In general, Medicare Part B will cover the most common diabetic supplies, when medically necessary and prescribed by a doctor, including Blood sugar (blood glucose) monitoring and self-testing equipment insulin pumps
Full Answer
Does Medicare cover diabetes?
When it comes to diabetic supplies covered by Medicare, it’s important to keep in mind that Original Medicare covers most basic diabetes supplies —including annual diabetes wellness checks, testing supplies, and insulin pumps. You may still have to pay a copay, though, and you may not get full coverage for all of the supplies you need or want.
Are diabetic supplies covered by Medicare?
Medicare does cover diabetes supplies such as insulin and lancets. Medicare Advantage plans also cover the same diabetes supplies and services as Original Medicare. Medicare beneficiaries who are diabetic have a number of Medicare coverage options they can consider for the diabetes care they need.
What does Medicare cover for diabetics?
- Blood sugar (glucose) testing monitors
- Blood sugar (glucose) test strips
- Finger-prick devices and lancets
- Glucose control solution for calibrating monitors
- Therapeutic shoes or inserts
Will Medicare cover A1c?
Hi David! Yes, Medicare will cover an A1c test once every three months under Part B.

What part of Medicare are diabetic supplies covered under?
Part DGenerally, Part B covers the services that may affect people who have diabetes. Part B also covers some preventive services for people who are at risk for diabetes. You must have Part B to get services and supplies it covers. Part D covers diabetes supplies used to inject or inhale insulin.
Is Livongo covered by Medicare?
Mountain View, CA – April 30, 2019 – Livongo, the leading Applied Health Signals company empowering people with chronic conditions to live better and healthier lives, today announced that it has been approved by the Centers for Medicare and Medicaid Services (CMS) as an enrolled provider for Medicare Advantage members.
Do diabetics qualify for Medicare?
Some preventive care is covered by Part B, including diagnostic screenings for diabetes and cardiovascular disease, obesity screening and counseling, and glaucoma tests. Starting April 1, 2018, Medicare will cover diabetes prevention program services for certain individuals at risk for diabetes.
Does Medicare pay for diabetes screening?
Medicare Part B covers an annual diabetes screening, including a fasting blood glucose test and/or a post-glucose challenge test, if you have one of the following risk factors: High blood pressure (hypertension) History of high blood sugar. History of abnormal cholesterol levels (dyslipidemia)
What brand of glucose meter is covered by Medicare 2021?
A2: Starting January 1, 2021, covered meters include: OneTouch Verio Reflect ®, OneTouch Verio Flex®, OneTouch Verio® and OneTouch Ultra 2®. All OneTouch test strips will have preferred formulary status.
Is Accu Chek covered by Medicare?
Accu-Chek is ALWAYS COVERED on Medicare Part B Your patient pays only $1.66 for 50 test strips and may pay a $0 co-pay.
What diagnosis will cover a hemoglobin A1c?
“HbA1c may be used for the diagnosis of diabetes, with values >6.5% being diagnostic.
Is metformin covered by Medicare?
Yes. 100% of Medicare prescription drug plans cover this drug.
Is A1c test covered by Medicare?
Hemoglobin A1c Tests: Your doctor might order a hemoglobin A1c lab test. This test measures how well your blood glucose has been controlled over the past 3 months. Medicare may cover this test for anyone with diabetes if it is ordered by his or her doctor.
Does Medicare pay for Libre FreeStyle?
Medicare covers CGMs like the FreeStyle Libre under the durable medical equipment (DME) portion of Medicare Part B, provided you meet eligibility criteria. If you qualify for coverage for the monitor, Medicare will also cover your supplies within certain limits.
Does Medicare cover A1c for pre diabetes?
(Note that the Hemoglobin A1c is not currently covered by Medicare for pre-diabetes screening).
Does Medicare cover test strips for type 2 diabetes?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers some diabetic test supplies, including blood sugar test strips, as durable medical equipment (DME).
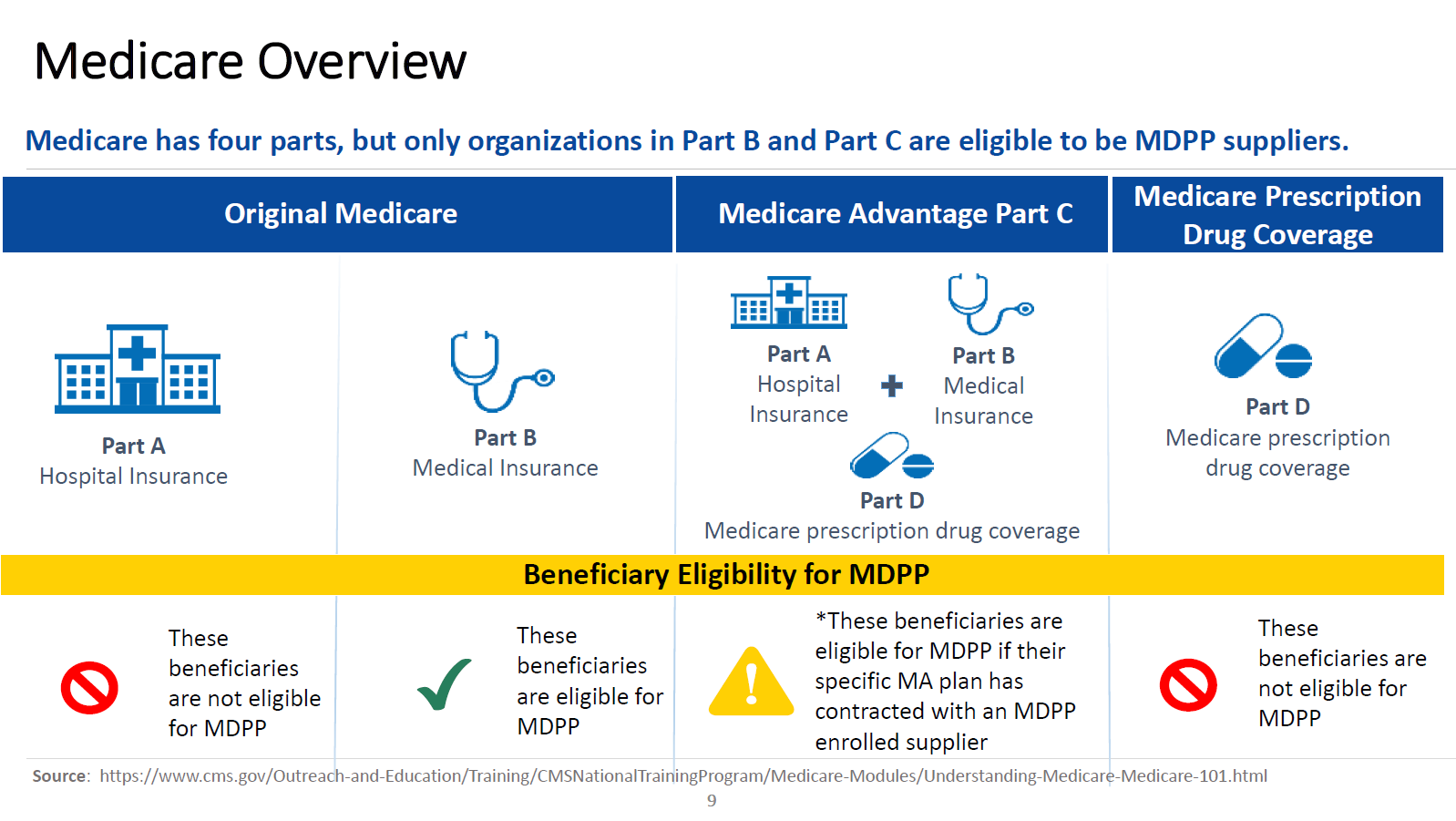
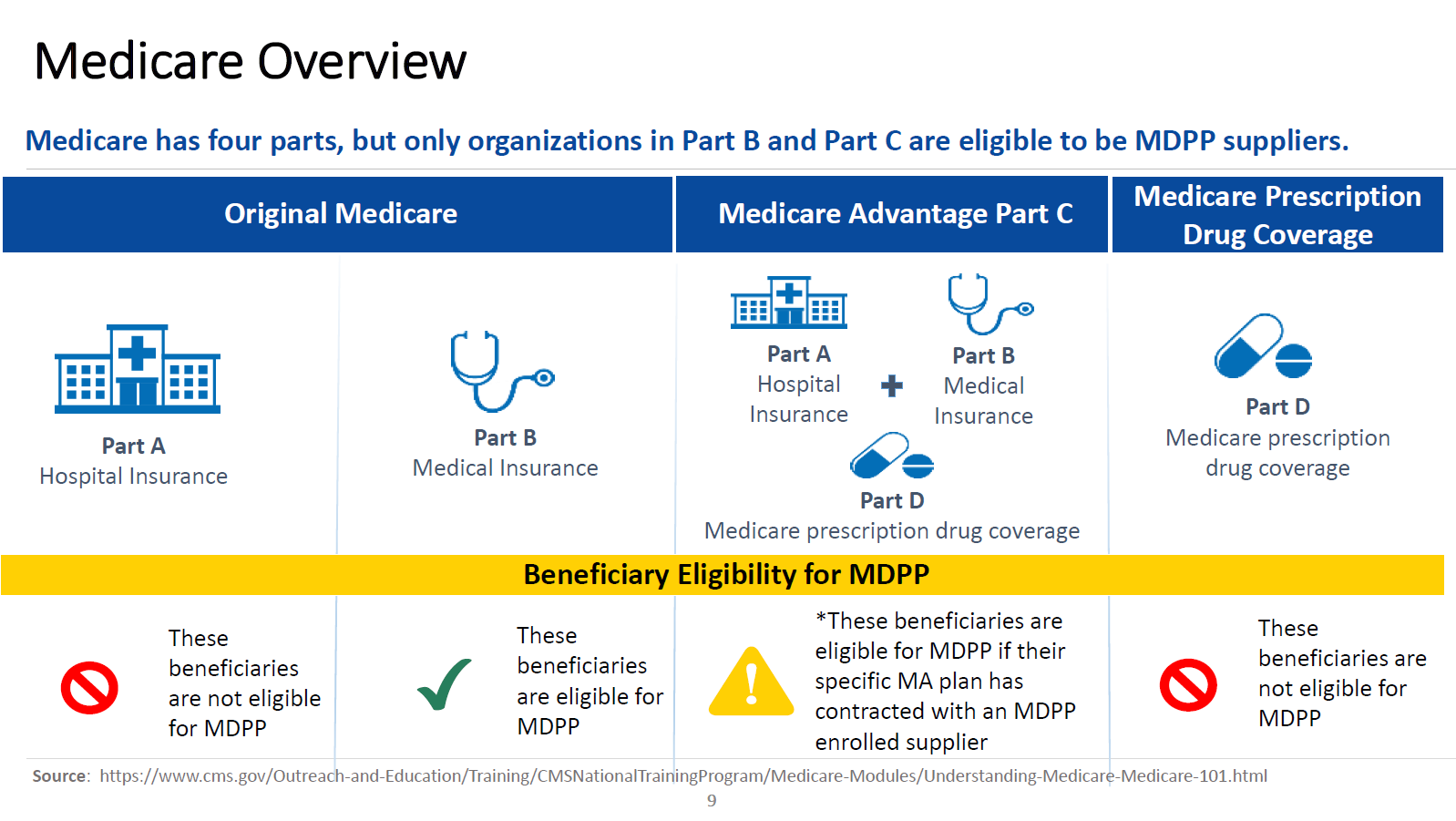
Medicare Part A
Medicare Part A (hospital insurance) provides coverage for medically necessary inpatient hospital stays, skilled nursing facilities, hospice care and some home health care.
Medicare Part B
Medicare Part B (medical insurance) provides coverage for medically necessary doctors' services, outpatient care, durable medical equipment, lab tests, preventive care and some medically necessary services not covered by Part A (including some physical and occupational therapy services and some home health care).
Medicare national mail-order program for diabetes testing supplies
On July 1, 2013, a Medicare National Mail-Order Program for diabetes testing supplies went into effect.
Medicare advantage (medicare Part C)
Some beneficiaries choose Medicare Advantage plans instead of Medicare Part A and B (the "Original Medicare Plan"). A Medicare Advantage Plan is a type of Medicare health plan offered by a private insurance company that contracts with Medicare to provide you with all your Part A and Part B benefits.
Medicare Part D
Medicare Part D is the prescription drug program available to all Medicare beneficiaries. Under Part D, beneficiaries choose a Prescription Drug Plan run by a private insurance company approved by Medicare.
How to learn more
For more information on all of the options available under Medicare, visit: www.medicare.gov or call 1-800-MEDICARE (800-633-4227). Also look for the Medicare and You handbook which Medicare mails to beneficiaries in the fall and is available by calling 1-800-MEDICARE (800-633-4227).
What is the Medicare Part B copayment?
For Medicare Part B, this comes to 20%. Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
What is the number to call for insulin pump?
For questions about Part B’s coverage of insulin and insulin pumps, a person can call 1-800-MEDICARE.
What are the factors that affect Medicare Part B screening?
high blood pressure. history of high blood sugar. history of abnormal cholesterol levels. obesity. Medicare Part B also covers an annual diabetes screening if at least two of the following factors apply: a person is 65 years of age or older. a person has overweight. a person’s family has a history of diabetes.
Does Medicare pay for glucose monitors?
In 2020, a person with Medicare Part B will pay 20% of the cost for diabetes self-management suppli es such as glucose monitors, lancets, and test strips. However, to ensure Medicare coverage, a person must get the prescription from their doctor, and use an in-network pharmacy or supplier.
Does Medicare cover diabetic supplies?
Share on Pinterest. Medicare may cover some diabetic supplies, including some preventive services. Medicare Part D, which is prescription drug coverage, may cover a person for some diabet ic supplies used for inhaling or injecting insulin.
Does Medicare pay for diabetic eye exams?
Costs of diabetic eye exams. If a person has original Medicare, they may pay 20% of the Medicare-approved amount for the eye doctor’s services. A Part B deductible may also apply. If the eye exam takes place in a hospital outpatient setting, a person may have to pay a copay.
Does Medicare cover foot exams?
If a person has diabetes-related nerve damage, Medicare Part B may cover a foot exam twice a year. A person is eligible for coverage if they have not seen a foot care doctor for other medical reasons between the foot exam visits.
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS) has developed a variety of educational resources for use by health care professionals and their staff as part of a broad outreach campaign to promote awareness and increase utilization of preventive services covered by Medicare. For more information about coverage, coding, billing, and reimbursement of Medicare-covered preventive services and screenings, visit
Does Medicare cover therapeutic shoes?
If a beneficiary has Medicare Part B, has diabetes, and meets certain conditions (see below), Medicare will cover therapeutic shoes if they need them. The types of shoes that are covered each year include one of the following:
Does Medicare pay for insulin pumps?
In the Original Medicare Plan, the beneficiary pays 20 percent of the Medicare-approved amount after the yearly Part B deductible. Medicare will pay 80 percent of the cost of the insulin pump. Medicare will also pay for the insulin that is used with the insulin pump.
How many prescription drugs are covered by Medicare?
Plans include both brand-name prescription drugs and generic drug coverage. The formulary includes at least 2 drugs in the most commonly prescribed categories and classes. This helps make sure that people with different medical conditions can get the prescription drugs they need. All Medicare drug plans generally must cover at least 2 drugs per ...
How many drugs does Medicare cover?
All Medicare drug plans generally must cover at least 2 drugs per drug category, but plans can choose which drugs covered by Part D they will offer. The formulary might not include your specific drug. However, in most cases, a similar drug should be available.
What is formulary exception?
A formulary exception is a drug plan's decision to cover a drug that's not on its drug list or to waive a coverage rule. A tiering exception is a drug plan's decision to charge a lower amount for a drug that's on its non-preferred drug tier.
What happens if you don't use a drug on Medicare?
If you use a drug that isn’t on your plan’s drug list, you’ll have to pay full price instead of a copayment or coinsurance, unless you qualify for a formulary exception. All Medicare drug plans have negotiated to get lower prices for the drugs on their drug lists, so using those drugs will generally save you money.
What does Medicare Part D cover?
All plans must cover a wide range of prescription drugs that people with Medicare take, including most drugs in certain protected classes,” like drugs to treat cancer or HIV/AIDS. A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary.
What is a tier in prescription drug coverage?
Tiers. To lower costs, many plans offering prescription drug coverage place drugs into different “. tiers. Groups of drugs that have a different cost for each group. Generally, a drug in a lower tier will cost you less than a drug in a higher tier. ” on their formularies. Each plan can divide its tiers in different ways.
What is a drug plan's list of covered drugs called?
A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary. Many plans place drugs into different levels, called “tiers,” on their formularies. Drugs in each tier have a different cost. For example, a drug in a lower tier will generally cost you less than a drug in a higher tier.