Medicare Part B traditionally has covered the medication and administration costs of treatments given by infusion, including chemotherapy, and with the advent of biologic agents, medications such as infliximab (3).
What drugs does Medicare Part B cover?
What kind of drugs are covered under Medicare Part B vs. Parts A and D? Part B drug coverage is typically for medications you receive in a doctor’s office or outpatient setting. Coverage includes: Drugs used with medical equipment like an infusion pump or a nebulizer. Antigens. Injectable osteoporosis drugs
What are injections covered by Medicare?
- erectile dysfunction or low sex drive
- hair loss, body and head
- muscle and bone mass loss
- breast tissue growth
- fatigue
- memory impairment
- mood irregularities
What does Part B in Medicare cover?
What does Medicare Part B cover?
- Doctor visits
- Certain cancer screenings
- Certain lab tests
- An annual wellness visit with your primary care provider
- A one-time Welcome to Medicare visit with your primary care provider
- Diabetes screening, supplies, and certain services
- A diabetes prevention program for those who qualify
- Alcohol abuse screening and counseling for those who qualify
- Flu shots
Is Procrit covered by Medicare?
Most Medicare prescription drug plans have prior authorization rules that will require your prescriber to contact your plan before you can get your medication. This is to show that the drug is medically necessary. What drug tier is Procrit typically on? Medicare prescription drug plans typically list Procrit on Tier 5 of their formulary.
Are biologics covered by Medicare?
Most private health insurance plans cover biologics for RA. So do Medicare Part D and Medicaid.
Does Medicare Part D pay for Enbrel?
Enbrel is a medication that people take to treat certain autoimmune diseases. Usually, Medicare Part D and Medicare Advantage plans offer coverage for the medication. As Enbrel is a specialty drug, Medicare Part D may cover it at a more reduced rate compared with other medications.
Does Medicare cover Remicade?
Do Medicare prescription drug plans cover Remicade? No. In general, Medicare prescription drug plans (Part D) do not cover this drug.
Do Medicare Advantage plans cover biologics?
Medicare Advantage plans covered more individual biologic DMARDs (55% to 100%) than stand-alone drug plans (22% to 100%), but charged higher average coinsurance (31.1% vs. 29.0%).
Is Humira covered by Medicare?
Medicare does provide coverage for Humira. It's usually covered through Medicare Part D, which is Medicare's prescription drug coverage. Part D plans are sold by private insurance companies and can be added to your original Medicare coverage.
Is cimzia covered by Medicare?
CIMZIA* is now covered by Medicare Administrative Contractors administering Medicare Part B to patients in all 50 United States and US Territories.
How much does Remicade cost of Medicare?
Then, depending on your medical condition, you may get an infusion every other month or so. What you pay out-of-pocket for a single dose of Remicade depends on where you live and who administers it, but it generally costs between $1350.00 and $2600.00 in the U.S.
Does Medicare cover biologics for Crohn's?
Most Medicare beneficiaries are enrolled in Part B automatically. This part of Medicare typically covers infusion biologic costs but frequently has a coinsurance that the patient is responsible for paying.
Is actemra covered by Medicare?
Do Medicare prescription drug plans cover Actemra? No. In general, Medicare prescription drug plans (Part D) do not cover this drug.
Are biologics covered by Medicare Part B?
Medicare Part B traditionally has covered the medication and administration costs of treatments given by infusion, including chemotherapy, and with the advent of biologic agents, medications such as infliximab (3).
What is the cheapest biologic?
The cheapest biosimilars are Kanjinti and Ogivri, which are both 15% cheaper than Herceptin for a 150 mg vial. Herzuma, which was approved in 2018, has only a 10% discount compared to Herceptin.
Does Medicare pay for Stelara injections?
Medicare will no longer cover STELARA SQ injections under the medical benefit (Part B) and instead will cover STELARA SQ under the prescription benefit (Part D).
Does Medicare Cover Orencia Infusions
Orencia is also a biologic DMARD its available as an infusion or an injection. If you have an infusion, your doctor will administer the drug through a vein in your arm.
Sorting Out Insurance Plans And Covered Treatment Options
It is incomprehensible to me why insurance companies make the process so cumbersome and difficult and unpleasant. Add to that the fact that we often shift insurance carriers over the years for various reasons. That adds a whole new level of complication as we try to sort out which plan to get or what medications and treatments are covered.
When Does Medicare Part B Cover Orencia
Generally, Medicare Part B covers the cost of intravenous infusions performed in a doctor’s office, provided that the treatment is deemed medically necessary and the physician participates in Medicare. You will usually have to first pay your deductible to receive coverage.
Infusions Under The Medical Side Of Medicare
The good news for me, and anyone who uses injectables that are also available by infusion, is that I now can get my medication under the medical side of Medicare, rather than through the RX side, simply by switching to infusions as the medication delivery method. I did not get this information as a routine matter of course from my care team.
Ra Costs: What Are Payment Options For Treating Rheumatoid Arthritis
Rheumatoid arthritis is a chronic disease that requires ongoing medication and treatment for the majority of patients. Many of these treatments are highly effective and can stop the diseases progression, preventing further joint damage.
Rheumatoid Arthritis Treatment And Medicare Coverage
Medicare covers a wide range of treatments to slow the progression of rheumatoid arthritis and help with its symptoms. Rheumatoid arthritis treatments can be costly, even with Medicare. If you dont have supplemental coverage, you may pay thousands of dollars.
Paying For Rheumatoid Arthritis Treatment
There are many programs and organizations available to help support RA patients in need of financial support. Be sure to speak with your healthcare team about any financial concerns. Your doctor or rheumatologist may be able to suggest programs and offer assistance in order to ensure you get the personalized treatment that you need.
When did Medicare go into effect?
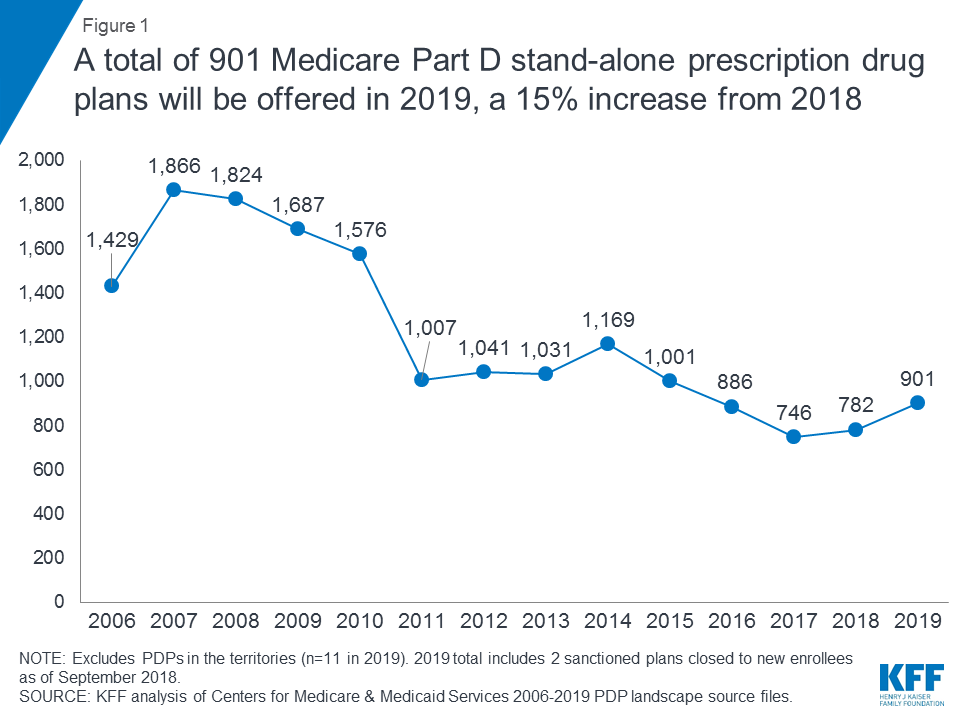
It wasn't until 2003, that the Medicare Modernization Act was passed that created the Medicare drug benefit which went into effect in 2006. A windfall for the drug industry, and some say written by drug lobbyists, it banned the federal government from negotiating directly with drug companies for lower prices.
What is Medicare Advantage Plan?
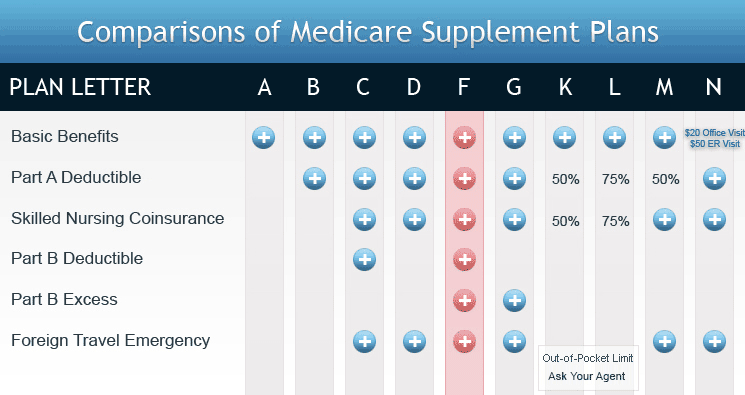
An option some Medicare beneficiaries choose is a private Medicare Advantage plan (Part C), which covers Part A, B and D. Biologics and specialty drugs are expensive drugs, and often in the highest tiers in Part D and Medicare Advantage plans.
What to do if you don't have Medicare Part D?
If you do not have Medicare Part D, the drug company has assistance to pay for most if not all of your cost. Call the drug company assistance # and they can let you know what they will pay and how to go about it. Then call your health insurance and find out how much they will pay and co-pay.
Do you have to have Medicare A for biologics?
No, I was just explaining what each is. For those of us on biologics, it's worth it to have Medicare A, which is required and a second insurance which covers ancillary bills. Just don't take D because you won't get any aid for copay on your drug.
Can Medicare pay part of a drug claim?
If the drug company is receiving federal grants to get the drug out to market, then by law, Medicare cannot pay part of your claim.
Can Medicare beneficiaries get private insurance?
Medicare beneficiaries are not eligible for private insurance sold on the ACA (Obamacare) exchange. Usually, if someone has original Medicare, they have Part A (for hospitalization) and pay a premium for Part B (for outpatient care). Part B covers 80% of health costs.
Can Medicare negotiate drug discounts?
".... Medicare can’t negotiate drug discounts with the manufacturers like private insurance companies can!"#N#***********************************#N#Legislation passed in 1965 that created the Medicare program did not include prescription drug coverage.#N#It wasn't until 2003, that the Medicare Modernization Act was passed that created the Medicare drug benefit which went into effect in 2006. A windfall for the drug industry, and some say written by drug lobbyists, it banned the federal government from negotiating directly with drug companies for lower prices. Instead, the private for-profit insurance companies that sell Part D plans negotiate prices with drug companies.#N#Unlike those with employer health plans who are eligible for drug company patient assistance programs and receive help w/copays - regardless of income -- Medicare beneficiaries are not eligible due to a 1972 anti-kickback statute, which bars payments made to induce patients to choose particular services.#N#See Patient Assistance Programs for Medicare Enrollees, 2005 - page 70625, II. Federal Anti-Kickback Statute#N#https://oig.hhs.gov/fraud/docs/alertsandbulletins/2005/2005PAPSp...
Do you need a modifier for a manufacturer's claim?
The manufacturer modifier is not required on claims that use a miscellaneous HCPCS code. Please note that the determination of the payment amount for biosimilars is not affected by the use of a modifier.
Do you need a modifier to claim a HCPCS code?
However, if a HCPCS code and corresponding biosimilar modifier (s) do not appear on the quarterly update, then a modifier is not required to appear on claims for the code.
Psoriasis Gone!
For the first time in 20 years my psoriasis cleared up. No steroid creams, moisturizers, no specials baths. I finally over time understood that this is a condition that needs to be healed from the inside out. Everyone is different, the reason why all of you are getting psoriasis I cannot say.
Black Seed Oil---a miracle gift from God
I have been dealing with psoriasis for about 13 years now. Two years ago I was determined to find the cause and rid myself of this. I have read literally thousands of articles, studies and posts about psoriasis, causes, research, etc.
Papaya helps suppressing Psoriasis
I have had Psoriasis all over my body for over 10 years now and no medicine ever helped except Methotrexate which I stopped 2 years ago. it started in my scalp and when I peeled off the extra skin watery substance came. I didn't knew at that time that my life is going to change from that point onwards.
How I've Cleared my Psoriasis (Almost all the way)!
Hi guys, I wanted to take a few moments to share how I've cleared up my skin. For those who want me to cut to the chase - I used oregano essential oil, 4-8 drops in veggie capsules with a full glass of water. (Never on an empty stomach, that can make you feel sick). Make SURE to drink plenty of water with it too. :) Now, a little more detail.
Is a compounded drug covered by Medicare?
Compounded drugs created by a pharmacist in accordance with the Federal Food, Drug and Cosmetic Act and the FDA Modernization Act of 1997 may be covered under Medicare when their use meets all other criteria for services incident to a physician's service. Compounded drugs do not have a National Drug Code number (NDC).
Is Noridian a biosimilar?
The FDA approved use of biosimilars for FDA approved drugs, has increased recently. Noridian will accept a biosimilar drug on the same criteria as the drug to which it is a biosimilar unless an article is published to the contrary.
How much does it cost to take biologics for RA?
These genetically engineered drugs often slow or halt the progression of joint damage, and they may even push RA into remission. But the drugs are expensive; they cost about $1,000 to $3,000 a month.
How many biologics are there for RA?
There are nine biologics available for the treatment of RA. Each type targets a specific inflammatory mechanism of the immune system. Some are given as an injection -- a shot under the skin -- others are given by infusing it directly into a vein (IV or intravenously).
How much does RA medication cost?
But the drugs are expensive; they cost about $1,000 to $3,000 a month. Even with health insurance, your out-of-pocket costs can add up to hundreds or thousands of dollars. Here’s what you need to know about paying ...
Do insurance companies cover biologics?
Although many insurance plans cover biologics at some level, you usually have to pay a percentage of the cost. And getting your insurer's approval for the drugs can take time. Here are five tips to help you get started. Check your individual policy to see if biologics are covered and what your co-pay is.
Is there a more effective biologic?
There may be an equally or more effective biologic that costs less. Taking a long-term view, evidence shows that all the biologics aggressively slow the disease, which may ultimately reduce the overall cost of managing the disease by reducing complications, long-term disability, and the need for surgery.
Do you need pre-authorization for biologics?
If it is covered, find out if drug costs apply to your out-of-pocket maximum; most of the time they won’t. You may need pre-authorization from your insurance company before treatment can start.
Do drug companies offer financial assistance?
Many drug companies offer financial help for biologics. Most offer reimbursement services to help with your co-pay or other discount programs. Check the drug manufacturer’s web site to find out how the company can help you. Your pharmacist or doctor may also have information on financial assistance.
What is Medicare Advantage Policy Guideline?
The Medicare Advantage Policy Guideline documents are generally used to support UnitedHealthcare Medicare Advantage claims processing activities and facilitate providers’ submission of accurate claims for the specified services. The document can be used as a guide to help determine applicable:
What happens if a drug is not indicated by CMS?
If a use is identified as not indicated by CMS or the FDA, or if a use is specifically identified as not indicated in one or more of the compendia listed, or if the contractor determines, based on peer-reviewed medical literature, that a particular use of a drug is not safe and effective, the off-label use is not supported and the drug will not be covered.
Is it safe to use a biological drug?
Use of the drug or biological must be safe and effective and otherwise reasonable and necessary. (See the Medicare Benefit Policy Manual, Chapter 16, “General Exclusions from Coverage,” §20.) Drugs or biologicals approved for marketing by the Food and Drug Administration (FDA) are considered safe and effective for purposes of this requirement when used for indications specified on the labeling. Therefore, the program may pay for the use of an FDA approved drug or biological, if: