To view the complete policy and the full list of codes, please refer to the CMS
Centers for Medicare and Medicaid Services
The Centers for Medicare & Medicaid Services, previously known as the Health Care Financing Administration, is a federal agency within the United States Department of Health and Human Services that administers the Medicare program and works in partnership with state government…
What is the CPT code for CBC without platelet count?
Based on comments, codes G0306 and G0307 have been established to permit continued billing of common bundled CBC testing services without a platelet count. If additional CBC component test (s) are medically necessary, only the medically necessary components (e.g. hemoglobin (Hgb) or hematocrit (Hct) ) should be ordered and performed.
What is the CPT value for CBC and manual differential?
Option No. 2 — The laboratory reports both CPTs 85027 ($8.89) and 85007 ($4.73) to capture the CBC (w/o differential) and manual differential.
What is the use of a modifier for CBC testing?
Billing modifiers can assist in reporting additional medically necessary CBC component test (s) or bundling testing service for the same patient on the same date of service, such as modifier -91 Repeat clinical laboratory test.
What is included in a complete blood count (CBC)?
Many treatments and therapies affect the blood or bone marrow, and blood counts may be used to monitor treatment effects. The complete blood count (CBC) includes a hemogram and differential white blood count (WBC).
What diagnosis covers CBC with diff?
Specific indications for CBC with differential count related to the WBC include signs, symptoms, test results, illness, or disease associated with leukemia, infections or inflammatory processes, suspected bone marrow failure or bone marrow infiltrate, suspected myeloproliferative, myelodysplastic or lymphoproliferative ...
Does Medicare pay for CBC test?
Original Medicare does cover blood tests when they are ordered by a doctor or other health care professional to test for, diagnose or monitor a disease or condition. The blood test must be deemed medically necessary in order to be covered by Medicare.
What is diagnosis code for CBC and CMP?
2022 ICD-10-CM Diagnosis Code Z13. 228: Encounter for screening for other metabolic disorders.
What ICD-10 code covers CBC for Medicare?
NCD 190.15 4. In some patients presenting with certain signs, symptoms or diseases, a single CBC may be appropriate.
How often does Medicare pay for CBC?
For people watching their cholesterol, routine screening blood tests are important. Medicare Part B generally covers a screening blood test for cholesterol once every five years. You pay nothing for the test if your doctor accepts Medicare assignment and takes Medicare's payment as payment in full.
Does Medicare Part B cover lab tests?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers medically necessary clinical diagnostic laboratory tests, when your doctor or provider orders them. You usually pay nothing for Medicare-covered clinical diagnostic laboratory tests.
What codes cover a CBC?
A complete blood count consists of measuring a blood specimen for levels of hemoglobin, hematocrit, red blood cells, white blood cells, and platelets.
What will cover a CBC?
The complete blood count (CBC) includes a hemogram and differential white blood count (WBC). The hemogram includes enumeration of red blood cells, white blood cells, and platelets, as well as the determination of hemoglobin, hematocrit, and indices.
What ICD-10 code covers routine labs?
From ICD-10: For encounters for routine laboratory/radiology testing in the absence of any signs, symptoms, or associated diagnosis, assign Z01. 89, Encounter for other specified special examinations.
Is CPT 82947 covered by Medicare?
Medicare only pays claims for Durable Medicare Equipment (DME) if the ordering provider and DME supplier are actively enrolled in Medicare on the date of service. Tell the Medicare beneficiary if you are not participating in Medicare before you order DME.
Does Medicare cover CPT code 80061?
Frequency Limitations: When monitoring long term anti-lipid dietary or pharmacologic therapy and when following patients with borderline high total or LDL cholesterol levels, it is reasonable to perform the lipid panel annually.
Is 85610 covered by Medicare?
A: When physicians use a prothrombin time test (reported with CPT code 85610) to monitor patients on anticoagulant drugs, Medicare pays the entity that performed the test. Its payment for the test is based on the geographically specific laboratory test fee schedule.
Description Information
Please Note: This may not be an exhaustive list of all applicable Medicare benefit categories for this item or service.
Coding Analyses for Labs (CALs)
This NCD has been or is currently being reviewed under the National Coverage Determination process. The following are existing associations with CALs, from the Coding Analyses for Labs database.
What is the CPT code for CBC?
A: One of the highest volume tests – the complete blood count (CBC) — may also be the source of most billing errors. Where does the confusion come from? Let’s take a closer look. The most common CPT codes reported in conjunction with CBC billing are as follows: 85025 — Blood count; complete (CBC), automated (Hgb, Hct, RBC, WBC and platelet count) and automated differential WBC count 85027– Blood count; complete (CBC), automated (Hgb, Hct, RBC, WBC and platelet count) 85007 — Blood count; blood smear, microscopic examination with manual differential WBC count
What is the CPT code for blood panel?
The first entry in the Pathology and Laboratory Section of the Current Procedural Terminology (CPT®′) codebook is labeled “Organ or Disease Oriented Panels.” Under the code for each blood panel is an inclusive list of each component code which when grouped together comprise the entire blood panel. CPT indicates that these panels were developed for coding purposes only. The blood panels are:#N#Code Description
What is NCCI code?
National Correct Coding Initiative (NCCI) edits have been established to promote correct coding and prevent inappropriate payments. For example, test codes 85027 and 85004 should not be billed along with code 85025 which represents the bundled testing service
What is a complete blood count?
A complete blood count consists of measuring a blood specimen for levels of hemoglobin, hematocrit, red blood cells, white blood cells, and platelets. Also, a differential white blood cell (WBC) count measures the percentages of different types of white blood cells.
Does Medicare cover CPT code 80050?
Do not report individually; claim will be denied for inappropriate coding. ** Medicare does not cover CPT code 80050. ** When codes 85025, 84443 and 80053 are done on the same encounter, you must report each code individually.
What percentage of Medicare beneficiaries are excluded from coverage?
For purpose of this exclusion, "the term 'usually' means more than 50 percent of the time for all Medicare beneficiaries who use the drug. Therefore, if a drug is self-administered by more than 50 percent of Medicare beneficiaries, the drug is excluded from coverage" and the MAC will make no payment for the drug.
Why are CPT codes not included in CPT codes?
They are used to identify various items and services that are not included in the CPT code set because they are medical items or services that are regularly billed by suppliers other than physicians. For example, ambulance services, hearing and vision services, drugs, and durable medical equipment.
What is MEDCAC in medical?
The MEDCAC reviews and evaluates medical literature, reviews technology assessments, public testimony and examines data and information on the benefits, harms, and appropriateness of medical items and services that are covered under Medicare or that may be eligible for coverage under Medicare.
What is a local coverage determination?
A Local Coverage Determination (LCD) is a decision made by a Medicare Administrative Contractor (MAC) on whether a particular service or item is reasonable and necessary, and therefore covered by Medicare within the specific jurisdiction that the MAC oversees. MACs are Medicare contractors that develop LCDs and process Medicare claims.
What is local coverage article?
Local coverage Articles are a type of educational document published by the Medicare Administrative Contractors (MACs). Articles often contain coding or other guidelines that complement a Local Coverage Determination (LCD). MACs are Medicare contractors that develop LCDs and Articles along with processing of Medicare claims.
What are some examples of Medicare coverage documents?
Examples include guidance documents, compendia, and solicitations of public comments. Close.
What is a LCD in Medicare?
LCDs are specific to an item or service (procedure) and they define the specific diagnosis (illness or injury) for which the item or service is covered. LCDs outline how the contractor will review claims to ensure that the services provided meet Medicare coverage requirements.
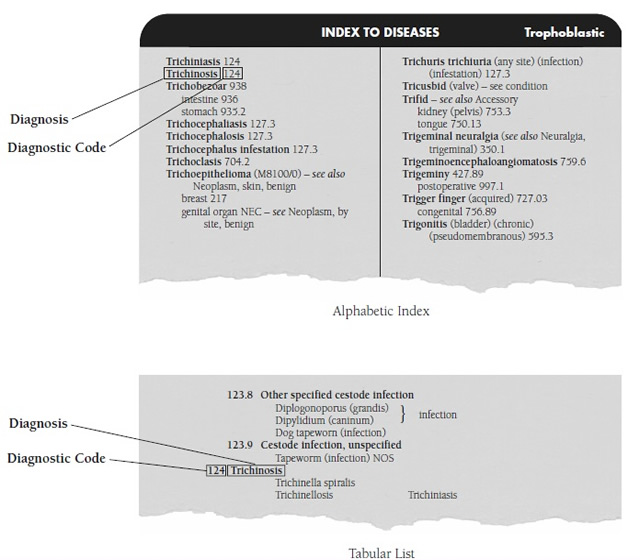
When did CMS release the ICD-10 conversion ratio?
On December 7, 2011, CMS released a final rule updating payers' medical loss ratio to account for ICD-10 conversion costs. Effective January 3, 2012, the rule allows payers to switch some ICD-10 transition costs from the category of administrative costs to clinical costs, which will help payers cover transition costs.
When did the ICD-10 come into effect?
On January 16, 2009, the U.S. Department of Health and Human Services (HHS) released the final rule mandating that everyone covered by the Health Insurance Portability and Accountability Act (HIPAA) implement ICD-10 for medical coding.
General Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
Title XVIII of the Social Security Act, §1833 (e) prohibits Medicare payment for any claim which lacks the necessary information to process the claim.
Article Guidance
The information in this article contains billing, coding or other guidelines that complement the Local Coverage Determination (LCD) for HbA1c L33431.
ICD-10-CM Codes that Support Medical Necessity
ICD-10 codes for performing tests at frequencies more than every 3 months. The following codes indicate or imply a condition of hyperglycemia and may be billed alone on the claim.
Bill Type Codes
Contractors may specify Bill Types to help providers identify those Bill Types typically used to report this service. Absence of a Bill Type does not guarantee that the article does not apply to that Bill Type.
Revenue Codes
Contractors may specify Revenue Codes to help providers identify those Revenue Codes typically used to report this service. In most instances Revenue Codes are purely advisory. Unless specified in the article, services reported under other Revenue Codes are equally subject to this coverage determination.