The CPT codes used to report urinalysis are as follows: 81000 Urinalysis, by dip stick or tablet reagent for bilirubin, glucose, hemoglobin, ketones, leukocytes
White blood cell
White blood cells are the cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. All white blood cells are produced and derived from multipotent cells in the bone marrow known as hematopoietic stem cells. Leukocytes are found throughout the body, including the blood and lymphatic system.
- CPT CODES and Description.
- 81000 Urinalysis, by dip stick or tablet reagent for bilirubin, glucose, hemoglobin, ketones, leukocytes, nitrite, pH, protein, specific gravity, urobilinogen, any number of these constituents; non-automated, with microscopy.
What modifiers can be used with CPT code for urinalysis?
Routine urinalysis is coded to CPT 81002 Guidelines to use Modifier with CPT code for Urinalysis: Below are the list of modifiers that can be used with CPT code of Urinalysis. 22, 52, 59, 90, 91, 99, AR, CR, ET, GA, GC, GR, GY, GZ, KX, Q0, Q5, Q6, QJ, QP, XE, XP, XS, XU
Do you get paid for 81000 urinalysis codes?
We are paid for 81000 urinalysis (the only one we do in-office) and E/M codes. We are starting to notice Medicare denials for 81000 and E/M but for the reason of "no medical necessity." This is especially true in the case of prostate CA or elevated PSA.
What is the CPT code for urobilinogen?
CPT CODES and Description 81000 Urinalysis, by dip stick or tablet reagent for bilirubin, glucose, hemoglobin, ketones, leukocytes, nitrite, pH, protein, specific gravity, urobilinogen, any number of these constituents; non-automated, with microscopy
When does a physician order a urinalysis?
Physician orders for urinalysis when a patient shows symptoms such as blood in urine, low back pain, abdominal pain, frequent urination, painful urination or cloudy urine. Urine sample is collected directly into a sample cup and analysis is done in laboratory by lab technician.

What ICD 10 code covers urinalysis?
Unspecified abnormal findings in urine R82. 90 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes. The 2022 edition of ICD-10-CM R82. 90 became effective on October 1, 2021.
What diagnosis will cover a urinalysis?
Healthcare providers often use urinalysis to screen for or monitor certain common health conditions, such as liver disease, kidney disease and diabetes, and to diagnose urinary tract infections (UTIs).
What ICD 10 codes cover urine culture?
Unspecified abnormal findings in urinemicrobiological examination R82.79 (culture)positive culture R82.79.
What is the code for urinalysis?
377200: Urinalysis, Complete With Microscopic Examination With Reflex to Urine Culture, Comprehensive | Labcorp.
Does Medicare cover a urinalysis?
Urinalysis is one of the laboratory services covered under Part B. Medicare benefits also include blood tests, screening tests and some tissue specimen testing. To be covered, the test must be medically necessary, ordered by a qualified health care practitioner and performed by a Medicare-approved laboratory.
Why does Medicare not pay for urinalysis?
Urine screenings for employment and other non-medical reasons would not be eligible for coverage under Medicare benefits. With Medicare Part B coverage, most medically necessary diagnostic tests do not require copays or coinsurances. Part A benefits cover diagnostic tests for inpatient hospital stays.
What is the CPT code for a urine culture?
If culture is positive, CPT code(s): 87088 (each isolate) will be added with an additional charge. Identification will be performed at an additional charge (CPT code(s): 87077 or 87140 or 87143 or 87147 or 87149).
Does Medicare pay for CPT 81002?
Medicare has not paid any of our 81002, 85610 services, they paid the E/M = 99214, 99213 or 99215's.
Does Medicare cover CPT code 81002?
All services billed to Medicare must be documented as billed and be medically necessary. CPT codes 81002, 81025, 82270, 82272, 82962, 83026, 84830, 85013, and 85651 do not require a QW modifier to be recognized as a waived test.
Which code set would be used to assign a code for a patient's urinalysis?
It is common practice to do a urinalysis prior to a urine culture. CPT code 81000-81003 are used for dip stick urinalysis.
What is included in a complete urinalysis?
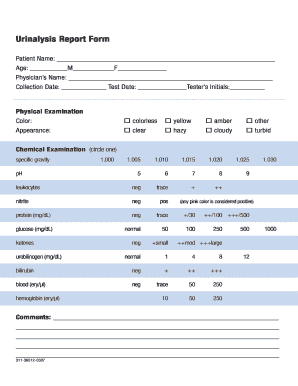
A complete urinalysis will typically include a visual (also called physical) examination, a microscopic examination, and a chemical dipstick test, each of which involves different measurements and evaluations.
What is the CPT code for urinalysis dipstick?
81000-81003CPT Code For Urinalysis Dipstick There are four CPT codes 81000-81003 that include dipstick methods. CPT 81001 or CPT 81003 are automated and prints directly generated by the machines, while for CPT 81000 and CPT 81002 method documentation leads to documentation done by the provider.
What are 4 types of tests done on urine?
Examples of specific urinalysis tests that may be done to check for problems include:Red blood cell urine test.Glucose urine test.Protein urine test.Urine pH level test.Ketones urine test.Bilirubin urine test.Urine specific gravity test.
What can be found in a urine test?
Urine tests are most commonly done to check:for infections – such as a urinary tract infection (UTI) or some sexually transmitted infections (STIs) such as chlamydia in men.if you are passing any protein in your urine as a result of kidney damage – this is known as an ACR test.
Does a urinalysis show STDS?
Sexually Transmitted Infections (STIs) A urinalysis can give clues to the presence of sexually transmitted infections. A positive dipstick for leukocyte esterase or increased numbers of white blood cells in the microscopic exam is suggestive of chlamydia or gonoccocal infection.
Which finding in a urinalysis would indicate the presence of a urinary tract infection?
Infection: The presence of nitrates or leukocyte esterase are found in urine, it could indicate a urinary tract infection.
What are the components of a urinalysis?
The components of a urinalysis include an evaluation of physical characteristics (color, odor, and opacity); determination of specific gravity and pH; detection and measurement of protein, glucose, and ketone bodies; and examination of sediment for blood cells, casts, and crystals. Some laboratories include screening for leukocyte esterase ...
What is the best way to perform urinalysis?
Urinalysis can be performed either by automated instruments or the use of tablets, tapes or dipsticks. Dipsticks are chemically impregnated reagent (reactive) strips that allow for quick determination of pH, protein, glucose, ketones, bilirubin, hemoglobin, nitrate, leukocyte esterase, and urobilinogen. The tip of the dipstick is impregnated ...
What is the pH of a urobilinogen?
Normally, the color is straw to dark yellow, specific gravity 1.005-1.035, pH 4.5-8.0, normal urobilinogen, and negative for protein, glucose, ketones, bilirubin, hemoglobin, erythrocytes (RBCs), Nitrite (bacteria), and leukocytes (WBCs). A urinalysis study will be considered medically reasonable and necessary for the following conditions:
Does CLIAwaived test require modifier QW?
Exception: Because it is the simplest urine dipstick (manual, without microscopy), 81002 is one of the original CLIAwaived tests and does not require modifier QW. Example: The physician-office lab performs urinalysis for ketones, protein, hemoglobin, and glucose using the Bayer Clinitek Status Urine Chemistry Analyzer.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
This article contains coding that complements the Local Coverage Determination (LCD) for Urine Drug Testing.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
Article Guidance
The billing and coding information in this article is dependent on the coverage indications, limitations and/or medical necessity described in the related LCD L34645 Drug Testing.
ICD-10-CM Codes that Support Medical Necessity
For monitoring of patient compliance in a drug treatment program, use diagnosis code Z03.89 as the primary diagnosis and the specific drug dependence diagnosis as the secondary diagnosis.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act (SSA), §1862 (a) (1) (A), states that no Medicare payment shall be made for items or services which "are not reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member."
Article Guidance
The following coding and billing guidance is to be used with its associated Local coverage determination.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.
