The Special Enrollment Period to sign up for Part C (must also be enrolled in Parts A & B) occurs: During the 63 days after the employer or union group health plan coverage ends, or when the employment ends (whichever is first). The Special Enrollment Period to sign up for Part D (must also enroll in Part A & B) occurs:
Full Answer
Who is eligible for Medicare Part C?
· If you do not qualify for a Special Enrollment Period, the general Medicare and Medicare Advantage Enrollment Periods are as follows: Initial Enrollment Period (IEP) – The seven-month period when you are first eligible for Medicare. See the chart below to figure out your personal IEP. General Enrollment Period (GEP) – If you miss your initial enrollment, you …
What are the pros and cons of delaying Medicare enrollment?
January–March. April–June. July–September. If you make a change, it will take effect on the first day of the following month. You’ll have to wait for the next period to make another change. You can’t use this Special Enrollment Period from October–December.
Do I need Part C of Medicare?
You’ll be given a Special Enrollment Period of eight months to sign up starting the month that follows the end of your employer coverage. Enroll in Medicare Advantage ( Medicare Part C) or a Prescription Drug Plan ( Medicare Part D ). You have two months to enroll in these options. Additionally, there’s a Medicare Advantage SEP for ...
Is part C and Original Medicare the same?
· There are actually two kinds of Medicare Special Enrollment Periods. A Medicare Special Enrollment Period allows you to switch plans or sign up for Medicare outside of the standard Medicare enrollment periods. Special Enrollment Period – Qualifying Life Events: 2 months; Special Enrollment Period – Working Past 65: 8 months . If you have Medicare: For …

Can you add Medicare Part C at any time?
It runs from October 15 to December 7 each year. You can add, change, or drop Medicare Advantage plans during the AEP, and your new coverage starts on January 1 of the following year.
During which period can a member enroll in a different part C plan?
15 – Dec. 7 each year, and is generally the one time of year you can make changes to your plan. If you don't already have a Medicare Advantage plan, you can choose to enroll in one during this time.
What is the length of the special enrollment period?
Depending on your Special Enrollment Period type, you may have 60 days before or 60 days following the event to enroll in a plan. You can enroll in Medicaid or the Children's Health Insurance Program (CHIP) any time. Job-based plans must provide a Special Enrollment Period of at least 30 days.
When should you apply for Medicare Part C?
When you first get Medicare (Initial Enrollment Periods for Part C & Part D)If you joinYour coverage beginsDuring one of the 3 months before you turn 65The first day of the month you turn 65During the month you turn 65The first day of the month after you ask to join the plan1 more row
What is the Medicare initial enrollment period?
7 monthsGenerally, when you turn 65. This is called your Initial Enrollment Period. It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65. My birthday is on the first of the month.
What are the extra benefits in Medicare Part C?
Medicare Advantage Plans may offer extra coverage, such as vision, hearing, dental, and/or health and wellness programs.
What is a special enrollment?
Special enrollment in California You qualify for a special enrollment period if you have a certain life event. You generally have 60 days from the date of your qualifying life event to enroll for health coverage or change your plan. In most cases, you need to have proof of your life event.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
What qualifies as a life changing event for Medicare?
A change in your situation — like getting married, having a baby, or losing health coverage — that can make you eligible for a Special Enrollment Period, allowing you to enroll in health insurance outside the yearly Open Enrollment Period.
How do I apply for Medicare Part C?
Once you understand the plan's rules and costs, here's how to join:Use Medicare's Plan Finder.Visit the plan's website to see if you can join online.Fill out a paper enrollment form. ... Call the plan you want to join. ... Call us at 1-800-MEDICARE (1-800-633-4227).
Is Medicare Part C required?
You don't need to buy a Medicare Part C plan. It's an alternative to original Medicare that offers additional items and services. Some of these include prescription drugs, dental, vision, and many others.
What is Medicare Part C used for?
Medicare Part C outpatient coverage doctor's appointments, including specialists. emergency ambulance transportation. durable medical equipment like wheelchairs and home oxygen equipment. emergency room care.
When can I enroll in a Medicare Advantage plan?
You're newly eligible for Medicare because you turn 65. Sign up for a Medicare Advantage Plan (with or without drug coverage) or a Medicare drug plan. During the 7‑month period that starts 3 months before the month you turn 65, includes the month you turn 65, and ends 3 months after the month you turn 65.
Is it too late to change Medicare plans?
Anyone can change their Medicare Advantage Plan during their Initial Enrollment Period, Open Enrollment or Medicare Advantage Open Enrollment. Open Enrollment occurs every year from October 15 to December 7. Medicare Advantage Open Enrollment lasts from January 1 through March 31 each year.
At what age will a person normally enroll with an insurance carrier under a Part C Medicare Advantage Plan?
The Medicare initial enrollment period (IEP) begins from 3 months before a person turns 65 and lasts for 7 months. During this enrollment period, a person can enroll in: Medicare Parts A and B. Medicare Part C (Medicare Advantage)
What is Medicare Part C and how does it work?
Medicare Advantage, or Medicare Part C, is a type of Medicare plan that uses private health insurance to cover all the services you'd receive under Medicare Parts A and B. Anyone who is eligible for original Medicare Parts A and B is eligible for the Medicare Advantage programs in their area.
When is Medicare open enrollment?
The open enrollment period goes from October 15 through December 7 each year . Medicare Advantage (Part C) open enrollment. This period is from January 1 though March 31 each year. Sometimes changes in your life circumstances make it necessary to change your healthcare coverage at other times during the year.
When do you have to sign up for Medicare Part A and Part B?
If you have health insurance coverage through your employer and you work for an employer with fewer than 20 employees, it’s important to sign up for Medicare Part A and Part B when you’re first eligible or you may have to pay a late enrollment penalty.
How to change Medicare Advantage plan?
Depending on the life event that has made you eligible for an SEP, you may be able to: 1 Switch from a Medicare Advantage (Part C) plan to original Medicare (parts A and B). 2 Switch from original Medicare to a Medicare Advantage plan. 3 Switch to a different Medicare Advantage plan. 4 Add, drop, or change your prescription drug coverage. 5 Drop your Medicare coverage and opt for an employer-provided plan.
What is a SEP in Medicare?
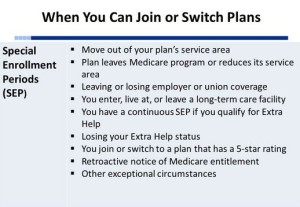
Certain life events can trigger a Medicare special enrollment period (SEP). An SEP can begin when a change in your residence affects your coverage. SEPs also apply when you lose coverage, have a chance to get new coverage, or become eligible for certain special programs. The time you have to choose new coverage varies depending on the event ...
Can you change your Medicare coverage?
Sometimes changes in your life circumstances make it necessary to change your healthcare coverage at other times during the year. Medicare does allow you to change your Medicare coverage in certain special circumstances. When one of these qualifying events happens in your life, it triggers an SEP.
Parts A and B Special Enrollment Periods
Did you know that there are special circumstances, or Special Enrollment Periods (SEPs), when you can enroll in Part A and Part B outside the normal enrollment periods without incurring a penalties?
Medicare Advantage and Part D Special Enrollment Periods
There are also special circumstances in which you can make changes to your Medicare Advantage and Medicare Part D prescription drug coverage.
General Enrollment Periods
If you do not qualify for a Special Enrollment Period, the general Medicare and Medicare Advantage Enrollment Periods are as follows:
How long do you have to enroll in Medicare Advantage?
Enroll in Medicare Advantage ( Medicare Part C) or a Prescription Drug Plan ( Medicare Part D ). You have two months to enroll in these options. Additionally, there’s a Medicare Advantage SEP for individuals who are Dual-Eligible or receive “Extra Help” (also known as Low Income Subsidy).
What is a SEP in Medicare?
The Medicare Special Enrollment Period (SEP) takes place when certain events or life changes occur, giving you the opportunity to make changes to your existing Medicare Advantage plan and Medicare Prescription Drug plan.
What is extra help?
Extra Help is a federal program that helps pay for some to most out-of-pocket costs of Medicare prescription drug coverage. If you receive Extra Help in 2020, there is a SEP to enroll in a Medicare Advantage plan with or without drug coverage, a Part D plan, or to switch between plans.
What is a special enrollment period for Medicare?
A Medicare Special Enrollment Period allows you to switch plans or sign up for Medicare outside of the standard Medicare enrollment periods. If you have Medicare: For people who already have Medicare and who experience a qualifying life event, there is a two-month Special Enrollment Period for switching a Medicare Advantage or Part D plan.
How long is the Medicare Advantage enrollment period?
If you have Medicare: For people who already have Medicare and who experience a qualifying life event, there is a two-month Special Enrollment Period for switching a Medicare Advantage or Part D plan.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
What is the late enrollment penalty for Medicare?
The late enrollment penalty is an amount that’s added to your Part D premium. You may owe a late enrollment penalty if at any time after your Initial Enrollment Period is over, there’s a period of 63 or more days in a row when you don’t have Part D or other creditable prescription drug coverage. Creditable prescription drug coverage is coverage (for example, from an employer or union) that’s expected to pay, on average, at least as much as Medicare’s standard prescription drug coverage. If you have a penalty, you may have to pay it each month for as long as you have Medicare drug coverage. For more information about the late enrollment penalty, visit Medicare.gov, or call 1‑800‑MEDICARE (1‑800‑633‑4227). TTY users can call 1‑877‑486‑2048.
Is Medicare limited to certain times?
Enrollment in Medicare is limited to certain times. This publication has information about enrolling in Medicare Advantage Plans (Part C) and Medicare Prescription Drug Plans (Part D), including who can sign up, when to sign up, and how the timing, including signing up late, can affect your costs.
What happens if you don't enroll in Part D?
If you do not enroll in Part D when you are first eligible, and you do not have creditable drug coverage, you will likely have to pay a premium penalty if you later enroll in a Part D plan.
What is a SEP plan?
The length of the Special Enrollment Period (SEP) and the effective date of your new coverage vary depending on the circumstances that trigger your SEP. The plan and, in some cases, the Centers for Medicare & Medicaid Services (CMS), determine whether you qualify for an SEP.
When will SEP be available in 2021?
Starting on February 15, 2021 and continuing through May 15, 2021, Marketplaces using the HealthCare.gov platform will operationalize functionality to make a SEP available to all Marketplace-eligible consumers who are submitting a new application or updating an existing application.
Does CMS have a marketplace?
CMS strongly encourages states operating their own Marketplace platform s to make a similar enrollment opportunity available to consumers in their states .
When is the Affordable Care Act 2021?
Jan 28, 2021. Affordable Care Act. The coronavirus disease 2019 (COVID-19) national emergency has presented unprecedented challenges for the American public. Millions of Americans are facing uncertainty and millions of Americans are experiencing new health problems during the pandemic. Due to the exceptional circumstances ...
How long do you have to change your health insurance plan?
Consumers will have 30 days after they submit their application to choose a plan. Current enrollees will be able to change to any available plan in their area without restriction to the same level of coverage as their current plan.
What is the national emergency for the US?
The coronavirus disease 2019 (COVID-19) national emergency has presented unprecedented challenges for the American public. Millions of Americans are facing uncertainty and millions of Americans are experiencing new health problems during the pandemic. Due to the exceptional circumstances and rapidly changing Public Health Emergency (PHE) impacting millions of people throughout the US every day, many Americans remain uninsured or underinsured and still need affordable health coverage. In accordance with the Executive Order issued today by President Biden, the Centers for Medicare & Medicaid Services (CMS) determined that the COVID-19 emergency presents exceptional circumstances for consumers in accessing health insurance and will provide a Special Enrollment Period (SEP) for individuals and families to apply and enroll in the coverage they need. This SEP will be available to consumers in the 36 states served by Marketplaces that use the HealthCare.gov platform, and CMS will conduct outreach activities to encourage those who are eligible to enroll in health coverage. CMS strongly encourages states operating their own Marketplace platforms to make a similar enrollment opportunity available to consumers in their states.
