2022 Medicare Advantage Prescription Drug Plans Star Ratings
| Overall Star Rating | Number of Plan Contracts | % of Total Plans (Weighted by Enrollment ... |
| 5 Stars | 74 | 26.6% |
| 4.5 Stars | 96 | 33.2% |
| 4 Stars | 152 | 29.9% |
| 3.5 Stars | 122 | 8.5% |
What are top rated Medicare Advantage plans?
The Medicare Stars is a rating system developed by the Centers for Medicare & Medicaid Services (CMS). The system rates Medicare Advantage (MA) and Prescription Drug (PDPs or Part D) plans on a 5-star scale with 1 being the lowest and 5 being the highest score. Measurements focus on health plan quality based on measurements of customer satisfaction and quality of …
How do you find top rated Medicare Advantage plans?
Jun 21, 2021 · In 2021, most (80%) Medicare Advantage enrollees are in plans with quality ratings of 4 or more stars, an increase from 2020 (76%). An additional 5 percent of enrollees are in plans that were not...
Which Medicare Advantage plan is the best?
8 rows · Nov 18, 2021 · All Medicare Advantage plans (Medicare Part C) and Medicare prescription drug plans ...
How are Medicare Advantage plans rated by the government?
66 rows · Oct 14, 2021 · A Best Insurance Company for Medicare Advantage Plans is defined as a company whose plans ...

Who has the highest rated Medicare Advantage plan?
List of Medicare Advantage plansCategoryCompanyRatingBest overallKaiser Permanente5.0Most popularAARP/UnitedHealthcare4.2Largest networkBlue Cross Blue Shield4.1Hassle-free prescriptionsHumana4.01 more row•Feb 16, 2022
What is the star rating system for Medicare Advantage plans?
Medicare uses information from member satisfaction surveys, plans, and health care providers to give overall performance star ratings to plans. A plan can get a rating between 1 and 5 stars. A 5-star rating is considered excellent. These ratings help you compare plans based on quality and performance.
What is devoted star rating on its Medicare Advantage plans?
Medicare uses a Star Rating System to measure how well Medicare Advantage and Part D plans perform. Medicare scores how well plans perform in several categories, including quality of care and customer service. Ratings range from one to five stars, with five being the highest and one being the lowest.
What states have 5-star Medicare Advantage plans?
States where 5-star Medicare Advantage plans are available:Alabama.Arizona.California.Colorado.Florida.Georgia.Hawaii.Idaho.More items...•Jan 31, 2022
How often are CMS Star Ratings released?
annuallyPlans are rated on a one-to-five scale, with one star representing poor performance and five stars representing excellent performance. Star Ratings are released annually and reflect the experiences of people enrolled in Medicare Advantage and Part D prescription drug plans.Oct 8, 2021
What is the 5-Star SEP?
The 5-Star Special Enrollment Period (SEP) is a once-a-year opportunity to switch from your current Medicare Part D prescription drug plan (PDP) or Medicare Advantage plan (MA or MAPD) to another Medicare Part D or Medicare Advantage plan with a "5-Star" quality rating.
What is devoted star rating?
This lets you easily compare plans based on quality and performance. Star Ratings are based on factors that include: • Feedback from members about the plan's service and care. • The number of members who left or stayed with the plan. • The number of complaints Medicare got about the plan.
What are the Medicare 5 star measures?
5-Stars is the highest rating CMS considers any plan with a 4-star rating or more to be an above average plan. However, if a plan gets a 5-star rating, it is considered excellent. This means you'll get a plan that excels at keeping members healthy and has better customer service.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
What determines star ratings Medicare?
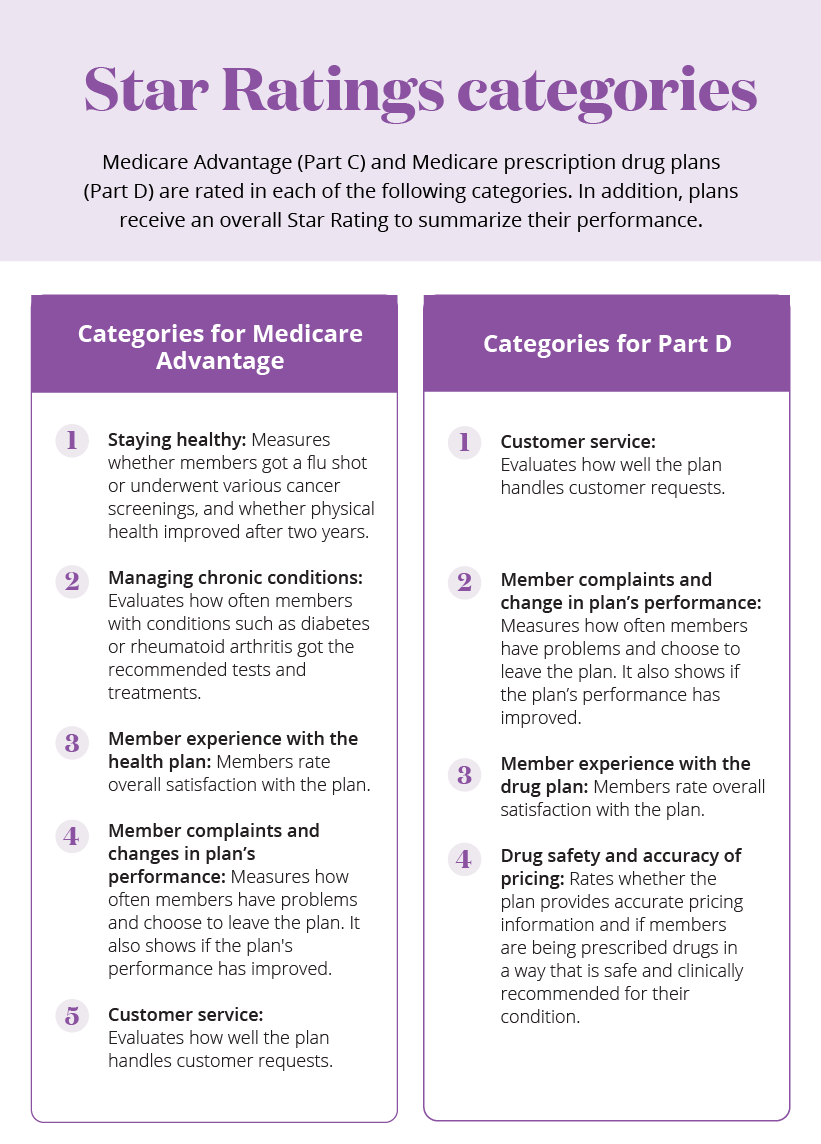
A Medicare Advantage plan's overall rating is determined by 5 categories – staying healthy, managing chronic (long-term) conditions, member experience with the health plan, member complaints and changes in the health plan's performance, and health plan customer service.
Who sets the standards for Medicare star ratings?
The Centers for Medicare & Medicaid Services (CMS) publishes the Medicare Part C and D Star Ratings each year to measure the quality of health and drug services received by beneficiaries enrolled in Medicare Advantage (MA) and Prescription Drug Plans (PDPs or Part D plans).Oct 13, 2020
How many star measures are there?
Of the more than 40 measures used to determine a health plan's Star Rating, the measures we have listed below can have the greatest impact on Independence's Star Ratings during measurement year 2017.
What is the MLR for Medicare Advantage?
However, plans’ ability to keep these and other payments as profit is not unlimited – Medicare Advantage plans must meet medical loss ratio (MLR) requirements of at least 85 percent, and are required to issue rebates to the federal government if their MLRs fall short of required levels.
How many stars does a health insurance plan have?
As a result of changes made in the Affordable Care Act (ACA), plans that receive at least 4 stars and those without ratings ...
What is Medicare Advantage 2021?
Medicare Advantage in 2021: Star Ratings and Bonuses. Medicare Advantage plans receive a star rating based on performance measures that are intended to help potential enrollees compare plans available in their area as well as encourage plans to compete based on quality. All plans that are part of a single Medicare Advantage contract are combined ...
How much will Medicare pay in 2021?
Medicare spending on bonus payments to Medicare Advantage plans totals $11.6 billion in 2021. Between 2015 and 2021, the total annual bonuses to Medicare Advantage plans have nearly quadrupled, rising from $3.0 billion to $11.6 billion. The rise in bonus payments is due to both an increase in the number of plans receiving bonuses, ...
What is a quality rating?
Quality ratings are assigned at the contract level, rather than for each individual plan, meaning that each plan covered under the same contract receives the same quality rating. Most contracts cover multiple plans, and can include individual plans, as well as employer-sponsored and special needs plans (SNPs).
How much is the bonus for Medicare 2021?
UnitedHealthcare and Humana, which together account for 46% of Medicare Advantage enrollment, have bonus payments of $5.3 billion (46% of total bonus payments) in 2021. BCBS affiliates (including Anthem BCBS) and CVS Health each have $1.6 billion in bonus spending, followed by Kaiser Permanente ($1.1 billion), Cigna and Centene ($0.2 billion each).
Is Medicare Advantage enrollment growing?
As Medicare Advantage enrollment continues to grow and fiscal pressure on the Medicare program increases, questions pertaining to the quality rating system, associated bonus payments, and related costs to Medicare and taxpayers may be on the agenda.
What is the star rating for Medicare Advantage?
1. A five-star rating system is used, with one star being given to the lowest-rated plans, and five stars being reserved for only the highest-rated plans.
When did Medicare start using the star rating system?
The Centers for Medicare & Medicaid Services started using the Star Rating system in 2007 to evaluate Medicare Advantage plan contracts. The goal of the Medicare Star Rating system is to help Medicare-eligible individuals and Medicare beneficiaries better understand the quality of the plans that are available on the market.
How to speak to a licensed insurance agent about Medicare Advantage?
Because the availability of Medicare Advantage plans varies from one location to the next, you may want to call. 1-800-557-6059. 1-800-557-6059 TTY Users: 711 to speak with a licensed insurance agent. An agent can go over the plan options available in your area and identify which ones have received a five-star rating.
What is a 5 star plan?
A 5-star plan is considered an excellent plan, and any plan rated 4 stars or higher is considered "top rated.". 1-star plans are the lowest-rated plans, and these plans typically earn their low rating due to poor plan performance, low customer satisfaction and bad customer service. The star rating system for Medicare Advantage plans is as follows: ...
How long does Medicare enrollment last?
You are given a 7-month Medicare Initial Enrollment Period. This period begins three months before you turn 65 years old, includes the month of your birthday and continues for three months thereafter. You are only eligible to enroll in plans that are offered in your area.
When is Medicare open enrollment?
If you are already enrolled in Part A and/or Part B, you may sign up for a Medicare Advantage plan during the fall Medicare Open Enrollment Period, which lasts from October 15 to December 7 each year.
How many MA-PD beneficiaries will be in 2021?
According to the CMS, roughly 77 percent of all beneficiaries of Medicare Advantage plans that include prescription drug coverage (called MA-PD plans) are enrolled in 2021 Medicare Advantage plans rated 4 stars or higher. This means that more than 3 out of 4 MA-PD beneficiaries are enrolled in a top-rated 2021 Medicare Advantage plan.
