
Does Medicare cover CPAP supplies?
Offer helpful instructions and related details about Cpap Providers That Accept Medicare - make it easier for users to find business information than ever. Top Companies. How To Change Main Desktop Screen Setup External Monitor For Laptop ... Cpap Mask Suppliers Near Me ...
What is Medicare’s improved supplier directory?
After you meet the Part B deductible , you pay 20% of the Medicare-Approved Amount for the machine rental and purchase of related supplies (like masks and tubing). Medicare pays the supplier to rent a CPAP machine for 13 months if you’ve been using it without interruption. After Medicare makes rental payments for 13 continuous months, you’ll own the machine.
Will Medicare pay for a PAP device?
Mar 19, 2017 · The CPAP supplies (the DME or HME company) can provide the objective data either though a direct data download (learn more about smart CPAP machines here) or through a visual inspection of the usage data documentation provided in a written report that is reviewed by the physician and included in the patient’s medical record. Many other insurance companies …
How does Medicare define compliance with PAP?
Aug 13, 2021 · Unfortunately, CPAP cleaners and sanitizers aren’t covered by Medicare; however, they are eligible to purchase with your HSA/FSA funds! CPAPsupplies.com offers a wide selection of CPAP cleaners at the lowest prices, so an affordable sanitizer may still be in your budget.
Does CPAP com take Medicare?
What is the Medicare approved amount for a CPAP machine?
How often will Medicare pay for a new CPAP?
Do Medicare Advantage plans cover CPAP machines?
Can you claim CPAP machine on Medicare Australia?
What is better than a CPAP machine?
How many apneas per hour is severe?
How often should you change your CPAP mask and hose?
How many years does a CPAP machine last?
Does Medicare Part B pay for CPAP machine?
How do you qualify for a CPAP machine?
Will Medicare replace my recalled CPAP machine?
Does Medicare Cover CPAP and Other Pap Therapy For Sleep Apnea?
Yes. Medicare covers a 3-month trial of for CPAP therapy (learn more about CPAP here) if you’ve been diagnosed wtih obstructive sleep apnea (learn...
How Does Medicare Define CPAP Compliance Or Adherence?
Medicare defines adherence as using the device more than 4 hours per night for 70% of nights (that’s 21 nights) during a consecutive 30 day period...
What Is The Rental Term For Pap Therapy?
If the 3-month trial is successful (see above) Medicare will continue to cover the PAP device on a rental basis for up to 13 months in total up to...
Will Medicare Cover CPAP If I had A Machine Before I Got Medicare?
Yes, Medicare may cover rental or a replacement CPAP machine and/or CPAP supplies if you meet certain requirements.
When Does Medicare Cover Bi-Level Or Bipap?
Medicare will cover a bi-level respiratory assist device without backup (this is what they call a bi-level or BiPAP) for patients with obstructive...
What Is Required in The Initial Face-To-Face Clinical Evaluation?
Written entries of the evaluation may include:History 1. Signs and symptoms of sleep disordered breathing including snoring, daytime sleepiness, ob...
What Information Does Medicare Require on The Prescription For CPAP and Supplies?
1. Beneficiary/patient’s name 2. Treating physician’s name 3. Date of order 4. Detailed description of items (type of device and supplies, pressure...
How Often Does Medicare Cover Replacement Pap Supplies?
Here’s an outline of the Medicare supply replacement schedule. For more detail (including how to tell when your equipment needs to be replaced, che...
How Much Will Medicare Pay For A CPAP Or Other Pap Machine?
Medicare will pay 80% of the Medicare-approved amount for a PAP device after you’ve met your Part B deductible (learn about this and other insuranc...
Does Medicare cover CPAP?
Yes. Medicare covers a 3-month trial of for CPAP therapy (learn more about CPAP here) if you’ve been diagnosed wtih obstructive sleep apnea (learn more about OSA here) and meet one of the following criteria: AHI or RDI > 15 events per hour with a minimum of 30 events or. AHI or RDI > 5 to14 events per hour with a minimum ...
Does Medicare cover bi level respiratory assist?
Medicare will cover a bi-level respiratory assist device without backup (this is what they call a bi-level or BiPAP) for patients with obstructive sleep apnea if the patient meets the criteria for PAP therapy (outlined above) and:
How many events per hour is AHI?
AHI or RDI > 15 events per hour with a minimum of 30 events or. AHI or RDI > 5 to14 events per hour with a minimum of 10 events recorded and documentation of: Excessive daytime sleepiness, impaired cognition, mood disorders or insomnia; or. Hypertension, ischemic heart disease or history of stroke.
Does Medicare cover CPAP?
Wait, does Medicare cover CPAP supplies? Really?! Yes, and they may cover a new CPAP machine too, if yours is older than five years old. You just have to be diagnosed with sleep apnea and follow Medicare’s guidelines.
Why do you need to replace CPAP supplies?
Because your CPAP supplies must be replaced on a regular basis to keep your CPAP working like new. Plus, this is crucial to keeping your equipment free of viruses, germs, or other harmful pathogens and prevents air leaks.
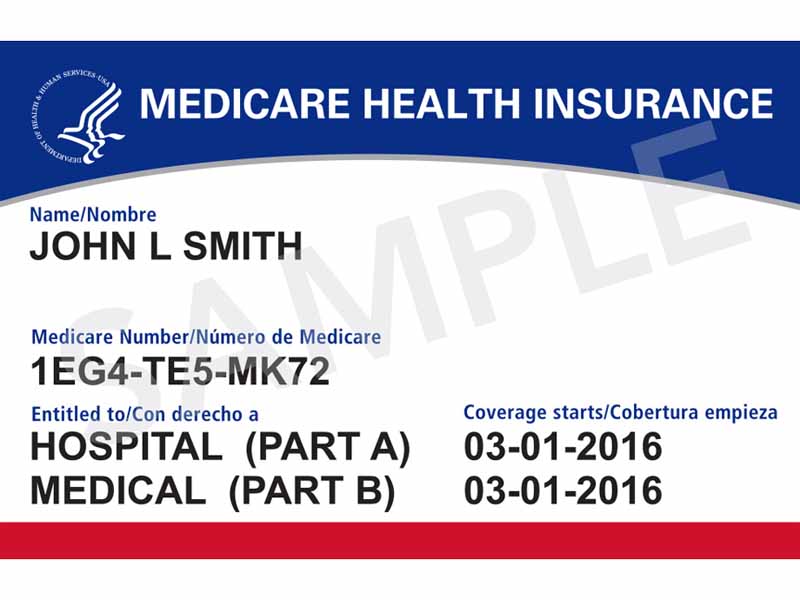
How old do you have to be to get Medicare?
To enroll you must be age 65 or older and you must be a U.S. citizen or a permanent resident for five consecutive years. You may automatically enroll in Medicare part A if you already receive benefits from Social Security or the Railroad Retirement Board (RRB).
What is a sleep study?
A Home Sleep Study: A home sleep study is a sleep apnea test that you can take in the comfort of your own bed. You receive the test in the mail and wear a pulse oximeter overnight. In the morning repackage the test and send it back. Then a qualified sleep technician will evaluate your results.
Does Medicare cover CPAP?
Medicare does cover CPAP machine therapy if you are diagnosed with sleep apnea. You may be eligible for sleep apnea treatment options if you are enrolled in Medicare Part B and have been diagnosed with obstructive sleep apnea. If you have been formally diagnosed with sleep apnea, you are likely eligible for a 3-month trial of CPAP therapy.
How long is a CPAP trial?
If you have been formally diagnosed with sleep apnea, you are likely eligible for a 3-month trial of CPAP therapy. If the therapy is successful, your doctor can extend the treatment and Medicare will cover it.
What is the best treatment for sleep apnea?
A continuous positive airway pressure (CPAP) machine is the most common treatment for moderate to severe sleep apnea. The machine is equipped with a mask that blows air into your throat while you are sleeping to keep your airway ...
Who is Christian Worstell?
Or call 1-800-995-4219 to speak with a licensed insurance agent. Christian Worstell is a health care and policy writer for MedicareSupplement.com. He has written hundreds of articles helping people better understand their Medicare coverage options.
Does Medicare cover CPAP?
You must get the CPAP equipment from a Medicare-assigned supplier for Medicare to cover it. If your health-care provider decides that the sleep apnea therapy is helping, you may continue to be covered under Medicare for a longer period.
How long does Medicare pay for a CPAP machine?
Medicare pays the supplier to rent the CPAP machine for up to 13 months, and after that, the CPAP machine is considered yours.
Is sleep apnea covered by Medicare?
If your health-care provider decides that the sleep apnea therapy is helping, you may continue to be covered under Medicare for a longer period. To avoid possible extra costs, you might want to make sure your CPAP machine is medically necessary according to your Medicare-assigned doctor.
What is the Medicare Part B deductible?
As mentioned, with Medicare Part B, you will be responsible for paying 20% of the Medicare-approved amount to rent a CPAP device and necessary parts or accessories, and the Part B deductible applies.
How long is a CPAP trial?
If you have Medicare and you’re diagnosed with obstructive sleep apnea, you may be eligible to receive Continuous Positive Airway Pressure (CPAP) therapy for a three-month trial period. With Medicare Part B, you’ll pay 20% of the Medicare-approved amount for the CPAP machine rental and supplies, after reaching ...
