What glucose meters does Medicare cover?
Medicare covers therapeutic continuous glucose monitors and related supplies instead of blood sugar monitors for making diabetes treatment decisions, like changes in diet and insulin dosage. If you use insulin and require frequent adjustments to your insulin regimen/dosage, Medicare may cover a continuous glucose monitor if your doctor determines that you meet all of the …
What glucometer is covered by Medicare?
Jan 16, 2022 · Beginning Feb. 28, 2022, those using a Medtronic CGM integrated with the company’s MiniMed insulin pumps will be able to get Medicare coverage for their transmitters, sensors and supplies.
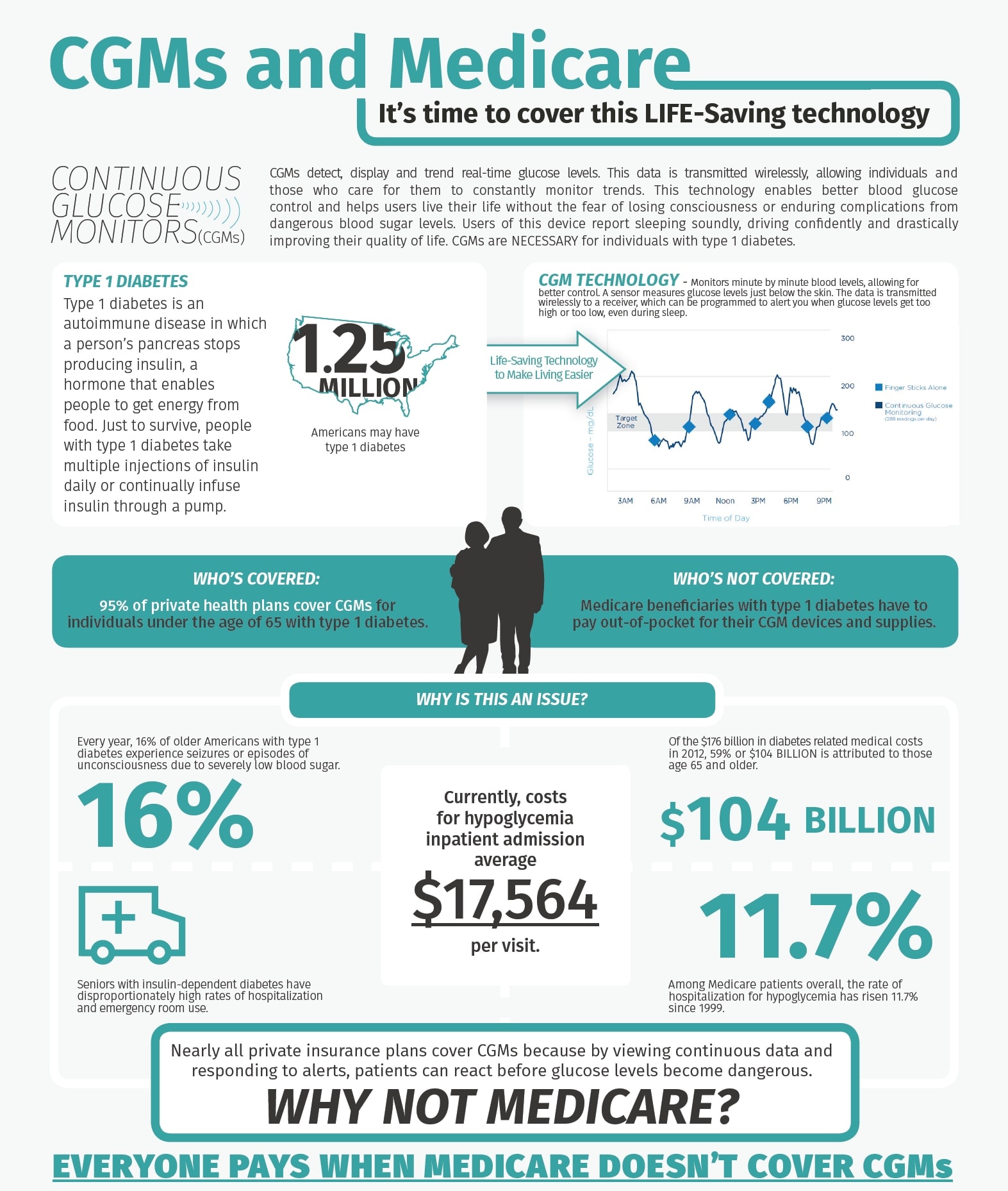
Are CGMS covered by Medicare?
Beginning on July 18, 2021, Medicare will permanently eliminate the requirement of the four-time-daily fingerstick in order to qualify for coverage of a continuous glucose monitor (CGM). This requirement was an unnecessary barrier for Medicare beneficiaries, delaying access to this effective technology for individuals with diabetes. CGMs provide users with real-time, dynamic …
Does Medicare cover continuous glucose monitors (CGM)?
Nov 23, 2021 · The Dexcom G6 Continuous Glucose Monitoring System is covered by Medicare for patients who meet the Medicare coverage criteria. Medicare coverage for therapeutic CGM includes certain beneficiaries who have either type 1 or …
Does Medicare cover any CGM?
Yes. The Dexcom G6 Continuous Glucose Monitoring (CGM) System is covered by Medicare for patients who meet the Medicare coverage criteria. Medicare coverage for therapeutic CGM includes certain beneficiaries who have either type 1 or type 2 diabetes and intensively manage their insulin.Jan 31, 2022
What brand of CGM does Medicare cover?
Medicare Part B covers therapeutic continuous glucose monitors (CGM) such as the Freestyle Libre 2 and the Dexcom G6 for people with diabetes. Medicare covers therapeutic continuous glucose monitors as durable medical equipment (DME).
How much does CGM cost with Medicare?
Q: How much does CGM cost for Medicare users? A: According to Dexcom's Medicare FAQ page, those covered by Medicare can expect to pay 20% of the costs of their G5 CGM, which is roughly $50 per month. (This may be covered by secondary insurance.) Medicare will cover the remaining 80%.Jun 15, 2018
What is the Medicare criteria for a CGM?
The Four Criteria Have a diagnosis of diabetes, either type 1 or type 2. Use a home blood glucose monitor (BGM) and conduct four or more daily BGM tests. Be treated with insulin with multiple daily injections or a constant subcutaneous infusion (CSI) pump.Nov 7, 2017
Is FreeStyle Libre covered under Medicare Part B?
Medicare covers CGMs like the FreeStyle Libre under the durable medical equipment (DME) portion of Medicare Part B, provided you meet eligibility criteria. If you qualify for coverage for the monitor, Medicare will also cover your supplies within certain limits.Sep 30, 2021
Does Medicare cover Livongo?
In addition, the company's diabetes management program will soon be available to qualifying Cambia Health Solution members.Apr 30, 2019
Do you need a smartphone for a continuous glucose monitor?
Dexcom's G5 Mobile is the only continuous glucose monitoring system that meets Medicare criteria for coverage.Mar 28, 2017
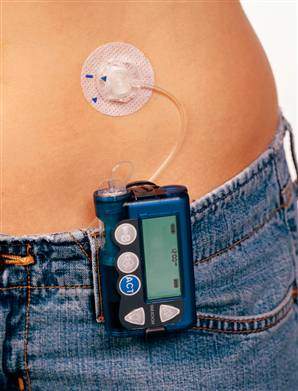
Are insulin pumps covered by Medicare?
Part B. Medicare Part B covers a portion of an insulin pump and the insulin costs, as long as your doctor prescribes it and it meets Medicare's requirements.Jul 31, 2020
What is the monthly cost of FreeStyle Libre?
Most commercially insured patients end up paying between $0 to $60 per month for FreeStyle Libre 2 sensors,§1 and no more than $65 for a FreeStyle Libre 2 reader.
Does Medicare Part B cover CGM?
Medicare also covers therapeutic continuous glucose monitors (CGMs) approved for use in place of blood sugar monitors for making diabetes treatment decisions (like, changes in diet and insulin dosage) and related supplies.
When did Medicare approve CGM?
New Medicare Coverage Requirements Make CGMs More Accessible Beginning on July 18, 2021, Medicare will permanently eliminate the requirement of the four-time-daily fingerstick in order to qualify for coverage of a continuous glucose monitor (CGM).
Is CGM covered by insurance?
CGMs have been around for years, but the new models are better than ever, and are covered by Medicare and most private insurance.
How long can you have Medicare Part B?
If you’ve had Medicare Part B for longer than 12 months , you can get a yearly “Wellness” visit to develop or update a personalized prevention plan based on your current health and risk factors. This includes:
What is Part B for diabetes?
In addition to diabetes self-management training, Part B covers medical nutrition therapy services if you have diabetes or renal disease. To be eligible for these services, your fasting blood sugar has to meet certain criteria. Also, your doctor or other health care provider must prescribe these services for you.
What is part B?
Part B covers a once-per-lifetime health behavior change program to help you prevent type 2 diabetes. The program begins with weekly core sessions in a group setting over a 6-month period. In these sessions, you’ll get:
What is diabetes self management training?
Diabetes self-management training helps you learn how to successfully manage your diabetes. Your doctor or other health care provider must prescribe this training for Part B to cover it.
Does Medicare cover diabetes?
This section provides information about Medicare drug coverage (Part D) for people with Medicare who have or are at risk for diabetes. To get Medicare drug coverage, you must join a Medicare drug plan. Medicare drug plans cover these diabetes drugs and supplies:
What is the A1C test?
A hemoglobin A1c test is a lab test that measures how well your blood sugar has been controlled over the past 3 months. If you have diabetes, Part B covers this test if your doctor orders it.
What is coinsurance in insurance?
Coinsurance: An amount you may be required to pay as your share of the cost for services after you pay any deductibles. Coinsurance is usually a percentage (for example, 20%).