Medicare Part B (Medical Insurance) covers some diabetic test supplies, including blood sugar test strips, as durable medical equipment (DME). If your supplier accepts Assignment you pay 20% of the Medicare-approved amount, and the Part B Deductible applies. Medicare pays for different kinds of DME in different ways.
Full Answer
Does Medicare pay for diabetic testing supplies?
Medicare Part B covers the same type of blood glucose testing supplies for people with diabetes whether or not they use insulin. However, the amount of supplies that are covered varies. If the beneficiary • Uses insulin, they may be able to get up to 100 test strips and lancets every month, and 1 lancet device every 6 months.
What supplies do I need to test for diabetes?
- Insulin and insulin loaded dispensing products (vials or box of individual vials, jet injectors, biojectors, epipens, infusers and preloaded syringes)
- Unlimited number of unused syringes when accompanied by insulin or other injectable medication
- Lancets, blood glucose meters, blood glucose meter test strips, alcohol swabs, meter-testing solutions
Where to get some diabetic testing supplies?
- Discounts and free shipping: ADW carries a full stock of popular, brand name diabetes products. ...
- Free meters: ADW offers numerous glucose meter deals. ...
- Autoship Program: If you need regular deliveries, you can enroll in ADW’s Autoship program. ...
- Pet diabetic supplies: ADW also sells diabetic pet supplies. ...
How do I get my diabetic supplies through Medicare?
- A National Effort to Prevent Type 2 Diabetes: Participant-Level Evaluation of CDC’s National Diabetes Prevention Program
- Free Diabetes Supplies Available Tomorrow in Houston and Corpus Christi, Plus Extended Hours at 1-800-DIABETES Call Center Through Next Week
- Work to Do Before Medicare's Diabetes Prevention Program Is Set in Place

Are diabetic test strips and lancets covered by Medicare?
Medicare Part B covers the same type of blood glucose testing supplies for people with diabetes whether or not they use insulin. However, the amount of supplies that are covered varies. Uses insulin, they may be able to get up to 100 test strips and lancets every month, and 1 lancet device every 6 months.
What brand of glucometer does Medicare cover?
Accu-Chek ® is ALWAYS COVERED on Medicare Part B. 1 Give your patient a better testing experience.
Are Accu-Chek strips covered by Medicare?
Accu-Chek is ALWAYS COVERED on Medicare Part B Your patient pays only $1.66 for 50 test strips and may pay a $0 co-pay.
Does Medicare cover test strips for type 2 diabetes?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers some diabetic test supplies, including blood sugar test strips, as durable medical equipment (DME).
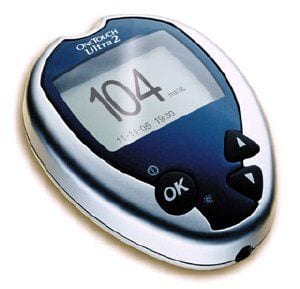
What brand of glucose meter is covered by Medicare 2021?
A2: Starting January 1, 2021, covered meters include: OneTouch Verio Reflect ®, OneTouch Verio Flex®, OneTouch Verio® and OneTouch Ultra 2®. All OneTouch test strips will have preferred formulary status.
How do I get free diabetic supplies?
People who don't have insurance coverage for prescriptions may find their medicines and supplies for free or at low cost through PPARX.org. RxAssist.org lists drug-company assistance programs, state programs, discount drug cards, copay help, and more.
How many diabetic test strips will Medicare pay for?
If you don't use insulin, you may be able to get 100 test strips and 100 lancets every 3 months. If your doctor says it's medically necessary, and if other qualifications and documentation requirements are met, Medicare will allow you to get additional test strips and lancets.
How do I get free diabetic supplies from Medicare?
You must have Part B to get services and supplies it covers. Part D covers diabetes supplies used to inject or inhale insulin. You must be enrolled in a Medicare drug plan to get supplies Part D covers.
Does Medicare cover A1c test?
Hemoglobin A1c Tests: Your doctor might order a hemoglobin A1c lab test. This test measures how well your blood glucose has been controlled over the past 3 months. Medicare may cover this test for anyone with diabetes if it is ordered by his or her doctor.
How can I get free glucose test strips?
Glucose meters One of the easiest ways to get a free blood glucose meter is to contact the manufacturer directly. The majority of manufacturers offer free glucose monitors as a way to entice patients to purchase other brand-name supplies, such as glucose test strips, through the manufacturer.
How much are diabetes test strips?
Walmart's brand ReliOn also has a meter and 50 test strips available for $15, with additional test strips available for $9 per 50 strips. Subscription Services: For each of the subscription services, no health insurance or doctor's prescription is needed.
What supplies do you need to treat diabetes?
You may need the following supplies to help manage the disease: Glucose (blood sugar) testing monitors and test strips. Insulin.
What are the best ways to treat diabetes?
If you are diagnosed with diabetes, you and your physician will create a treatment plan designed to meet your specific needs. You may need the following supplies to help manage the disease: 1 Glucose (blood sugar) testing monitors and test strips 2 Insulin 3 Lancet devices and lancets 4 Blood sugar control solutions (to check the accuracy of the test strips and monitor) 5 Therapeutic shoes or inserts
What is Medicare Part D?
What Medicare Part D Can Do. Medicare Part D provides prescription drug coverage and may help you pay for some diabetes supplies. If you have Original Medicare, you may enroll in a stand-alone Prescription Drug Plan (PDP). Many Medicare recipients choose to get their benefits through a Medicare Advantage ...
What is covered by Part B?
Many of the diabetes supplies you will need are covered by Part B’s DME benefits, including: Glucose testing monitors. Blood sugar test strips. Lancets and lancet devices. Glucose control solutions.
Can you get Medicare for diabetes?
Treatment for diabetes can vary depending on the needs of each individual patient, but many people living with diabetes rely on medical supplies to test blood sugar levels, recognize symptoms, and treat the disease. If you are eligible for Medicare, you may get help paying for the diabetes supplies that can help you manage diabetes.
Does Medicare cover shoes?
One pair of extra-depth shoes. Medicare will also cover 2 additional pairs of inserts each calendar year for custom-molded shoes and 3 pairs of inserts each calendar year for extra-depth shoes. Medicare will cover shoe modifications instead of inserts. In order for Medicare to help cover these supplies, you will likely need to rent ...
Can Medicare pay for blood sugar control?
Blood sugar control solutions (to check the accuracy of the test strips and monitor) If you are eligible for Medicare, you may get help paying for some of your diabetes supplies. When you qualify for Medicare due to age or disability, you will likely be automatically enrolled in Part A (Hospital Insurance).
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B.
What percentage of Medicare payment does a supplier pay for assignment?
If your supplier accepts Assignment you pay 20% of the Medicare-approved amount, and the Part B Deductible applies. Medicare pays for different kinds of DME in different ways. Depending on the type of equipment:
Does Medicare cover DME equipment?
You may be able to choose whether to rent or buy the equipment. Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare.
Do suppliers have to accept assignment for Medicare?
It’s important to ask your suppliers if they participate in Medicare before you get DME. If suppliers are participating suppliers, they must accept assignment (which means, they can charge you only the coinsurance and Part B deductible for the Medicare‑approved amount).
How often do you need to take insulin test strips?
number of test strips and lancets you need (Part B typically pays for 100 strips and lancets every 3 months if you don’t use insulin) New prescriptions are needed each year from your doctor. If you need to monitor your blood sugar more often, your supply limits for each month will need to be increased.
What is DME in diabetics?
Some diabetic equipment, nutritional therapy, and shoe inserts/special footwear are available through durable medical equipment (DME) providers. You’ll need prescriptions from your doctor for all supplies and equipment.
What is Medicare Part D?
Medicare Part D plans are private plans that cover medications that treat diabetes, including insulin and supplies to inject insulin. You must be enrolled in original Medicare (parts A and B) to be eligible for Part D.
How much does Medicare Part B coinsurance cost?
Under Medicare Part B, you’ll pay coinsurance costs (typically 20 percent ). As long as the pharmacy you use accepts assignment, the costs will be lower than with a nonparticipating provider.
What are the parts of Medicare?
Medicare parts B, C, and D each covers different supplies, medications, and services needed to manage diabetes. Make sure you go to pharmacies or equipment providers that are enrolled in Medicare and accept the assignment prices set by Medicare.
How many people have diabetes?
Of the 30 million. Americans with diabetes, 90 percent have type 2. Twenty–four million people 65 and older have prediabetes (higher than normal blood sugar concentrations). Risk factors for diabetes can be different for each type, but family history, age, race, and environmental factors may all impact the condition.
Does Medicare cover diabetes?
Get prescriptions from your doctor for any medication, supply, or service you’ll want Medicare to cover. Check that your pharmacy or device supplier accepts Medicare set payment rates to avoid overpaying. Diabetes is a metabolic condition that leads to high blood sugar levels.
What is the number to call for insulin pump?
For questions about Part B’s coverage of insulin and insulin pumps, a person can call 1-800-MEDICARE.
What are the factors that affect Medicare Part B screening?
high blood pressure. history of high blood sugar. history of abnormal cholesterol levels. obesity. Medicare Part B also covers an annual diabetes screening if at least two of the following factors apply: a person is 65 years of age or older. a person has overweight. a person’s family has a history of diabetes.
What is the Medicare Part B copayment?
For Medicare Part B, this comes to 20%. Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
Does Medicare pay for glucose monitors?
In 2020, a person with Medicare Part B will pay 20% of the cost for diabetes self-management suppli es such as glucose monitors, lancets, and test strips. However, to ensure Medicare coverage, a person must get the prescription from their doctor, and use an in-network pharmacy or supplier.
Does Medicare cover diabetic supplies?
Share on Pinterest. Medicare may cover some diabetic supplies, including some preventive services. Medicare Part D, which is prescription drug coverage, may cover a person for some diabet ic supplies used for inhaling or injecting insulin.
Does Medicare pay for diabetic eye exams?
Costs of diabetic eye exams. If a person has original Medicare, they may pay 20% of the Medicare-approved amount for the eye doctor’s services. A Part B deductible may also apply. If the eye exam takes place in a hospital outpatient setting, a person may have to pay a copay.
Does Medicare cover foot exams?
If a person has diabetes-related nerve damage, Medicare Part B may cover a foot exam twice a year. A person is eligible for coverage if they have not seen a foot care doctor for other medical reasons between the foot exam visits.
How Much Do Diabetic Supplies Cost With Medicare
You must get your diabetic supplies from a participating pharmacy or supplier thats enrolled in Medicare. Otherwise, Medicare wont pay and youll be responsible for the bill.
What Diabetes Supplies Does Medicare Cover
The diabetes equipment and supplies that are covered by Medicare Part B include the following:
Medicare And Diabetes Coverage
Medicare and diabetes coverage is a concern for many Americans. Diabetes can cause a persons health and well-being to deteriorate over time. Close monitoring is often necessary because diabetes causes other health concerns and conditions. Below we go into full detail about what you need to know regarding Medicare and diabetes coverage.
Medicare Coverage Of Diabetic Services And Supplies
Medicare covers many diabetic services, if they are delivered by a doctor or other provider who accepts Medicare assignment. Medicare also covers a range of common diabetic supplies when theyre considered medically necessary.
Is There Medicare Coverage For Insulin Pumps And Insulin
If you meet certain medical conditions and your doctor believes an external insulin pump is medically necessary to treat your diabetes, Medicare may cover 80% of the allowable charges for the pump. You generally pay 20% plus any applicable deductible.
Medicare Beneficiaries With Diabetes May Have Other Coverage Options For Insulin And More
You can compare Part D plans available where you live and enroll in a Medicare prescription drug plan online when you visit MyRxPlans.com.
How Does Medicare Part D Cover Diabetes
Medicare Part D is prescription drug coverage. If you joined a Medicare drug plan, youre covered for the following: 5
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS) has developed a variety of educational resources for use by health care professionals and their staff as part of a broad outreach campaign to promote awareness and increase utilization of preventive services covered by Medicare. For more information about coverage, coding, billing, and reimbursement of Medicare-covered preventive services and screenings, visit
Does Medicare cover therapeutic shoes?
If a beneficiary has Medicare Part B, has diabetes, and meets certain conditions (see below), Medicare will cover therapeutic shoes if they need them. The types of shoes that are covered each year include one of the following:
Does Medicare pay for insulin pumps?
In the Original Medicare Plan, the beneficiary pays 20 percent of the Medicare-approved amount after the yearly Part B deductible. Medicare will pay 80 percent of the cost of the insulin pump. Medicare will also pay for the insulin that is used with the insulin pump.
Medicare diabetic coverage at a glance
Generally, Part B covers the services that may affect people with diabetes. Part B also covers certain preventive services for people at risk for diabetes. You must have Part B to get the services and supplies it covers. 1
Sharing the cost of diabetic supplies and services
To see what Medicare covers and what you pay, review the following chart:
Learn more about Medicare
For more helpful information on Medicare, check out these 10 frequently asked questions about Medicare plans.