• In the discharge plan, include a list of HHAs or SNFs available to the patient that participate in Medicare, and serve the geographic area in which patient resides. SNFs must serve the geographic area requested by patient; HHAs must request to be listed by the hospital.
Full Answer
Who can request a discharge plan for a patient?
Sep 26, 2019 · The Centers for Medicare & Medicaid Services (CMS) today issued a final rule that empowers patients to make informed decisions about their care as they are discharged from acute care into post-acute care (PAC), a process called “discharge planning.”. In addition to improving quality by improving these care transitions, today’s rule supports CMS’ …
What should be on your discharge planning checklist?
More information for people with Medicare. If you need help choosing a home health agency or nursing home: • Talk to the staff. • Visit . Medicare.gov. to compare the quality of home health agencies, nursing homes, dialysis facilities, inpatient rehabilitation facilities, and hospitals in your area. • Call . 1-800-MEDICARE (1-800-633-4227).
Are Medicare beneficiaries given timely notice of reasons for discharge?
Apr 03, 2019 · Simplifying Documentation Requirements. As part of our Patients over Paperwork Initiative, Medicare is simplifying documentation requirements so that you spend less time on paperwork, allowing you to focus more on your patients and less on confusing and time-consuming claims documentation. We've made some important changes already.
What should a final resident discharge summary contain?
Discharge from the Hospital Setting. Effective July 1, 2007, Medicare participating hospitals must deliver valid, written notice, using the “Important Message from Medicare” (IM) (site visited May 15, 2015). This notice is to explain a patient’s rights …
What documentation is needed for a discharge summary?
Does Medicare require a discharge summary?
After all the reading I've done, it appears that Medicare does not require discharge summaries. That doesn't mean you shouldn't do it. Keep reading for why writing a discharge summary, even if it isn't required, could save you a lot of money and even your professional license.Jan 27, 2020
What is the criteria for patient discharge?
What are the components of a discharge plan?
What is discharge planning PDF?
When should a discharge summary be completed?
What is the criteria for the patients discharge from PACU to the ward?
What are the determining factors for a patient to be discharged from the PACU?
- Consciousness level. Patients should respond to verbal stimulation, be able to answer questions appropriately and to be oriented to their surroundings. ...
- Respiration. ...
- Circulation. ...
- Pain control. ...
- Nausea and vomiting. ...
- Fluid balance. ...
- Heat conservation. ...
- Wound site, drains and dressings.
What is a discharge process?
What is the most important part of discharge planning?
What is discharge summary sheet?
What is effective discharge planning?
What is discharge notice?
A notice is any written or oral discussion of one’s rights and protections, particularly with respect to costs and services available in a proposed care setting. It is therefore important that notice is:
Who should contact if a Medicare discharge is too soon?
Medicare beneficiaries and their advocates who question the appropriateness of a proposed discharge from a Medicare hospital, whether the discharge is too soon or whether necessary post-hospital services have been arranged, should contact the local Quality Improvement Organization ( QIO) and file a complaint.
How to contact Medicare for Elder Care?
In addition, contact the Medicare program’s information line: 1-800-MEDICARE (1-800-633-4227) (TTY: 1-877-486-2048 for the hearing impaired).
What information is useful for Medicare beneficiaries and their advocates?
The following information for Medicare beneficiaries and their advocates is useful in challenging a discharge or reduction in services in the hospital, skilled nursing, home health, or hospice care setting: Carefully read all documents that purport to explain Medicare rights.
When a hospital determines that inpatient care is no longer necessary, the Medicare beneficiary has the right to request an
When a hospital (with physician concurrence) determines that inpatient care is no longer necessary, the Medicare beneficiary has the right to request an expedited QIO review. The CMS guidelines provide that the appeal for expedited review must be made before the beneficiary leaves the hospital.
How long is an outpatient observation in Medicare?
Medicare beneficiaries throughout the country are experiencing the phenomenon of being in a bed in a Medicare-participating hospital for multiple days, sometimes over 14 days, only to find out that their stay has been classified by the hospital as outpatient observation. In some instances, the beneficiaries’ physicians order their admission, but the hospital retroactively reverses the decision. As a consequence of the classification of a hospital stay as outpatient observation (or of the reclassification of a hospital stay from inpatient care, covered by Medicare Part A, to outpatient care, covered by Medicare Part B), beneficiaries are charged for various services they received in the acute care hospital, including their prescription medications. They are also charged for their entire subsequent SNF stay, having never satisfied the statutory three-day inpatient hospital stay requirement, as the entire hospital stay is considered outpatient observation. The observation status issue has been challenged in Bagnall v. Sebelius (No. 3:11-cv-01703, D. Conn), filed on November 3, 2011. Litigation is ongoing. For updates, see https://www.medicareadvocacy.org/bagnall-v-sebelius-no-11-1703-d-conn-filed-november-3-2011/ (site visited May 27, 2015).
When did the Center for Medicare Advocacy sue?
On November 3, 2011, the Center for Medicare Advocacy, and co-counsel National Senior Citizens Law Center, filed a lawsuit on behalf of seven individual plaintiffs from Connecticut, Massachusetts, and Texas who represent a nationwide class of people harmed by the illegal “observation status” policy and practice.
What are the guidelines for medical records?
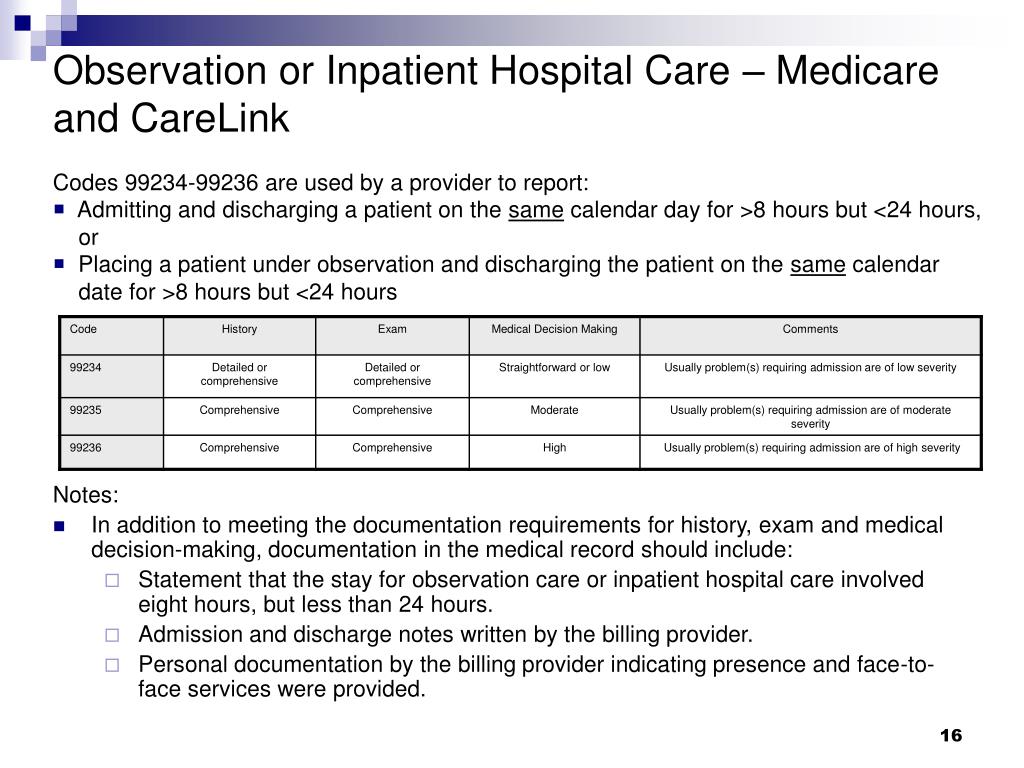
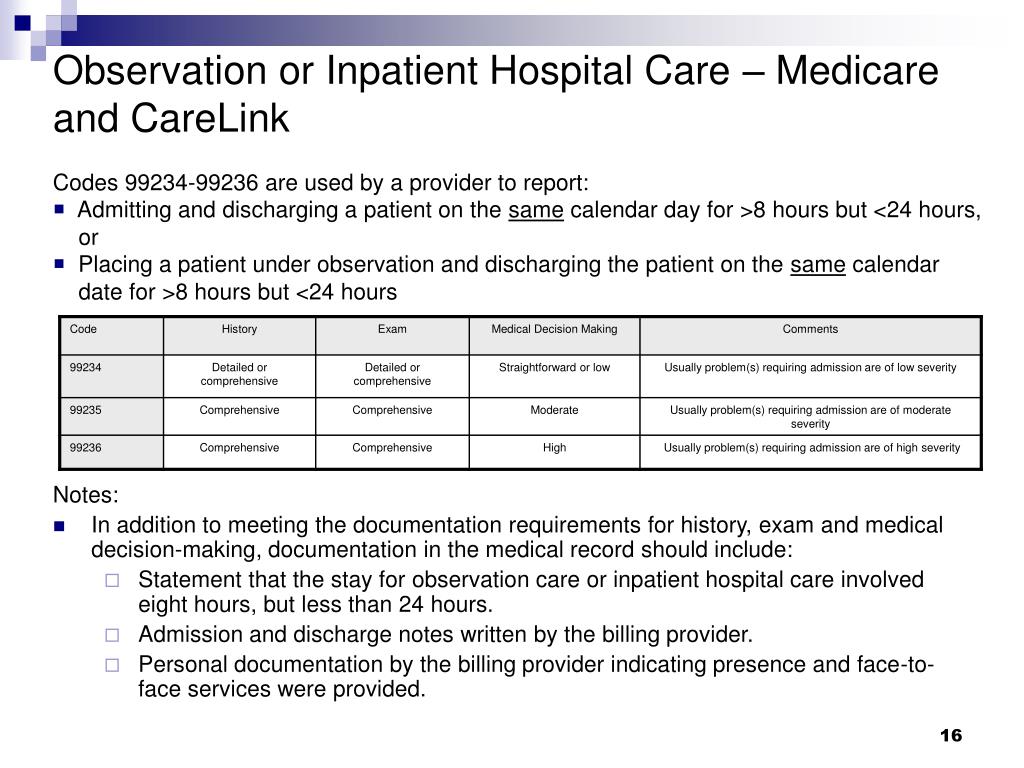
General Documentation Guidelines. All medical record entries must be legible, complete, dated, timed, and authenticated in written or electronic form by the person responsible for providing or evaluating the service provided. The following list may be used when submitting documentation to Medicare.
Why is medical documentation important?
Documentation is required to record pertinent facts, findings and observations about an individual’s health history, including past and present illnesses, examinations, tests, treatments and outcomes. The medical record chronologically documents the care of the patient and is an important element contributing to high-quality care.
What is required to record health history?
Documentation. Documentation is required to record pertinent facts, findings and observations about an individual’s health history, including past and present illnesses, examinations, tests, treatments and outcomes.
Why is it important to document medical history?
Documentation. Documentation is required to record pertinent facts, findings and observations about an individual’s health history, including past and present illnesses, examinations, tests, treatments and outcomes. The medical record chronologically documents the care of the patient and is an important element contributing to high-quality care.
Why is medical record important?
The medical record chronologically documents the care of the patient and is an important element contributing to high-quality care. An appropriately documented medical record can reduce many of the challenges associated with claims processing and may serve as a legal document to verify the care provided, if necessary.
When should a physician report a level 5 office visit?
When a physician performs a visit or consultation that meets the definition of a Level 5 office visit or consultation several days prior to an admission and on the day of admission performs less than a comprehensive history and physical, he or she should report the office visit or consultation that reflects the services furnished and also report the lowest level initial hospital care code (i.e., code 99221) for the initial hospital admission. Contractors pay the office visit as billed and the Level 1 initial hospital care code.
Does the revision date apply to red italicized material?
Disclaimer for manual changes only: The revision date and transmittal number apply only to red italicized material. Any other material was previously published and remains unchanged. However, if this revision contains a table of contents, you will receive the new/revised information only, and not the entire table of contents.
When will CMS release discharge planning rules?
In 2019, CMS provided the elements of the proposed rules that would be adopted in November 2019.
How much does CMS spend on discharge planning?
Facilities that must adhere to the new rules include: • Critical access hospitals. CMS estimates that hospitals and home health agencies will spend $215 million per year to comply with the discharge planning changes, and will incur an additional $46.5 million in one-time costs.
What are the conditions of participation in Medicare?
The Conditions of Participation. The current federal standards for hospitals participating in the Medicare and Medicaid programs are presented in the Code of Federal Regulations (CFR) as 13 Conditions of Participation (CoPs). The original CoPs were written in 1983, and were developed to ensure quality standards in hospitals ...
When will CMS rule changes be made?
In 2019, CMS provided the elements of the proposed rules that would be adopted in November 2019. While the selected rules may not be as dramatic as the entire set of proposed rules, some of the new rules will require changes in how case management departments perform some components of discharge planning.
Is discharge planning a process or outcome?
CMS describes discharge planning as a process, not an outcome.1 Because it is a process, case management professionals should always follow the CoP for discharge planning, as well as their department’s policies and procedures. In this way, one can ensure one’s practice and department are compliant.
What is discharge planning?
In other words, discharge planning allows for a smooth move for the patient across the continuum, and at all transition points. As discharge planners, case management professionals are responsible for ensuring that the patient’s discharge is timely, safe, and appropriate.
Do hospital policies and procedures have to be specified in writing?
• Patients who require discharge planning evaluation must be identified early in the hospital stay. Evaluations also should be provided to other patients at the request of the patient, the person acting on the patient’s behalf, or the physician.