Other Disabilities and Medicare
- Dementia. Medicare covers the cost of some services for adults with dementia. Covered services can include physical...
- Mental illness. When it comes to mental illness — if you are disabled, you may qualify for SSDI and Medicare coverage.
- Long-term and chronic conditions. Adults with long-term or chronic conditions are also eligible for...
What are the top 10 conditions that qualify for disability?
Jul 16, 2020 · Even though most people on Social Security Disability Insurance must wait for Medicare coverage to begin, two conditions might ensure immediate eligibility: end-stage renal disease (ESRD) and Lou Gehrig’s disease (ALS). End-stage renal disease (ESRD) ESRD, also known as permanent kidney failure, is a disease in which the kidneys no longer work.
What do I need to know about Medicare Disability Eligibility?
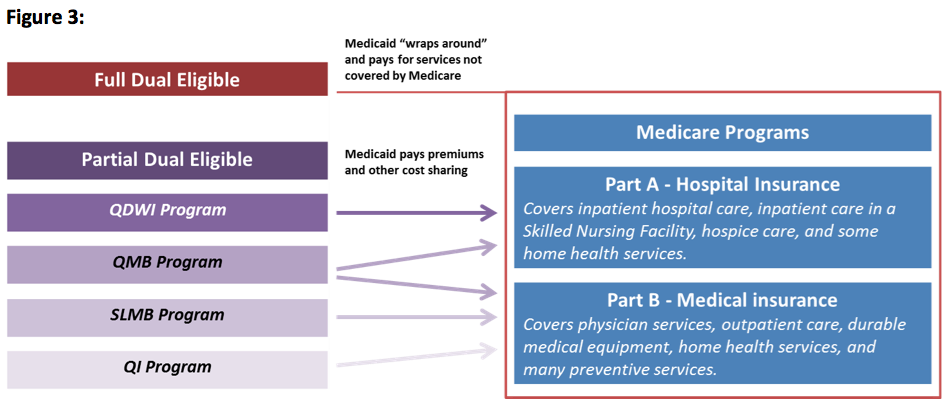
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance). You are eligible for premium-free Part A if you are age 65 or older and you or your spouse worked and …
What are the criteria to meet eligibility for Medicare?
Mar 15, 2022 · Here are some of the most common: Cerebral palsy Down Syndrome Muscular Dystrophy Blindness or visual impairment Hearing impairment Kidney disease Liver disease Mental illness Paralysis Severe arthritis
Can you get Medicare early if you are disabled?
Medicare is available for certain people with disabilities who are under age 65. These individuals must have received Social Security Disability benefits for 24 months or have End Stage Renal Disease (ESRD) or Amyotropic Lateral Sclerosis (ALS, also known as Lou Gehrig’s disease).
How long does it take to get Medicare?
This process alone can take several months to complete. It may take three to six months for the Social Security Administration to approve your application.
How long does a disability last?
For the purposes of Social Security Disability Insurance, impairments must last at least more than 12 months in duration. 1 . Definitions of disability can vary from person to person but Medicare guidelines leave no room for interpretation. Someone must be incapacitated for the long term.
Who is Elaine Hinzey?
Elaine Hinzey is a fact checker, writer, researcher, and registered dietitian. Learn about our editorial process. Elaine Hinzey, RD. Updated on October 22, 2020. Not everyone who is eligible for Medicare is 65 years and older.
How many people have ALS?
It is estimated that as many as 16,000 Americans have ALS at any one time. 2 The severity and rapid progression of the disease requires a higher level of medical care and services. You are immediately eligible for Medicare and should apply as soon as possible. There is no waiting period. 3 .
How long does Medicare cover kidney transplant?
If you get a kidney transplant, Medicare coverage may not be long term. The program will provide coverage for 36 months after a Medicare-approved transplant.
How many people have end stage renal disease?
You have end-stage renal disease (ESRD): About 15 percent of Americans are estimated to have chronic kidney disease, according to the Centers for Disease Control and Prevention. 4 More than 100,000 people go on to develop kidney failure, also referred to as end-stage renal disease, each year.
How long does it take for Social Security to approve a claim?
It may take three to six months for the Social Security Administration to approve your application. The application process could be expedited if your medical condition is on the list of Compassionate Allowances Conditions. 5 .
Compare Plans in your Area
We help Medicare beneficiaries maximize their benefits.#N#(and Discover the Best Rates, for FREE)
ESRD Medicare Coverage
ESRD Medicare coverage can provide coverage for permanent kidney failure that requires dialysis or a kidney transplant. To be eligible, you must be diagnosed with end-stage renal disease (ESRD) and qualify for SSDI (Social Security Disability Insurance) or Social Security retirement benefits/railroad retirement benefits based on your work history.
ALS Medicare Coverage
If you have been diagnosed with ALS, also known as Lou Gehrig’s Disease, you will be automatically enrolled in Original Medicare (Part A and B) the first month you receive Social Security Disability Insurance (SSDI) or a railroad disability annuity check.
Other Qualifying Disabilities
You are automatically enrolled in Original Medicare (Part A and B) after you have received Social Security disability benefits for 24 months or have certain disability benefits from the RRB for 24 months. If you qualify, you will get your red, white, and blue Medicare card in the mail 3 months before your 25th month of disability.
How to Enroll in Coverage Beyond Original Medicare
Health costs can quickly add up. It’s great that Original Medicare is available with qualifying disabilities to people under 65, but what about coverage beyond Original Medicare? Medicare Advantage, Medicare Supplements, and Part D plans can add additional benefits and help you save on out-of-pocket costs.
What are the conditions covered by Medicare?
People with these and other long-term conditions are entitled to coverage if the care ordered by their doctors meets Medicare criteria: 1 Alzheimer’s Disease 2 Mental Illness 3 Multiple Sclerosis 4 Parkinson’s Disease
What is covered by Medicare?
Coverage includes certain hospital, nursing home, home health, physician, and community-based services. The health care services do not have to be related to the individual’s disability in order to be covered.
How long do you have to wait to get Medicare?
There is a five month waiting period after a beneficiary is ...
How long do you have to wait to collect Social Security?
There is a five month waiting period after a beneficiary is determined to be disabled before a beneficiary begins to collect Social Security Disability benefits. People with ESRD and ALS, in contrast to persons with other causes of disability, do not have to collect benefits for 24 months in order to be eligible for Medicare.
How long does Medicare coverage last?
Medicare eligibility for working people with disabilities falls into three distinct time frames. The first is the trial work period, which extends for 9 months after a disabled individual obtains a job.
How long does a disabled person have to work to get a job?
The first is the trial work period, which extends for 9 months after a disabled individual obtains a job. The second is the seven-and-three-quarter years (93 months) after the end of the trial work period. Finally, there is an indefinite period following those 93 months.
Is Medicare the primary or secondary payer?
If the individual’s employer has more than 100 employees, it is required to offer health insurance to individuals and spouses with disabilities, and Medicare will be the secondary payer. For smaller employers who offer health insurance to persons with disabilities, Medicare will remain the primary payer. Indefinite Access to Medicare.
How old do you have to be to get Medicare?
A person with a disability who is under 65 years of age may be eligible for Medicare. There are three groups of people eligible for Medicare if they are under the age of 65. The time frame in which each group becomes eligible differs as follows:
What is the best Medicare plan?
We may use a few terms in this piece that can be helpful to understand when selecting the best insurance plan: 1 Deductible: This is an annual amount that a person must spend out of pocket within a certain time period before an insurer starts to fund their treatments. 2 Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%. 3 Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
What is the difference between coinsurance and deductible?
Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%.
How long do you have to wait to get Medicare?
Some people with a disability do not need to wait until they reach the age of 65 to become eligible for Medicare. Those who have collected Social Security disability benefits for 24 months receive automatic enrollment into traditional Medicare, which comprises parts A and B. This article will examine the eligibility of people with a disability ...
Does Medicare Part D include prescriptions?
Part D and Medicare Advantage costs. The coverage from parts A and B does not include prescription drug costs. Coverage for prescribed medication is known as Medicare Part D. A person may wish to include Part D as part of their plan, or they may decide to explore available options through Medicare Advantage.
How long does Medicare Part D last?
A person with a disability who wishes to enroll in either Medicare Part D or an Advantage plan may do so during: the 7-month period that begins 3 months before the 25th month of Social Security disability benefits . the 7-month period that includes the 25th month of disability benefits.
How much is the deductible for Part A?
Most people do not pay a monthly premium for Part A, but they pay a $1,484 deductible for each benefit period. They also pay coinsurance that varies with the length of their hospital stay within the benefit period.
What is SSI disability?
Supplemental Security Income (SSI) Disability & Medicaid coverage. Waiting for a disability status decision and don’t have health insurance. No disability benefits, no health coverage. The Marketplace application and disabilities. More information about health care for people with disabilities.
How long do you have to wait to get Medicare if you get SSDI?
If you get Social Security Disability Income (SSDI), you probably have Medicare or are in a 24-month waiting period before it starts. You have options in either case.
Can I get medicaid if I have SSDI?
You may be able to get Medicaid coverage while you wait. You can apply 2 ways: Create an account or log in to complete an application. Answer “ yes” when asked if you have a disability.
Can I keep my Medicare Marketplace plan?
One exception: If you enrolled in a Marketplace plan before getting Medicare, you can keep your Marketplace plan as supplemental insurance when you enroll in Medicare. But if you do this, you’ll lose any premium tax credits and other savings for your Marketplace plan. Learn about other Medicare supplement options.

Health
Definition
- Definitions of disability can vary from person to person but Medicare guidelines leave no room for interpretation. Someone must be incapacitated for the long term. You will meet disability criteria for Medicare eligibility only if you fall into one of the following three categories.
Prognosis
- Also known as Lou Gehrigs disease, ALS is a debilitating neurologic disease that can lead to muscle atrophy, breathing difficulties and even death. It is estimated that as many as 20,000 Americans have ALS at any one time. The severity and rapid progression of the disease requires a higher level of medical care and services.
Overview
- More than 10 percent of Americans are estimated to have chronic kidney disease, according to the Centers for Disease Control and Prevention. More than 100,000 people go on to develop kidney failure, also referred to as end-stage renal disease, each year. When your kidneys fail, your body cannot filter toxins out of the body. You will require dialysis treatment or a kidney transplan…
Results
- Your coverage benefits begin three months after you start dialysis treatment. If you get a kidney transplant, Medicare coverage may not be long term. The program will provide coverage for 36 months after a Medicare-approved transplant. After that, if your new kidney remains functional, you will no longer be eligible for Medicare, and you will lose your coverage. You are not eligible f…
Qualification
- A number of other medical conditions can qualify as disabilities. In order to be recognized as Medicare eligible, the person must have gone through the rigorous application process of applying for Social Security Disability Insurance. This process alone can take several months to complete.
Effects
- This assures the government that the disability is severe enough to warrant Medicare coverage. The Social Security Administration reported that 8,939 disabled workers received disability benefits in April 2015.