Part B Claim Submission Requirements Paper (OCR) Original CMS
Centers for Medicare and Medicaid Services
The Centers for Medicare & Medicaid Services, previously known as the Health Care Financing Administration, is a federal agency within the United States Department of Health and Human Services that administers the Medicare program and works in partnership with state government…
What are the methods of claiming Medicare Part B benefits?
Medicare Claims Processing Manual Chapter 1 - General Billing Requirements Table of Contents (Rev. 10840, 06-11-21) ... 10.1 - A/B MACs (Part B) ... 10.5 – Claims Processing Requirements for Deported Beneficiaries 10.5.1 – Implementation of Payment Policy for Deported Beneficiaries ...
What is the interim process for Medicare Part B claims?
There are three situations in which a SNF may submit a claim for Part B services. These are identified in subsections A through C below. No bill is required when: • The patient is not enrolled under Part B; • Payment was made or will be made by the Public Health Service, VA, or other governmental entity;
When is payment not made for Medicare Part A or Part B?
Medicare FFS process for Part A/B claims. The chapter begins with the business service model, providing the context and high-level breakdown, or decomposition, of the Part A/B claims processing func-tion. The business service model displays what Part A/B claims processing is …
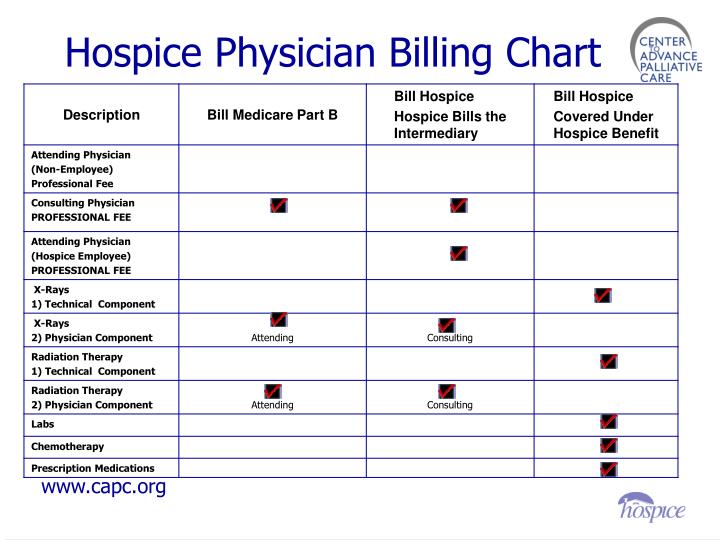
How are hospice services billed under Medicare Part B?
Avoiding Simple Mistakes on the CMS-1500 Claim Form. The Patient Protection and Affordable Care Act and other legislation have modified the requirements for the Medicare Part B claim, which is filed using the CMS-1500 claim form [PDF]. Audiologists and speech-language pathologists can refer to the checklist below to make sure their claims are not returned or …

Who processes Medicare Part B claims?
MACs are multi-state, regional contractors responsible for administering both Medicare Part A and Medicare Part B claims. MACs perform many activities including: Process Medicare FFS claims.Jan 12, 2022
What are Medicare reimbursement requirements?
If an individual has traditional Medicare and a Medigap plan, the law requires that a healthcare provider files claims for their services. An individual should not need to file a claim for reimbursement. People should present their Medicare and Medigap cards together when they receive a healthcare service.May 21, 2020
How do I process a Medicare claim?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
When must Medicare Part B providers file their claims?
Medicare regulations at 42 CFR 424.44 define the timely filing period for Medicare fee for service claims. In general, such claims must be filed to the appropriate Medicare claims processing contractor no later than 12 months, or 1 calendar year, after the date the services were furnished.Jan 21, 2011
How does Medicare Part B reimbursement work?
The giveback benefit, or Part B premium reduction, is when a Part C Medicare Advantage (MA) plan reduces the amount you pay toward your Part B monthly premium. Your reimbursement amount could range from less than $1 to the full premium amount, which is $170.10 in 2022.Dec 3, 2021
Who is eligible for Medicare Part B reimbursement?
How do I know if I am eligible for Part B reimbursement? You must be a retired member or qualified survivor who is receiving a pension and is eligible for a health subsidy, and enrolled in both Medicare Parts A and B. 2.
What document notifies Medicare beneficiaries of claims processing?
The MSN is used to notify Medicare beneficiaries of action taken on their processed claims. The MSN provides the beneficiary with a record of services received and the status of any deductibles.
How long does it take to process a Medicare claim?
When you submit a claim online, you'll usually get your benefit within 7 days.Dec 10, 2021
How long does Medicare have to process a claim?
approximately 30 daysMedicare takes approximately 30 days to process each claim. Medicare pays Part A claims (inpatient hospital care, inpatient skilled nursing facility care, skilled home health care and hospice care) directly to the facility or agency that provides the care.
Can I submit a claim directly to Medicare?
Usually, Medicare providers send claims directly to Medicare so their members don't need to do a thing. However, in some rare cases, people in Original Medicare may need to file their own claims. Follow these steps to make sure you file yours correctly.Dec 11, 2019
Who files Medicare claims?
Medicare Claims and Reimbursement If you have Original Medicare, Part A and/or Part B, your doctor and supplier are required to file Medicare claims for covered services and supplies you receive. If your doctor or the supplier doesn't file a claim, you can call Medicare at 1-800-MEDICARE (1-800-633-4227).
What is the first step in submitting Medicare claims quizlet?
The first step in submitting a Medicare claim is the health provider must submit the covered expenses.
What is the process of correcting an error on a Medicare bill?
When a SNF or intermediary discovers an error on an original bill, there are three methods for correcting the bill depending on the type of error. The SNF or intermediary may submit a late charge bill, an adjustment request, or maintain a log of charges. Each of the methods and appropriate use are explained in the Medicare Claims Processing Manual, Chapter 1, "General Billing Requirements," §130.
What is Medicare Part B SNF?
Section 1888(e)(9) of the Social Security Act (the Act) requires that the payment amount for Part B SNF services shall be the amount prescribed in the otherwise applicable fee schedule. Thus, where a fee schedule exists for the type of service, the fee amount will be paid. Where a fee does not exist on the Medicare Physician Fee Schedule (MPFS) the particular service is priced based on cost. This is also true for all “carrier-priced” codes on the MPFS, but not for services paid on the Clinical Diagnostic Laboratory Fee Schedule. All lab services missing fees are to be gap-filled. Some specific services continue to be paid on a cost basis and are specifically stated in the sections below where cost applies.
What is a pap smear?
Screening pap smears are laboratory tests consisting of a routine exfoliative cytology test (Papanicolaou test) provided for the purpose of early detection of cervical cancer. It includes a collection of the sample of cells and a physician's interpretation of the test.
What is BIPA 104?
Section 104 of the Benefits Improvement and Protection Act 2000, (BIPA) entitled "Modernization of Screening Mammography Benefit," provides for new payment methodologies for both diagnostic and screening mammograms that utilize advanced new technologies for the period April 1, 2001, through December 31, 2001. See the Medicare Claims Processing Manual, Chapter 18, "Preventive and Screening Services," for the payment method for this period, applicable HCPCS codes, and other billing and processing instructions.
What is HCPCS code?
HCPCS is required for reporting all SNF services paid under Part B, whether paid by Medicare fee schedules or by some other mechanism. A description of HCPCS codes is found in the Medicare Claims Processing Manual, Chapter 23.
What is a Part B inpatient stay?
Part B inpatient stay includes services furnished to inpatients whose benefit days are exhausted, or who are not entitled to have payment made for services under Part A. A more detailed description of services covered for beneficiaries in a Part B stay is founds at §10.1 – Billing for Inpatient Services Paid Under Part B.
Is screening covered by Medicare?
Screening and preventive services are only covered as a Medicare Part B benefit. When furnished to a beneficiary in a SNF Part A covered stay, the SNF must bill its intermediary using 22X type of bill. These services are billed on TOB 23x for SNF outpatients and beneficiaries outside the Medicare-certified SNF or DPU.
When mammography services are obtained for patients under arrangements with another facility, the provider must ensure that the facility performing the
When mammography services are obtained for patients under arrangements with another facility, the provider arranging the service must ensure that the facility performing the services has been issued a MQSA certificate by FDA.
How many localities are required for centralized billing?
To qualify for centralized billing, an individual or entity providing mass immunization services for flu and pneumonia must provide these services in at least three payment localities for which there are at least three different carriers processing claims.
What is central billing?
Centralized billing is a process in which a provider, who provides mass immunization services for influenza and Pneumococcal (PPV) immunizations, can send all claims to a single carrier for payment regardless of the geographic locality in which the vaccination was administered. (This does not include claims for the Railroad Retirement Board, United Mine Workers or Indian Health Services. These claims must continue to go to the appropriate processing entity.) This process is only available for claims for the flu and PPV vaccines and their administration. The administration of the vaccinations is reimbursed at the assigned rate based on the Medicare physician fee schedule for the appropriate locality. The vaccines are reimbursed at the assigned rate using the Medicare standard method for reimbursement of drugs and biologicals, which is based on the lower of cost or 95 percent of the Average Wholesale Price (AWP).
What is CMS-1500?
Qualifying individuals and entities must attach to the Form CMS-1500 claims form, a roster which contains the variable claims information regarding the supplier of the service and individual beneficiaries. While qualifying entities must use the modified Form CMS-1500 without deviation, carriers must work with these entities to develop a mutually suitable roster that contains the minimum data necessary to satisfy claims processing requirements for these claims. Carriers must key information from the beneficiary roster list and abbreviated Form CMS-1500 to process PPV and influenza virus vaccination claims.
How often is PPV administered?
Typically, PPV is administered once in a lifetime. Claims are paid for beneficiaries who are at high risk of pneumococcal disease and have not received PPV within the last five years or are revaccinated because they are unsure of their vaccination status.
Why is a Pap smear denied?
If there are no high risk factors, and the screening Pap smear and/or screening pelvic examination is being denied because the procedure/examination is performed more frequently than allowed use MSN 18.17:
Is a roster claim considered a paper claim?
Roster claims are considered paper claims and are not paid as quickly as electronic media claims (EMC). If available, offer electronic billing software free or at-cost to PHCs and other properly licensed individuals and entities. Carriers must ensure that the software is as user friendly as possible for the PPV and influenza virus vaccine benefits.
How much does Medicare pay for Part B?
If the provider accepts assignment (agrees to accept Medicare’s approved amount as full reimbursement), Medicare pays the Part B claim directly to him/her for 80% of the approved amount. You are responsible for the remaining 20% (this is your coinsurance ). If the provider does not accept assignment, he/she is required to submit your claim ...
How does Medicare receive claims?
Your Medigap (supplemental insurance) company or retiree plan receives claims for your services 1 of 3 ways: Directly from Medicare through electronic claims processing. This is done online. Directly from your provider, if he/she accepts Medicare assignment. This is done online, by fax or through the mail.
How to file a claim with Medicare?
Follow these steps: Fill out the claim form provided by your insurance company (if required). Attach copies of the bills you are submitting for payment (if required). Attach copies of the MSN related to those bills.
What happens if a provider does not accept assignment?
If the provider does not accept assignment, he/she is required to submit your claim to Medicare, which then pays the Part B claim directly to you. You are responsible for paying the provider the full Medicare-approved amount, plus an excess charge . Note: A provider who treats Medicare patients but does not accept assignment cannot charge more ...
Does Medicare send a bill for MSN?
For more information, see Assignment for Original Fee-for-Service Medicare . Medicare will send you a Medicare Summary Notice (MSN) form each quarter. Previously known as the Explanation of Medicare Benefits, the MSN is not a bill. You should not send money to Medicare after receiving an MSN.
