free Part A.
How to Enroll in Medicare and When You Should Start Your Research Process
Getting older means making more decisions, from planning for your kids’ futures to mapping out your retirement years. One of the most important dec...
Who Is Eligible to Receive Medicare Benefits?
Two groups of people are eligible for Medicare benefits: adults aged 65 and older, and people under age 65 with certain disabilities. The program w...
When Should You Enroll For Medicare?
Just because you qualify for something doesn’t mean you need to sign up, right? Not always. In the case of Medicare, it’s actually better to sign u...
Can You Delay Medicare Enrollment Even If You Are Eligible?
The short answer here is yes, you can choose when to sign up for Medicare. Even if you get automatically enrolled, you can opt out of Part B since...
What About Medigap Plans?
Original Medicare covers a good portion of your care, but it’s not exhaustive. There’s a wide range of services that Parts A and B don’t cover, inc...
What is Medicare guidance document?
Medicare Coverage Guidance Documents. The Medicare Prescription Drug, Improvement, and Modernization Act of 2003 requires that the Secretary make available to the public the factors that are considered in making National Coverage Determinations (NCDs) of whether an item or service is reasonable and necessary.
What is CMS guidance?
To do this, CMS is producing guidance documents similar to those used by the U.S. Food and Drug Administration. These guidance documents give the public - particularly individuals or organizations that might request an NCD - detailed information on the NCD process and related evaluation and decision-making factors.
How old do you have to be to get medicare?
You can become eligible in these ways: Age. You’ll become eligible for Medicare when you turn 65 years old. You can enroll starting 3 months before your birth month. Your enrollment period lasts until 3 months after your birth month.
What is Medicare for 65?
Medicare is a federally funded health insurance program for people ages 65 and over and those who have certain medical conditions or disabilities. Medicare helps cover the costs of staying healthy and treating any conditions you might have. The rules for enrolling in Medicare are different depending on how you become eligible.
How much does Part A pay for skilled care?
Part A will pay for up to 100 days of skilled care in each benefit period. On days 1 through 20, your stay will be completely covered with no copayment. On days 21 through 100, you’ll pay a coinsurance amount of $176 a day in 2020. If you’ve used more than 100 days, you’ll pay the full cost.
How is Medicare funded?
Medicare is funded by taxpayer contributions to Social Security. When you work and pay into Social Security, you earn what is known as a Social Security work credit. Social Security work credits determine your eligibility for services like SSDI and premium-free Medicare Part A.
How long does Medicare enrollment last?
Your enrollment period lasts until 3 months after your birth month. If you miss this window, you may need to pay a late enrollment penalty. Disability. You’ll be automatically enrolled in Medicare once you’ve received 24 months of SSDI at any age.
What is a Part D plan?
Part D plans are stand-alone plans that cover only prescriptions. These plans are also provided through private insurance companies. Medigap. Medigap is also known as Medicare supplement insurance. Medigap plans help cover the out-of-pocket costs of Medicare, like deductibles, copayments, and coinsurance.
Does Medicare pay for physical therapy?
Physical therapy guidelines. Medicare will pay for medically necessary physical therapy under Part B coverage. The services need to be ordered by your doctor to treat a condition or prevent a condition from getting worse — for example, physical therapy to reduce pain or to help you regain mobility following a stroke.
Who is eligible to receive Medicare benefits?
Two groups of people are eligible for Medicare benefits: adults aged 65 and older, and people under age 65 with certain disabilities. The program was created in the 1960s to provide health insurance for senior citizens. Older Americans had trouble finding affordable coverage, which spurred the government to create a program specifically for this portion of the population. It’s an entitlement program in that the federal government finances it to some degree, but it’s also supported and financed directly by the very people who use it. You’re eligible for Medicare because you pay for it, in one way or another.
How long do you have to be a US citizen to qualify for Medicare?
To receive Medicare benefits, you must first: Be a U.S. citizen or legal resident of at least five (5) continuous years, and. Be entitled to receive Social Security benefits.
What About Medigap Plans?
Original Medicare covers a good portion of your care, but it’s not exhaustive. There’s a wide range of services that Parts A and B don’t cover, including dental and vision care. About a third of Medicare enrollees choose the private version of the program – Medicare Advantage – because it tends to cover more than its original counterpart. But if you like the flexibility of original Medicare and don’t need the benefits that Advantage affords, but you still want additional coverage to offset your out-of-pocket costs, then consider adding a Medigap supplemental policy to your plan.
How long do you have to sign up for Medicare before you turn 65?
And coverage will start…. Don’t have a disability and won’t be receiving Social Security or Railroad Retirement Board benefits for at least four months before you turn 65. Must sign up for Medicare benefits during your 7-month IEP.
When do you sign up for Medicare if you turn 65?
You turn 65 in June, but you choose not to sign up for Medicare during your IEP (which would run from March to September). In October, you decide that you would like Medicare coverage after all. Unfortunately, the next general enrollment period doesn’t start until January. You sign up for Parts A and B in January.
How long does it take to enroll in Medicare?
If you don’t get automatic enrollment (discussed below), then you must sign up for Medicare yourself, and you have seven full months to enroll.
When does Medicare open enrollment start?
You can also switch to Medicare Advantage (from original) or join a Part D drug plan during the Medicare annual open enrollment period, which runs from October 15 through December 7 each year. Eligibility for Medicare Advantage depends on enrollment in original Medicare.
When will Medicare open enrollment start?
If you have ESRD, you can join a Medicare Advantage Plan during Open Enrollment (October 15–December 7, 2020). Your plan coverage will start January 1, 2021. See page 59.
How often does Medicare cover colorectal cancer screening?
Medicare covers this screening test for colorectal cancer, in certain cases, once every 3 years. See
What is section 7 of the 79?
79 Section 7: Get help paying your health & drug costs
Does Medicare pay for mental health?
If you have a behavioral health condition (like depression, anxiety, or another mental health condition), Medicare may pay your provider to help manage that condition if they offer the Psychiatric Collaborative Care Model. This model is a set of integrated behavioral health services, including care management support that may include:
Does Medicare cover preventive care?
Medicare covers many preventive services at no cost to you. Ask your doctor or other health care provider which preventive services (like screenings, shots or vaccines, and yearly “Wellness” visits) you need. See pages 30–51 and look for to learn more about which preventive services Medicare covers.
Can you use Medigap from a former employer?
page 75) to learn more about Medigap. Or, you can use coverage from a former employer or union, or Medicaid.
Does Medicare cover cognitive impairment?
Medicare covers a cognitive assessment to help detect the earliest signs of cognitive impairment. Your doctor may perform this assessment during a routine visit. If you show signs of cognitive impairment, Medicare also covers a separate visit with your regular doctor or specialist to do a full review of your cognitive function, establish or confirm a diagnosis like dementia, including Alzheimer’s disease, and develop a care plan. See
When did Medicare start providing prescription drugs?
Since January 1, 2006, everyone with Medicare, regardless of income, health status, or prescription drug usage has had access to prescription drug coverage. For more information, you may wish to visit the Prescription Drug Coverage site.
How long do you have to be on disability to receive Social Security?
You have been entitled to Social Security or Railroad Retirement Board disability benefits for 24 months. ( Note: If you have Lou Gehrig's disease, your Medicare benefits begin the first month you get disability benefits.)
What is Medicare Advantage Policy?
Medicare Advantage Policy Guidelines are intended to ensure that coverage decisions are made accurately based on the code or codes that correctly describe the health care services provided.
What is UnitedHealthcare's Medicare Advantage Policy?
UnitedHealthcare has developed Medicare Advantage Policy Guidelines to assist us in administering health benefits. These Policy Guidelines are provided for informational purposes, and do not constitute medical advice.
What is a member specific benefit plan?
The member specific benefit plan document identifies which services are covered, which are excluded, and which are subject to limitations. In the event of a conflict, the member specific benefit plan document supersedes the Medicare Advantage Policy Guidelines.
Where is the provider service number on a health card?
For questions, please contact your local Network Management representative or call the Provider Services number on the back of the member’s health ID card.
Do you have to consult your physician before making a decision about medical care?
Members should always consult their physician before making any decisions about medical care. Benefit coverage for health services is determined by the member specific benefit plan document* and applicable laws that may require coverage for a specific service.