Covered Preventive Services: One time “Welcome to Medicare” preventive visit Glaucoma tests Bone mass measurements Sexually transmitted infection testing Yearly wellness visit Flu, Hepatitis B and Pneumococcal shots
Full Answer
What preventive care screenings does Medicare cover?
Medicare Part B (Medical Insurance) covers: Abdominal aortic aneurysm screening; Alcohol misuse screenings & counseling; Bone mass measurements (bone density) Cardiovascular disease screenings; Cardiovascular disease (behavioral therapy) Cervical & vaginal cancer screening; Colorectal cancer screenings Multi-target stool DNA tests; Screening barium enemas
When do the changes to Medicare start?
Sep 12, 2018 · Preventive services covered by Medicare Medicare covers a variety of preventive services and screenings to help beneficiaries stay healthy. Here is a list of Medicare preventive services covered by Medicare Part B: Abdominal aortic aneurysm screenings; Alcohol misuse screenings and counseling; Bone mass measurements; Breast cancer screening and …
How much will Medicare Cost you in 2020?
Jan 04, 2021 · Medicare covers many preventive services, including your yearly “Wellness” visit and screenings for breast cancer, diabetes, and heart disease. Most of these services are provided at no cost to you. Preventive services are key to maintaining your wellbeing; they keep you from getting sick and help find health problems early.
When does Medicare open enrollment start?
Nov 23, 2021 · Depression screening, once a year; Diabetes screening, up to twice a year for people at high risk of diabetes; Flu shots; Hepatitis B shots, for those at medium or high risk; Hepatitis C screening test, for those at high risk and with a doctor’s order; HIV screening, every 12 months for those under age 65. For those 65 and older, screening is only covered for high-risk …

What tests are covered by Medicare?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers these tests (like CT scans, MRIs, EKGs, X-rays, and PET scans) when your doctor or other health care provider orders them to treat a medical problem.
Does Medicare cover carotid artery screening?
Carotid procedures and testing are covered when Medicare coverage criteria are met. Non-invasive test of carotid function (direct and indirect) is covered when criteria are met.Jun 14, 2021
What screenings are considered preventive?
Preventive CareBlood pressure, diabetes, and cholesterol tests.Many cancer screenings, including mammograms and colonoscopies.Counseling on such topics as quitting smoking, losing weight, eating healthfully, treating depression, and reducing alcohol use.Regular well-baby and well-child visits.More items...
Does Medicare cover all cancer screening?
Medicare covers these screening tests every 12 months (1 year) if you are at high-risk for cervical or vaginal cancer or if you're of childbearing age and had an abnormal Pap test in the past 36 months.May 13, 2019
Is lipid panel covered by Medicare?
Routine screening and prophylactic testing for lipid disorder are not covered by Medicare. While lipid screening may be medically appropriate, Medicare by statute does not pay for it.
Does Medicare cover cardiac screening?
Medicare covers a cardiovascular disease screening every 5 years at no cost to you. The preventive heart screening includes tests to help detect heart disease early and measures cholesterol, blood fat (lipids), and triglyceride levels.Feb 8, 2021
What activity is included in preventative health care?
Examples include immunization against disease, maintaining a healthy diet and exercise regimen, and avoiding smoking. Methods to detect and address an existing disease prior to the appearance of symptoms. Examples include treatment of hypertension (a risk factor for many cardiovascular diseases), and cancer screenings.
Is a colonoscopy considered preventive care?
A colonoscopy is an important preventive care screening test that helps detect pre-cancer or colon cancer. The earlier signs of colon cancer are detected, the easier it is to prevent or treat the disease.
What is the difference between routine and diagnostic?
Preventive care is given to you when you're symptom free and have no reason to believe you might be unhealthy. Preventive care is often given as part of a routine physical or checkup. Diagnostic care is what you receive when you have symptoms or risk factors and your doctor wants to diagnose them.
What blood work is not covered by Medicare?
You usually pay nothing for Medicare-approved clinical diagnostic laboratory tests. Laboratory tests include certain blood tests, urinalysis, tests on tissue specimens, and some screening tests.
How often will Medicare pay for a screening mammogram?
once every 12 monthscovers: A baseline mammogram once in your lifetime (if you're a woman between ages 35-39). Screening mammograms once every 12 months (if you're a woman age 40 or older).
Will Medicare pay for mammogram every year?
If you're under age 65 and on Medicare, Medicare will pay for one baseline mammogram when you're between 35 and 39 years old. Once you're 40, Medicare pays for a screening mammogram every year. When the doctor accepts assignment, you pay nothing for the screening. If the test is diagnostic, you'll pay 20% of the costs.Sep 30, 2021
How often do you get a wellness visit with Medicare?
Beneficiaries who have had Medicare Part B coverage for longer than 12 months are eligible for a yearly “wellness” visit every 12 months. During this visit, your physician will help develop or update your personalized plan for preventing diseases or disabilities based on current health and risk factors.
What is Medicare Part B?
Medicare Part B (Medical Insurance) provides this coverage. There are certain Medicare preventive services that do require payment of 20% of the Medicare-approved amount of the cost for service, after the annual Medicare Part B deductible has been paid.
Is Medicare Part B deductible?
If these additional services are not covered, you may be responsible for paying your Medicare Part B deductible and a coinsurance amount. As I’ve explained, Medicare preventive services are provided under your Medicare Part B coverage; they’re also covered under Medicare Advantage plans.
Does Medicare accept full payment?
This means that they will accept the Medicare-approved amount as full payment . Additionally, you will need to fall within the eligibility requirements and follow the requirements associated with each service. Medicare Part B (Medical Insurance) provides this coverage.
Does Medicare cover preventive care?
As a result of the Affordable Care Act, also known as health reform, the government now covers a variety of Medicare preventive services and screenings for individuals enrolled in Medicare Part B. Often, these benefits are covered at no cost to the beneficiary.
When will Medicare start covering 2021?
If you changed Medicare health or drug plans for 2021, your new coverage begins January 1. Check out your basic costs for Medicare-covered tests, items, and services to see if they’ve changed. For more personalized and cost specific information, visit your Medicare account or create one.
What to call if you choose the wrong Medicare plan?
Being confident in your plan choice is also very important. If you think you chose the wrong plan because of inaccurate or misleading information, call 1-800-MEDICARE (1-800-633-4227) and explain your situation. TTY users can call 1-877-486-2048.
What is preventive care?
Preventive services are key to maintaining your wellbeing; they keep you from getting sick and help find health problems early. Check out our complete list of Medicare-covered preventive services and watch our preventive benefits video to learn more.
Does Medicare cover breast cancer?
Medicare covers many preventive services, including your yearly “Wellness” visit and screenings for breast cancer, diabetes, and heart disease . Most of these services are provided at no cost to you. Preventive services are key to maintaining your wellbeing; they keep you from getting sick and help find health problems early.
How many visits does Medicare cover?
8) Cardiovascular disease (behavioral therapy) Medicare covers one visit per year to help you lower your risk for cardiovascular disease. During the visit, you can expect your doctor to discuss aspirin use (if appropriate), check your blood pressure, and give you tips to make sure you're eating well.
How many counseling sessions does Medicare cover?
Medicare also covers up to 2 individual 20-30 minute, face-to-face, high-intensity behavioral counseling sessions each year. These are covered for sexually active adolescents and adults at increased risk for STIs, if referred by a doctor.
How often is a mammogram covered?
A screening mammogram is covered once a year. You can also get a diagnostic mammogram when it’s medically necessary, but you will have to pay the 20% coinsurance as well as your Part B deductible if it hasn’t been met yet.
How often is a wellness visit free?
The yearly wellness visit is free after you’ve had Part B for more than a year. During this visit, your doctor or physician will have you fill out a Health Risk Assessment to help prevent disease and disability for the future. This visit is free once per year.
Is a wellness visit free with Medicare?
4) Preventive visit & yearly wellness exams. The preventive visit is free if you schedule it within the first year that you have Medicare Part B. During this visit, you get basic preventive services such as a flu shot, a vision test, blood pressure measurement, and more. The yearly wellness visit is free after you’ve had Part B for more than a year.
Does Medicare Advantage cover screenings?
If you’re in a Medicare Advantage (MA) plan, you’ll need to contact your plan for a list of covered preventive services. MA plans must cover all the same preventive services as Original Medicare, and some MA plans may even offer additional services – you just need to ask!
Does Medicare cover behavioral counseling?
If you have a BMI of 30 or above, Medicare will cover face-to-face, individual behavioral counseling sessions to help you lose weight. This counseling is only covered if you get it in a primary care setting (like a doctor's office).
What are the types of doctor visits that are covered by Medicare?
There are basically three types of doctor visits that may include preventive care and can be covered by Medicare: Your Welcome to Medicare visit. Certain preventive visits and screenings. Your annual wellness exam. New enrollees are often confused by the differences among these visits, because they are similar but not the same.
What is a welcome to Medicare visit?
At this visit, your doctor will go over your health and medical history, discuss your lifestyle and home welfare, and plan your future care, including preventive care. Typically, however, you do not receive preventive care at this visit – it is primarily a get-to-know-you interaction.
What is an annual wellness visit?
A Medicare annual Wellness visit (AWV) is similar to a standard preventive care visit to your doctor intended to check on your health, prevent and avoid disease and create a plan to maintain wellness. But these types of visits are also different.
What is an abdominal aneurysm screening?
Abdominal aortic aneurysm screening, a one-time screening for people at risk (family history of abdominal aortic an eurysms, or men between 65 and 75 who have ever smoked) who have a referral from their initial Welcome to Medicare visit or annual Wellness visit.
What does it mean when a provider does not accept Medicare?
Medicare providers that do not accept assignment can charge up to 15 percent more than the Medicare-approved amount, which could mean higher out-of-pocket costs for you.
Does Medicare cover preventive care?
Medicare covers many preventive services and health screenings at the Welcome to Medicare visit, annual wellness visits and during preventive care visits. Learn about what’s covered and what costs you may face, if any.
Do preventive services require copayments?
While some preventive services still require a copayment or coinsurance, many others are now entirely free if you meet certain guidelines and age requirements. Note: Typically, the following services are covered 100 percent by Medicare if your health care provider accepts assignment.
How often do you have to check cholesterol for Medicare?
Cardiovascular Screenings. Blood tests to check cholesterol, lipid, and triglyceride levels every 5 years, when ordered by a doctor. All Medicare beneficiaries.
What is a welcome to Medicare visit?
Several preventive screenings, tests, and services you may be eligible for are determined during key doctor’s visits, including: A Welcome to Medicare visit in which your doctor or healthcare provider looks at your medical and family history, your current health condition, and any prescriptions you currently have.
What age can you get preventive care?
We all know that preventive care is intended to prevent serious health conditions from sprouting in the future, potentially saving us thousands of dollars on healthcare costs and keeping our lives happy and healthy. If you’re age 65 or older and enrolled in Medicare — or are under age 65 and Medicare eligible because you have a disability — this is ...
What is a yearly hepatitis C test?
Hepatitis C Screening Test. One test only, or yearly screenings for people at high risk. Medicare beneficiaries who are at high risk because of past or present illicit injection drug use, those who had a blood transfusion before 1992, and those born between 1945-1965. HIV Screening.
What is cost sharing in Medicare?
Cost-sharing preventive services require the beneficiary to pay 20 percent of the Medicare-approved amount, and the Part B deductible applies. In a hospital outpatient setting, you will also have to pay a copayment. Diagnostic services are for a condition or symptoms you already have. These are cost-sharing services that require an out-of-pocket ...
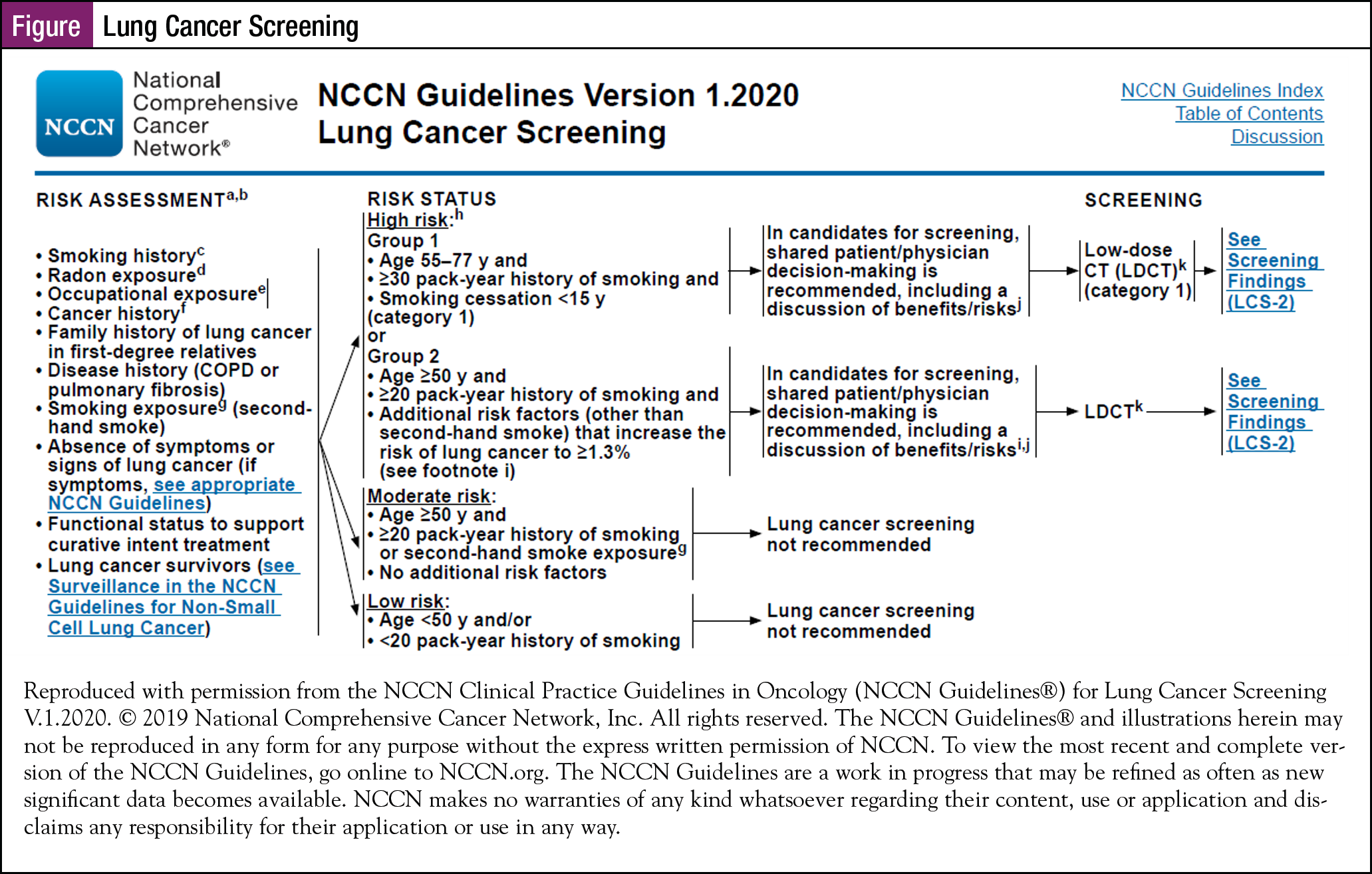
How long do you have to smoke a pack a day for Medicare?
Medicare beneficiaries who are ages 55-77, are asymptomatic, are a current smoker or quit smoking within the last 15 years, smoked a pack a day for at least 30 years, and get a written order from their physician. Medical Nutrition Therapy.
How often do you get a Pap test for cancer?
All Medicare beneficiaries. Cervical and Vaginal Cancer Screenings. Pap tests and pelvic exams once every 24 months or once every 12 months if you’re at high risk for cervical or vaginal cancer. All women with Medicare. Colorectal Cancer Screenings.
Medicare Options
Medicare has two options —the Original Medicare and Medicare Advantage. Original Medicare is made up of two parts: Part A (hospitalization) and Part B (doctor visits and testing). Most people with Medicare usually have both Part and Part B, but not always.
Medicare Enrollment Period
Medicare open enrollment runs from October 15 through December 7 annually. During this period, you may do one or more of the following:
Medicare Changes for 2022
Medicare is set to undergo certain changes for 2022. This year that includes the addition of certain services, as well as an increase in some costs.
Possible Price Increases for 2022 Medicare
A price increase is expected for some areas of Medicare come the new year. This increase includes the deductibles for Part A (hospitalization) and Part B (doctor visits and testing), as well as the premiums for Part B and Part D. While the increases may seem minor, it is important to note them, especially if you are affected by the changes.
Prepare for Open Enrollment
With these changes set to take effect in 2022, it’s important for seniors enrolled in (or about to enroll in) Medicare to be aware of and understand how these changes will impact their needs.
What is the Medicare premium for 2021?
The standard premium for Medicare Part B is $148.50/month in 2021. This is an increase of less than $4/month over the standard 2020 premium of $144.60/month. It had been projected to increase more significantly, but in October 2020, the federal government enacted a short-term spending bill that included a provision to limit ...
How many people will have Medicare Advantage in 2020?
People who enroll in Medicare Advantage pay their Part B premium and whatever the premium is for their Medicare Advantage plan, and the private insurer wraps all of the coverage into one plan.) About 24 million people had Medicare Advantage plans in 2020, and CMS projects that it will grow to 26 million in 2021.
What is the maximum out of pocket limit for Medicare Advantage?
The maximum out-of-pocket limit for Medicare Advantage plans is increasing to $7,550 for 2021. Part D donut hole no longer exists, but a standard plan’s maximum deductible is increasing to $445 in 2021, and the threshold for entering the catastrophic coverage phase (where out-of-pocket spending decreases significantly) is increasing to $6,550.
How much is the Medicare coinsurance for 2021?
For 2021, it’s $371 per day for the 61st through 90th day of inpatient care (up from $352 per day in 2020). The coinsurance for lifetime reserve days is $742 per day in 2021, up from $704 per day in 2020.
What is the income bracket for Medicare Part B and D?
The income brackets for high-income premium adjustments for Medicare Part B and D will start at $88,000 for a single person, and the high-income surcharges for Part D and Part B will increase in 2021. Medicare Advantage enrollment is expected to continue to increase to a projected 26 million. Medicare Advantage plans are available ...
How long is a skilled nursing deductible?
See more Medicare Survey results. For care received in skilled nursing facilities, the first 20 days are covered with the Part A deductible that was paid for the inpatient hospital stay that preceded the stay in the skilled nursing facility.
When will Medicare Part D change to Advantage?
Some of them apply to Medicare Advantage and Medicare Part D, which are the plans that beneficiaries can change during the annual fall enrollment period that runs from October 15 to December 7.
