What is a Medicare-Medicaid plan?
Feb 11, 2022 · After the deductible is met, one must pay a cost share (coinsurance) for services. For Medicare Part B (medical insurance), enrollees must pay a monthly premium of $170.10. There is also an annual deductible of $233. To enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B.
What is the Centers for Medicare&Medicaid Services (CMS)?
If you have Medicare and full Medicaid coverage, most of your health care costs are likely covered. You can get your Medicare coverage through Original Medicare or a Medicare Advantage Plan (Part C). If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare. And, you'll automatically qualify for Extra Help paying for your …
What is Medicaid Medicaid?
Page 1 of 10 MEDICARE AND MEDICAID BASICS ICN 909330 July 2018 PRINT-FRIENDLY VERSION. Target Audience: Medicare and Medicaid Providers The Hyperlink Table, at the end of this document, provides the complete URL for each hyperlink. Medicare. Federal health care coverage for: People . aged 65 or older . Certain . people. under 65 with . disabilities
What is a special health plan for people with Medicare and Medicaid?
Medicaid. Medicaid is an assistance program. It serves low-income people of every age. Patients usually pay no part of costs for covered medical expenses. A small co-payment is sometimes required. Medicaid is a federal-state program. It varies from state to state. It is run by state and local governments within federal guidelines.
How do you get $144 back from Medicare?
You can get your reduction in 2 ways:If you pay your Part B premium through Social Security, the Part B Giveback will be credited monthly to your Social Security check.If you don't pay your Part B premium through Social Security, you'll pay a reduced monthly amount directly to Medicare.Sep 16, 2021
What income is Irmaa based on?
Who Pays IRMAA? As noted above, only individuals who earn more than $88,000 and married couples filing jointly who earn more than $176,000 are required to pay IRMAA.Nov 11, 2021
What are the Irmaa brackets for 2021?
C. IRMAA tables of Medicare Part B premium year for three previous yearsIRMAA Table2021More than $276,000 but less than or equal to $330,000$386.10More than $330,000 but less than $750,000$475.20More than $750,000$504.90Married filing separately12 more rows•Dec 6, 2021
At what income level does Medicare premium increase?
For example, when you apply for Medicare coverage for 2022, the IRS will provide Medicare with your income from your 2020 tax return. You may pay more depending on your income. In 2022, higher premium amounts start when individuals make more than $91,000 per year, and it goes up from there.Nov 16, 2021
Does Social Security income count towards Irmaa?
The tax-exempt Social Security isn't included in the MAGI calculation for the IRMAA.Dec 18, 2018
Is Irmaa based on adjusted gross income?
SSA determines if you owe an IRMAA based on the income you reported on your IRS tax return two years prior, meaning two years before the year that you start paying IRMAA. The income that counts is the adjusted gross income you reported plus other forms of tax-exempt income.
What will Irmaa be in 2023?
2023 IRMAA Brackets (Projected)PROJECTED 2023 IRMAA BRACKETS FOR MEDICARE PART BAbove $149,000 – $178,000Above $298,000 – $356,000Standard Premium x 2.6Above $178,000 – $500,000Above $356,000 – $750,000Standard Premium x 3.2Greater than $500,000Greater than $750,000Standard Premium x 3.45 more rows•Mar 28, 2022
How do I avoid Medicare Irmaa?
To avoid getting issued an IRMAA, you can proactively tell the SSA of any changes your income has seen in the past two years using a “Medicare Income-Related Monthly Adjustment Amount – Life-Changing Event” form or by scheduling an interview with your local Social Security office (1-800-772-1213).Dec 21, 2021
How do you calculate Magi for Irmaa?
MAGI is calculated as Adjusted Gross Income (line 11 of IRS Form 1040) plus tax-exempt interest income (line 2a of IRS Form 1040).Jan 25, 2022
What income is used to determine Medicare premiums 2021?
modified adjusted gross incomeMedicare premiums are based on your modified adjusted gross income, or MAGI. That's your total adjusted gross income plus tax-exempt interest, as gleaned from the most recent tax data Social Security has from the IRS.
What is deducted from your monthly Social Security check?
You can have 7, 10, 12 or 22 percent of your monthly benefit withheld for taxes. Only these percentages can be withheld. Flat dollar amounts are not accepted. Sign the form and return it to your local Social Security office by mail or in person.
What is Medicare Part A deductible for 2021?
Medicare Part A Premiums/Deductibles The Medicare Part A inpatient hospital deductible that beneficiaries will pay when admitted to the hospital will be $1,484 in 2021, an increase of $76 from $1,408 in 2020.Nov 6, 2020
What is medicaid?
Medicaid is a joint federal and state program that: 1 Helps with medical costs for some people with limited income and resources 2 Offers benefits not normally covered by Medicare, like nursing home care and personal care services
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
What is extra help?
And, you'll automatically qualify for. Extra Help. A Medicare program to help people with limited income and resources pay Medicare prescription drug program costs, like premiums, deductibles, and coinsurance. paying for your.
Does Medicare cover prescription drugs?
. Medicaid may still cover some drugs and other care that Medicare doesn’t cover.
Does medicaid pay first?
Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second. Medicaid never pays first for services covered by Medicare. It only pays after Medicare, employer group health plans, and/or Medicare Supplement (Medigap) Insurance have paid.
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Can you get medicaid if you have too much income?
Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid. The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid. In this case, you're eligible for Medicaid because you're considered "medically needy."
What is Medicare insurance?
Medicare. Medicare is an insurance program. Medical bills are paid from trust funds which those covered have paid into. It serves people over 65 primarily, whatever their income; and serves younger disabled people and dialysis patients. Patients pay part of costs through deductibles for hospital and other costs.
Is Medicare a federal program?
Small monthly premiums are required for non-hospital coverage. Medicare is a federal program. It is basically the same everywhere in the United States and is run by the Centers for Medicare & Medicaid Services, an agency of the federal government.
What does SLMB cover?
SLMB benefits cover the cost of the monthly Medicare Part B premium. The standard Part B premium in 2021 is $148.50 per month and is required of all Medicare Part B beneficiaries.
How do you qualify for SLMB?
Each state Medicaid program has its own rules concerning qualification.
What other Medicare Savings Programs are there?
SLMB is just one of the available Medicare Savings Programs. Others include:
How do you apply for SLMB?
Contact your state Medicaid program for information and assistance with applying for the SLMB program.
Is there Medicaid assistance for Medicare Advantage beneficiaries?
Individuals who qualify for both Medicare and Medicaid are considered “dual eligible” and may qualify for a certain type of Medicare Advantage plan called a Special Needs Plan. And one particular type of Special Needs Plan is a Dual Eligible Special Needs Plan (D-SNP).
What is dual eligible Medicare?
Beneficiaries with Medicare and Medicaid are known as dual eligibles – and account for about 20 percent of Medicare beneficiaries (12.1 million people). Dual eligibles are categorized based on whether they receive partial or full Medicaid benefits. Full-benefit dual eligibles have comprehensive Medicaid coverage, ...
What is a dual eligible special needs plan?
If you are dual eligible, you are can enroll in a dual eligible special needs plan (D-SNP) that covers both Medicare and Medicaid benefits. These plans may also pay for expenses that Medicare and Medicaid don’t over individually, including over-the-counter items, hearing aids, and vision or dental care. Beneficiaries who are dual eligible can ...
Who is Josh Schultz?
Josh Schultz has a strong background in Medicare and the Affordable Care Act. He coordinated a Medicare ombudsman contract at the Medicare Rights Center in New York City, and represented clients in extensive Medicare claims and appeals.
Does Medicare cover long term care?
But this is not the case for things Medicare doesn’t cover, like long-term care . If Medicaid is covering a beneficiary’s long-term care, Medicare will still be the primary payer for any Medicare-covered services – like skilled nursing care or physical therapy.
Do seniors qualify for medicaid?
Many seniors who live in nursing homes are dual eligible: they qualify for Medicare based on their age, and Medicaid because of their financial circumstances.
Is Medicare the same as Medicaid?
The federal government oversees Medicare eligi bility – meaning it is the same in each state. But states set their own eligibility rules for Medicaid and the MSPs (within federal guidelines) – and income limits for these programs vary widely.
How many people are covered by Medicare?
Published: Aug 20, 2019. Medicare, the federal health insurance program for more than 60 million people ages 65 and over and younger people with long-term disabilities, helps to pay for hospital and physician visits, prescription drugs, and other acute and post-acute care services. This issue brief includes the most recent historical ...
How much is Medicare spending?
Medicare spending was 15 percent of total federal spending in 2018, and is projected to rise to 18 percent by 2029. Based on the latest projections in the 2019 Medicare Trustees report, the Medicare Hospital Insurance (Part A) trust fund is projected to be depleted in 2026, the same as the 2018 projection. In 2018, Medicare benefit payments totaled ...
Why is Medicare spending so high?
Over the longer term (that is, beyond the next 10 years), both CBO and OACT expect Medicare spending to rise more rapidly than GDP due to a number of factors, including the aging of the population and faster growth in health care costs than growth in the economy on a per capita basis.
When will Medicare be depleted?
In the 2019 Medicare Trustees report, the actuaries projected that the Part A trust fund will be depleted in 2026, the same year as their 2018 projection and three years earlier than their 2017 projection (Figure 8).
Will Medicare spending increase in the future?
While Medicare spending is expected to continue to grow more slowly in the future compared to long-term historical trends, Medicare’s actuaries project that future spending growth will increase at a faster rate than in recent years, in part due to growing enrollment in Medicare related to the aging of the population, increased use of services and intensity of care, and rising health care prices.
Does Medicare Advantage cover Part A?
Medicare Advantage plans, such as HMOs and PPOs, cover Part A, Part B, and (typically) Part D benefits. Beneficiaries enrolled in Medicare Advantage plans pay the Part B premium, and may pay an additional premium if required by their plan; about half of Medicare Advantage enrollees pay no additional premium.
Is Medicare spending comparable to private health insurance?
Prior to 2010, per enrollee spending growth rates were comparable for Medicare and private health insurance. With the recent slowdown in the growth of Medicare spending and the recent expansion of private health insurance through the ACA, however, the difference in growth rates between Medicare and private health insurance spending per enrollee has widened.
What is the federal reimbursement rate for Medicaid?
This Federal Medical Assistance Percentage (FMAP) changes each year and depends on the state’s average per capita income level. The reimbursement rate begins at 50% and reaches 77% in 2020.
How many people are covered by Medicare?
Department of Health and Human Services (HHS), oversee both. Data on Medicaid show that it serves about 64.5 million people, as of November 2019. Medicare funded the healthcare costs ...
What is the difference between Medicare and Medicaid?
Medicare and Medicaid are two government programs that provide medical and other health-related services to specific individuals in the United States. Medicaid is a social welfare or social protection program , while Medicare is a social insurance program. President Lyndon B. Johnson created both Medicare and Medicaid when he signed amendments ...
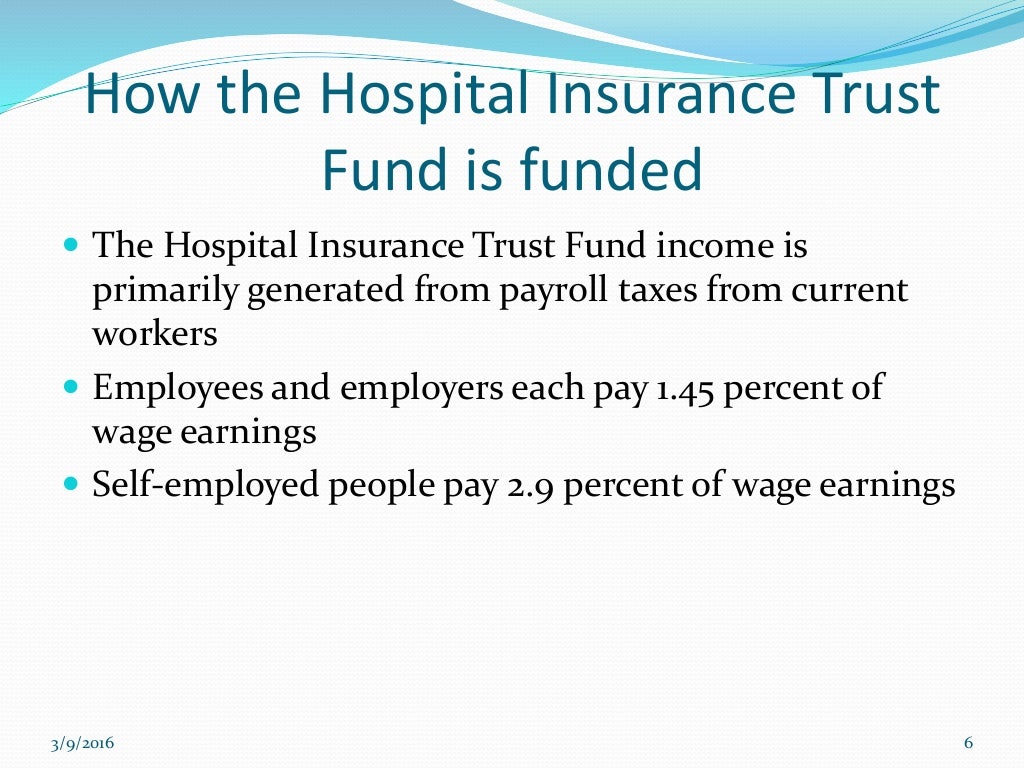
Where does Medicare money come from?
Most of the funding for Medicare comes from: payroll taxes under the Federal Insurance Contributions Act (FICA) the Self-Employment Contributions Act (SECA) Typically, the employee pays half of this tax, and the employer pays the other half.
What is Medicare Part C?
Medicare Part C. Medicare Part C, also known as Medicare Advantage Plans or Medicare+ Choice, allows users to design a custom plan that suits their medical situation more closely. Part C plans provide everything in Part A and Part B, but may also offer additional services, such as dental, vision, or hearing treatment.
What is a FQHC?
Users must check their coverage before receiving health care. People who do not have private health insurance can seek help at a federally qualified health center (FQHC). These centers provide coverage on a sliding scale, depending on the person’s income. FQHC provisions include: prenatal care. vaccines for children.
What is EPSDT in Medicaid?
early and periodic screening, diagnostic, and treatment (EPSDT) for under 21s. States may also choose to provide additional services and still receive federal matching funds. The most common of the 34 approved optional Medicaid services are: diagnostic services. prescribed drugs and prosthetic devices.
