Medicare Part B (Medical Insurance) covers some diabetes supplies, including: Blood sugar (glucose) testing monitors. Blood sugar test strips. Insulin. Lancet devices and lancets.
Full Answer
Which glucose meters are covered by Medicare?
Blood sugar monitors Medicare Part B (Medical Insurance) covers blood sugar (glucose) monitors as durable medical equipment (DME) that your doctor prescribes for use in your home. Your costs in Original Medicare After you meet the Part B Deductible , you pay 20% of the Medicare-Approved Amount (if your supplier accepts assignment ).
Are glucometers covered by Medicare?
10 Section 2: Medicare Part B-covered Diabetes Supplies Blood sugar self-testing equipment & supplies Part B covers blood sugar (also called blood glucose) self-testing equipment and supplies as durable medical equipment, even if you don’t use insulin. Self-testing supplies include: • Blood sugar monitors • Blood sugar test strips
Does Medicare cover a glucometer?
Mar 28, 2018 · Original Medicare Part B covers some diabetic supplies, including: Blood sugar (glucose) test strips Blood glucose monitors, lancet devices, and lancets Glucose control solutions for checking the accuracy of test strips and monitors Insulin if you are using a medically necessary insulin pump (see below) Therapeutic shoes or inserts (see below) There may be …
Does Medicare cover talking glucometers?
Mar 21, 2022 · Medicare Advantage plans cover glucose monitors in the same way as Medicare Part B and often offer additional benefits, such as vision, dental, and prescription drug coverage. Some types of Medicare Advantage plans use provider networks, and may reduce the amounts you pay to monitor your glucose levels at home with a glucose monitor.

What brand of glucose meter is covered by Medicare 2021?
A2: Starting January 1, 2021, covered meters include: OneTouch Verio Reflect ®, OneTouch Verio Flex®, OneTouch Verio® and OneTouch Ultra 2®.
What glucose meters does Medicare cover?
Medicare Part B covers therapeutic continuous glucose monitors (CGM) such as the Freestyle Libre 2 and the Dexcom G6 for people with diabetes. Medicare covers therapeutic continuous glucose monitors as durable medical equipment (DME).
What brand of glucose meter does Medicare 2022 coverage?
Accu-Chek ® is ALWAYS COVERED on Medicare Part B.
Does Medicare cover the cost of a glucometer?
Note: Medicare won't pay for any supplies you didn't ask for, or for any supplies that were sent to you automatically from suppliers, including blood sugar monitors, test strips, and lancets.
Does Medicare cover A1c blood test?
Hemoglobin A1c Tests: Your doctor might order a hemoglobin A1c lab test. This test measures how well your blood glucose has been controlled over the past 3 months. Medicare may cover this test for anyone with diabetes if it is ordered by his or her doctor.
How often does Medicare pay for A1c blood test?
Diabetes: once a year, or up to twice per year if you are higher risk (the A1C test will need to be repeated after 3 months) Heart disease: cholesterol, lipids, and triglycerides screening once every 5 years.
Does Medicare cover glucometer for prediabetes?
Medicare may bill you for any diagnostic care you receive during a preventive visit. Part B also covers certain diabetic supplies, including: Glucose monitors. Blood glucose test strips.
Is Accu Chek guide discontinued?
After 18 years, Roche Diabetes Care is discontinuing the Accu-Chek ® Compact Plus blood glucose meter. Learn why this platform is going away and how you can get the latest Accu-Chek Guide Me meter for free!
Who qualifies for CGM under Medicare?
To qualify for CGM coverage, you must3: Be diagnosed with diabetes type 1 or type 2. Use a blood glucose monitor (BGM) Test your blood sugar four or more times per day.
Does Medicare cover CGM type 2 diabetes?
Yes. The Dexcom G6 Continuous Glucose Monitoring (CGM) System is covered by Medicare for patients who meet the Medicare coverage criteria. Medicare coverage for therapeutic CGM includes certain beneficiaries who have either type 1 or type 2 diabetes and intensively manage their insulin.Jan 31, 2022
Are glucose monitors covered by insurance?
Continuous long-term monitoring for diabetic monitoring of glucose levels is covered when the medical conditions above are met. Intermittent monitoring (up to 72 hours) for diabetic glucose monitoring of type I diabetes is covered when the medical conditions above are met.
Is Livongo covered by Medicare?
The Centers for Medicare and Medicare Services has recognized chronic disease management company Livongo as an enrolled provider for Medicare Advantage members, the startup announced this morning in a release.Apr 30, 2019
What Are Glucose Monitors Used for?
If you have been diagnosed with diabetes, a glucose monitor can help you manage your disease and prevent complications, according to the National I...
Medicare Coverage of Glucose Monitors
Under Original Medicare (Part A and Part B), Part A covers health-care expenses you incur as an inpatient in a hospital, while Part B covers your o...
How Does Medicare Treat Durable Medical Equipment?
Medicare treats glucose monitors and blood sugar test strips as durable medical equipment (DME) under Medicare Part B. If your physician prescribes...
Are There Other Options For Medicare Coverage of Glucose Monitors?
Some Medicare beneficiaries choose to receive their Original Medicare benefits (except hospice care) through the Medicare Advantage (Medicare Part...
Would You Like to Know More About Medicare Coverage of Glucose Monitors?
If you have questions about Medicare coverage for home glucose monitors, or would like more information about Medicare plan options to help you bet...
How long can you have Medicare Part B?
If you’ve had Medicare Part B for longer than 12 months , you can get a yearly “Wellness” visit to develop or update a personalized prevention plan based on your current health and risk factors. This includes:
What is Part B for diabetes?
In addition to diabetes self-management training, Part B covers medical nutrition therapy services if you have diabetes or renal disease. To be eligible for these services, your fasting blood sugar has to meet certain criteria. Also, your doctor or other health care provider must prescribe these services for you.
How often do you have to have your eyes checked for glaucoma?
Part B will pay for you to have your eyes checked for glaucoma once every 12 months if you’re at increased risk of glaucoma. You’re considered high risk for glaucoma if you have:
What is the A1C test?
A hemoglobin A1c test is a lab test that measures how well your blood sugar has been controlled over the past 3 months. If you have diabetes, Part B covers this test if your doctor orders it.
What is diabetes self management training?
Diabetes self-management training helps you learn how to successfully manage your diabetes. Your doctor or other health care provider must prescribe this training for Part B to cover it.
Does Medicare cover diabetes?
This section provides information about Medicare drug coverage (Part D) for people with Medicare who have or are at risk for diabetes. To get Medicare drug coverage, you must join a Medicare drug plan. Medicare drug plans cover these diabetes drugs and supplies:
Does Part B cover insulin pumps?
Part B may cover insulin pumps worn outside the body (external), including the insulin used with the pump for some people with Part B who have diabetes and who meet certain conditions. Certain insulin pumps are considered durable medical equipment.
What is a glucose monitor?
A glucose monitor measures your blood sugar (glucose) levels so you can make informed decisions about eating, exercising, and taking prescription medications, such as insulin. According to the NIH, one way to monitor your glucose levels is by using a finger-stick device to collect a drop of blood, which you put into a glucose monitor on a set schedule each day. An alternative site glucose monitor allows blood samples from areas such as your palm or thigh, according to the Mayo Clinic. As well as a glucose monitor, you may also need other testing supplies, such as lancets, glucose test strips, and a glucose control solution. Medicare coverage of glucose monitors Under Original Medicare (Part A and Part B), Part A covers health-care expenses you incur as an inpatient in a hospital, while Part B covers your outpatient care, including some glucose monitoring supplies and durable medical equipment. Medicare does not generally cover “continuous glucose monitoring,” which (according to the NIH) involves a sensor inserted under your skin for several days to a week. If your health-care provider recommends a different way to monitor your blood sugar other than the finger-stick glucose monitor, you might want to check with Medicare to see whether it’s covered. You can reach a Medicare representative 24 hours a day, seven days a week, if you call 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048. If you have a Medicare Advantage plan, call your plan to ask about this coverage. How does Medicare treat durable medical equipment Continue reading >>
How many pairs of shoes does Medicare cover?
Medicare Part B covers one pair of custom-molded shoes (including inserts) or one pair of depth-inlay shoes per calendar year. Medicare also covers two additional pairs of inserts each calendar year for custom-molded shoes and three pairs of inserts each calendar year for depth-inlay shoes.
What are the preferred test strips for Ascensia?
For Abbott monitors, the preferred test strips include FreeStyle®, FreeStyle Lite®, and Precision Xtra®. For Ascensia monitors, the preferred test strips include Contour®, Contour®NEXT, Breeze®2, Elite®, and Autodisc®. Prior Authorization Required If your patient chooses to use a test strip that is not FreeStyle, FreeStyle Lite, Precision Xtra, Contour, Contour®NEXT, Breeze 2, Elite, or Autodisc, you will need to complete a prior authorization form on your patient’s behalf. If the prior authorization is not approved, the non-preferred test strips will not be a covered pharmacy benefit for your patient, and he or she will be responsible for the entire cost of the test strips. If the request for the non-preferred test strips is approved, your patient will be charged the highest level of cost-sharing. Free Blood Glucose Meters Both Abbott and Ascensia blood glucose meters are available at no cost to our members. Below is a comparison chart of important features of the blood glucose meters and corresponding test strips. The preferred brands rank high in patient satisfaction and can be used in several test sites, as listed below. Abbott Diabetes Care Ascensia Diabetes Care Blood Glucose Meter FreeStyle FreeStyle Freedom Lite Precision Xtra Contour Breeze 2 Contour® Next One Contour® Next EZ Contour® Next Sample size (uL) 0.3 0.3 0.6 0.6 1.0 0.6 0.6 0.6 Test time 5 seconds 5 seconds 5 seconds 5 seconds 5 seconds 5 seconds 5 seconds 5 seconds Approved test sites Fingertip, hand, forearm, upper arm, thigh, calf Fingertip, hand, forearm, Continue reading >>
Does Medicare pay for DME?
Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare. If your doctors or suppliers aren’t enrolled, Medicare won’t pay the claims submitted by them.
Does Medicare pay for blood sugar monitors?
How often is it covered? Medicare Part B (Medical Insurance) covers blood sugar monitors as durable medical equipment (DME) that your doctor prescribes for use in your home. Who's eligible? All people with Part B are covered. Your costs in Original Medicare If your supplier accepts assignment, you pay 20% of the Medicare-approved amount, and the Part B deductible applies. Medicare pays for different kinds of DME in different ways. Depending on the type of equipment: You may need to rent the equipment. You may need to buy the equipment. You may be able to choose whether to rent or buy the equipment. Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare. If your doctors or suppliers aren’t enrolled, Medicare won’t pay the claims submitted by them. It’s also important to ask your suppliers if they participate in Medicare before you get DME. If suppliers are participating suppliers, they must accept assignment. If suppliers are enrolled in Medicare but aren’t “participating,” they may choose not to accept assignment. If suppliers don't accept assignment, there’s no limit on the amount they can charge you. To find out how much your specific test, item, or service will cost, talk to your doctor or other health care provider. The specific amount you’ll owe may depend on several things, like: Other insurance you may have How much your doctor charges Whether your doctor accepts assignment The type of facility The location where you get your test, item, or service Continue reading >>
Does Medicare cover freestyle libre?
Coverage includes all Medicare patients with diabetes who use insulin and who meet the eligibility criteria2. The factory-calibrated FreeStyle Libre system is the only CGM system recognized by Medicare that requires no user calibration whatsoever (either by fingerstick or manual data entry).
Is Accu Chek covered by Medicare?
Stick with the brand you trust—don't let them switch your test strips! Some test strip suppliers may tell you otherwise, but Accu-Chek products are still covered by Medicare Part B at the same low co-pay1 as all other brands.2 They may even try switching you to another brand.
What percentage of Medicare deductible is covered for glucose monitoring?
If your physician prescribes glucose monitoring at home, your durable medical equipment costs are generally covered at 80 percent of the Medicare-approved. amount, once your deductible is met.
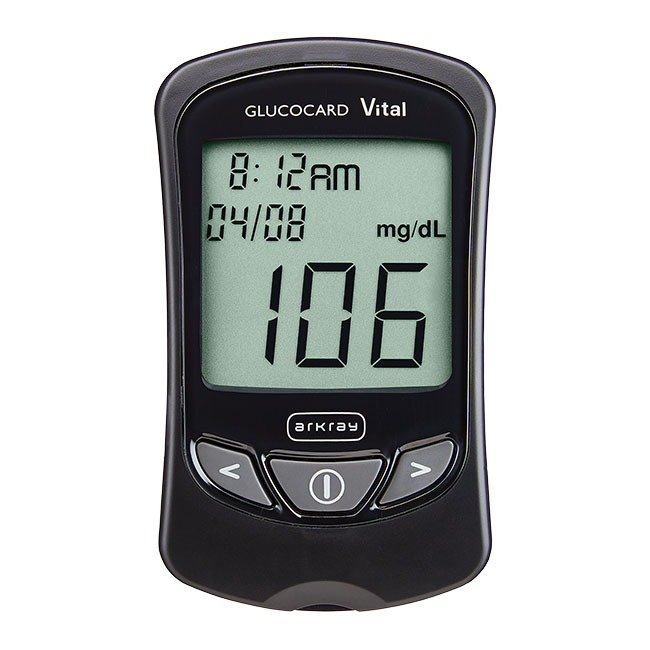
What is a glucose monitor?
A glucose monitor measures your blood sugar (glucose) levels so you can make informed decisions about eating, exercising, and taking prescription medications, such as insulin.
How to monitor glucose levels?
According to the NIH, one way to monitor your glucose levels is by using a finger-stick device to collect a drop of blood, which you put into a glucose monitor on a set schedule each day. An alternative site glucose monitor allows blood samples from areas such as your palm or thigh, according to the Mayo Clinic.
Does Medicare cover glucose monitoring?
Medicare does not generally cover “ continuous glucose monitoring,” which (according to the NIH) involves a sensor inserted under your skin for several days to a week. If your health-care provider recommends a different way to monitor your blood sugar other than the finger-stick glucose monitor, you might want to check with Medicare ...
Does Medicare cover hospice?
Part A covers hospice care when you have a Medicare Advantage plan. Medicare Advantage plans cover glucose monitors in the same way as Medicare Part B and often offer additional benefits, such as vision, dental, and prescription drug coverage. Some types of Medicare Advantage plans use provider networks, and may reduce the amounts you pay ...
What is a glucose monitor?
A glucose monitor measures your blood sugar (glucose) levels so you can make informed decisions about eating, exercising, and taking prescription medications, such as insulin. According to the NIH, one way to monitor your glucose levels is by using a finger-stick device to collect a drop of blood, which you put into a glucose monitor on a set schedule each day. An alternative site glucose monitor allows blood samples from areas such as your palm or thigh, according to the Mayo Clinic. As well as a glucose monitor, you may also need other testing supplies, such as lancets, glucose test strips, and a glucose control solution. Medicare coverage of glucose monitors Under Original Medicare (Part A and Part B), Part A covers health-care expenses you incur as an inpatient in a hospital, while Part B covers your outpatient care, including some glucose monitoring supplies and durable medical equipment. Medicare does not generally cover “continuous glucose monitoring,” which (according to the NIH) involves a sensor inserted under your skin for several days to a week. If your health-care provider recommends a different way to monitor your blood sugar other than the finger-stick glucose monitor, you might want to check with Medicare to see whether it’s covered. You can reach a Medicare representative 24 hours a day, seven days a week, if you call 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048. If you have a Medicare Advantage plan, call your plan to ask about this coverage. How does Medicare treat durable medical equipment Continue reading >>
What supplies does Medicare cover?
HEALTH FEATURE ARCHIVE Diabetes Supplies: What Medicare Covers 1. Self-testing equipment and supplies: Medicare Part B covered diabetes supplies: Coverage for glucose monitors, test strips, and lancets. Who is covered: All people with Medicare who have diabetes (insulin users and non-users). Medicare covers the same supplies for people with diabetes whether or not they use insulin. These include glucose testing monitors, blood glucose test strips, lancet devices and lancets, and glucose control solutions. There may be some limits on supplies or how often you get them. For more information about diabetic supplies, call your Durable Medical Equipment Regional Carrier. How to get your diabetes equipment and supplies: To get your diabetes equipment and supplies under Medicare, you need a prescription from your doctor. The prescription should say: You have been diagnosed with diabetes. How many test strips and lancets you need in a month. What kind of meter you need. For example, if you need a special meter for vision problems, the doctor should say that and state the medical reason why you need a special meter. Whether you use insulin or not. How often you should test your blood sugar. Points to remember: Ask your doctor or health care provider if regular blood sugar testing is right for you. You need a prescription from your doctor to get your diabetes equipment and supplies under Medicare. Learn the correct way to use your blood sugar meter properly. Your pharmacist, doctor, diabetes educator, or another health care provider can help you. Keep track of your blood sugar readings and share them with your doctor or health care provider at regular visits. Do not accept shipments of diabetes equipment and supplies that you did not ask for. 2. Therapeutic shoes: Medicare also c Continue reading >>
What is Medicare Part C?
If you have a Medicare Part C Medicare Advantage plan: Medicare Part C Medicare Advantage plans, also called Medicare Advantage plans, must cover everything that's included in original Medicare Part A and Part B coverage. But sometimes a Part C plan covers more, with extra services or an expanded amount of coverage.
How many pairs of shoes does Medicare cover?
Medicare Part B covers one pair of custom-molded shoes (including inserts) or one pair of depth-inlay shoes per calendar year. Medicare also covers two additional pairs of inserts each calendar year for custom-molded shoes and three pairs of inserts each calendar year for depth-inlay shoes.
Does Medicare cover insulin?
Who is covered: All people with Medicare who have diabetes (insulin users and non-users). Medicare covers the same supplies for people with diabetes whether or not they use insulin. These include glucose testing monitors, blood glucose test strips, lancet devices and lancets, and glucose control solutions.
Does Medicare cover diabetes meters?
If you're diagnosed with diabetes and prescribed a meter, Medicare covers it. Most meters are free, whether or not Medicare covers them. The details Medicare needs about your monitoring equipment, lancets and test strips are covered in the next section.
Can I order diabetes supplies through mail order?
The Medicare rules for ordering diabetes supplies through a mail-order pharmacy have changed. Here is the information you need to know to make this transition smoothly. On July 1, a Medicare rule took effect that impacts beneficiaries who get their diabetes testing supplies via mail order. It’s referred to as the Medicare National Mail-Order Program. Under the new ruling, beneficiaries must buy their diabetes supplies, including blood glucose trips, lancets, lancet devices, batteries and control solution, through a list of designated vendors, or Medicare national mail-order contract suppliers. Beneficiaries who pick up their testing supplies from a local pharmacy can still do so, but they need to make sure that the store accepts Medicare "assignment" to avoid higher charges for the supplies. At Joslin Diabetes Center, we are closely monitoring this new program which is intended to be a cost-cutting measure. If you have questions or difficulties navigating the new system, we provided you with additional details to ensure the program is not a disruption to your diabetes care. Who is affected? Medicare beneficiaries in all 50 states, D.C., Puerto Rico, the U.S. Virgin Islands, Guam, and American Samoa, who have Original Medicare, are impacted. These changes do not apply to Medicare Advantage plans (like an HMO or PPO). If you are enrolled in a private plan through Medicare, you can contact your plan to find out which suppliers you can use. How can I get my supplies? If you want diabetes testing supplies delivered to your home, you must use an approved Medicare national mail-order contract supplier in order for Medicare to help pay for the supplies. To find a contract supplier, you can call 1-800-MEDICARE (1-800-633-4227) or visit www.medicare.gov/supplier. Alternatively, Continue reading >>
What is a glucose monitor?
A glucose monitor measures your blood sugar (glucose) levels so you can make informed decisions about eating, exercising, and taking prescription medications, such as insulin. According to the NIH, one way to monitor your glucose levels is by using a finger-stick device to collect a drop of blood, which you put into a glucose monitor on a set schedule each day. An alternative site glucose monitor allows blood samples from areas such as your palm or thigh, according to the Mayo Clinic. As well as a glucose monitor, you may also need other testing supplies, such as lancets, glucose test strips, and a glucose control solution. Medicare coverage of glucose monitors Under Original Medicare (Part A and Part B), Part A covers health-care expenses you incur as an inpatient in a hospital, while Part B covers your outpatient care, including some glucose monitoring supplies and durable medical equipment. Medicare does not generally cover “continuous glucose monitoring,” which (according to the NIH) involves a sensor inserted under your skin for several days to a week. If your health-care provider recommends a different way to monitor your blood sugar other than the finger-stick glucose monitor, you might want to check with Medicare to see whether it’s covered. You can reach a Medicare representative 24 hours a day, seven days a week, if you call 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048. If you have a Medicare Advantage plan, call your plan to ask about this coverage. How does Medicare treat durable medical equipment Continue reading >>
What supplies are covered by Medicare Part B?
These supplies include: Blood glucose self-testing equipment and supplies Therapeutic shoes and inserts Insulin pumps and the insulin used in the pumps Blood Glucose Self-testing Equipment and Supplies Blood glucose self-testing equipment and supplies are covered for all people with Medicare Part B who have diabetes.
Does Railroad Medicare cover insulin?
Railroad Medicare covers certain supplies if you have Medicare Part B and have diabetes. These supplies include: Blood glucose self-testing equipment and supplies Therapeutic shoes and inserts Insulin pumps and the insulin used in the pumps Blood Glucose Self-testing Equipment and Supplies Blood glucose self-testing equipment and supplies are covered for all people with Medicare Part B who have diabetes. This includes those who use insulin and those who do not use insulin. These supplies include: Blood glucose monitors Blood glucose test strips Lancet devices and lancets Glucose control solutions for checking the accuracy of testing equipment and test strips Railroad Medicare covers the same type of blood glucose testing supplies for people with diabetes whether or not they use insulin. However, the amount of supplies that are covered varies. If you: Use insulin, you may be able to get up to 100 test strips and lancets every month, and 1 lancet device every 6 months Do not use insulin, you may be able to get 100 test strips and lancets every 3 months, and 1 lancet device every 6 months If your doctor documents why it is medically necessary, Railroad Medicare will cover additional test strips and lancets for you. Medicare and Railroad Medicare will only cover blood glucose self-testing equipment and supplies if you get a prescription from your doctor which includes: That you have diabetes What kind of blood glucose monitor you need and why Whether or not you use insulin How often you need to test your blood glucose Medicare will not pay for any supplies not asked for, or for any supplies that were sent to a beneficiary automatically from suppliers. This includes blood glucose monitors, test strips, and lancets. Also, if a beneficiary goes to a pharmacy or supplier that i Continue reading >>
Does Medicare cover CGMs?
One Voice Working to Ensure Medicare Coverage of Continuous Glucose Monitors (CGMs) Thanks to extensive advocacy by JDRF volunteers and staff, clinician support, and strong bipartisan support from Congress, the Centers for Medicare & Medicaid Services (CMS) determined recently that continuous glucose monitoring (CGM) devices that are approved for use in treatment decisions are eligible for Medicare coverage. (For more information, please see our JDRF blog and press release.) This decision is a victory for people with type 1 diabetes (T1D) who are on Medicare or will be aging into Medicare. It is also a victory for the entire T1D community as broader coverage creates an incentive for innovation. On behalf of JDRF and all those affected by T1D, we ask that you please take a moment to thank your U.S. Senators and also thank your U.S. Representative for their timely work on this issue. For a couple of years, the leadership of the Senate Diabetes Caucus and the Congressional Diabetes Caucus has been working tirelessly to ensure Medicare coverage of CGMs, which are currently covered by more than 95 percent of private health plans. These Members of Congress and their colleagues deserve our recognition and our appreciation for co-sponsoring the ‘Medicare CGM Access Act of 2015’ (S. 804 and H.R. 1427), as introduced by Senators Collins and Shaheen, and Representatives Reed and DeGette. A successful 2016 ended with 50 Senators on the Senate bill and 275 Representatives on the House companion version. Congress will not need to reintroduce and enact legislation now that there is finally a favorable Medicare coverage decision. CGMs have a medical purpose, and have been recognized as such by Medicare CGMs are U.S. Food & Drug Administration (FDA)-approved, physician-prescribed de Continue reading >>
Does Medicare cover blood glucose screening?
Medicare covers blood tests to screen for diabetes if you are at risk for diabetes or have pre-diabetes. You are eligible for one Medicare-covered diabetes screening every 12 months if you: have hypertension; have dyslipidemia (any kind of cholesterol problem); have a prior blood test showing low glucose (sugar) tolerance; are obese (body mass index of 30 or more); or meet at least two of the following: you are overweight (body mass index between 25 and 30); you have a family history of diabetes; you have a history of diabetes during pregnancy (gestational diabetes) or have had a baby over nine pounds; or you are 65 years of age or older. The Medicare-covered diabetes screening test includes: a fasting blood glucose tests; and/or a post-glucose challenge test. If you have been diagnosed with pre-diabetes, Medicare will cover two diabetes screening tests a calendar year. Having pre-diabetes means you have blood glucose (sugar) levels that are higher than normal, but are not high enough to be classified as diabetes. Medicare will pay for 100% of its approved amount for the test even before you have met the Part B deductible. You will pay no copay or deductible for these tests if you see doctors who take assignment. Doctors and other health care providers who take assignment cannot charge you more than the Medicare approved amount. Medicare Advantage Plans cover all preventive services the same as Original Medicare. This means Medicare Advantage Plans will not be allowed to charge cost-sharing fees (coinsurances, copays or deductibles) for preventive services that Original Medicare does not charge for as long as you see in-network providers. If you see providers that ar Continue reading >>
Does Medicare pay for blood sugar monitors?
How often is it covered? Medicare Part B (Medical Insurance) covers blood sugar monitors as durable medical equipment (DME) that your doctor prescribes for use in your home. Who's eligible? All people with Part B are covered. Your costs in Original Medicare If your supplier accepts assignment, you pay 20% of the Medicare-approved amount, and the Part B deductible applies. Medicare pays for different kinds of DME in different ways. Depending on the type of equipment: You may need to rent the equipment. You may need to buy the equipment. You may be able to choose whether to rent or buy the equipment. Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare. If your doctors or suppliers aren’t enrolled, Medicare won’t pay the claims submitted by them. It’s also important to ask your suppliers if they participate in Medicare before you get DME. If suppliers are participating suppliers, they must accept assignment. If suppliers are enrolled in Medicare but aren’t “participating,” they may choose not to accept assignment. If suppliers don't accept assignment, there’s no limit on the amount they can charge you. To find out how much your specific test, item, or service will cost, talk to your doctor or other health care provider. The specific amount you’ll owe may depend on several things, like: Other insurance you may have How much your doctor charges Whether your doctor accepts assignment The type of facility The location where you get your test, item, or service Continue reading >>
Is CGM covered by Medicare?
Huuuuge news in the Diabetes Community!!! In a surprise move late last week, the Centers for Medicare and Medicaid Services (CMS) issued a policy decision allowing for certain continuous glucose monitors (CGM) to be covered under Medicare! This important 16-page ruling on Jan. 12 came after business hours on the East Coast, and it was the JDRF -- one of the organizations that's led advocacy efforts on this issue for several years -- that put the word out right away among the D-Community. There are several reasons why this is a really big deal: CGM is a powerful therapy tool, one that can in particular save lives of people who experience hypoglycemia unawareness, or have dramatic highs and lows. SO naturally, it should be covered by insurance With Medicare refusing to cover it, patients using CGM who hit Medicare age were suddenly losing access to this important tool, which is nonsensical and frankly, unethical Classifying CGM as core therapy rather than "supplemental" paves the way not only for broader coverage of CGM across the board, but also for Artificial Pancreas systems on the near horizon What Exactly Has Changed: Up until now, CMS has considered CGM technology to be "precautionary," meaning it was classified as a supplemental type of device that wasn't medically necessary. CGM also didn't fall under the "Durable Medical Equipment" category that covers other diabetes devices and supplies, therefore it wasn't eligible for Medicare coverage. That now changes. A critical step that led to this CMS decision was the FDA's ruling in December that the Dexcom G5 specifically is accurate enough to be used for insulin dosing and treatment decisions. Thanks to that landmark FDA decision, the Medicare and Medicaid agency could now consider CGM "therapeutic" and classify it as Continue reading >>
What does Medicare cover?
Medicare covers various diabetes medications, supplies and services to help treat diabetes and keep your blood glucose in a healthy range. Medicare Part B covers blood glucose testing and other supplies you may need plus some medical and education services. Medicare Part D covers diabetes medications and supplies for injecting or inhaling insulin.
What does Medicare Advantage cover?
Medicare Advantage plans (Part C) cover diabetes supplies and services, too, and often additional services such as vision, dental and hearing care. The costs and items covered will depend on the specific plan you have.
What supplies are covered by Medicare Part D?
Diabetes Supplies and Services Covered by Medicare Part D. Medications to manage blood glucose. Insulin taken by injection. Supplies for taking insulin by injection (syringes, needles, alcohol swabs and gauze) Inhaled insulin.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
Does Medicare cover insulin?
Medicare Part D covers diabetes medications and supplies for injecting or inhaling insulin. Here’s a rundown of the diabetes supplies and services that Medicare covers. Some require a prescription or recommendation from your doctor. Coverage limits may include the amount of some supplies you can get or how often some services are covered.